| disease | Temporomandibular Joint Dislocation |
| alias | Dislocation of the Temporo-mandibular Joint |
When the mandibular condyle moves beyond its normal limit, dislocates from the glenoid fossa, and cannot return to its original position on its own, it is called temporomandibular dislocation. Clinically, anterior dislocation is most common and can occur unilaterally or bilaterally.
bubble_chart Etiology
Anterior dislocation of the temporomandibular joint often occurs due to sudden excessive mouth opening, such as during laughter or yawning, or from prolonged mouth opening, as in oropharyngeal examinations or surgeries where excessive use of a mouth gag causes the condyle to dislocate from the glenoid fossa and shift anterior to the joint structure.
bubble_chart Clinical Manifestations
The patient exhibits abnormal mandibular movement, remaining in an open position and unable to close. Speech is unclear, with drooling and difficulty in chewing and swallowing. The mandible protrudes forward, the chin shifts downward, and the facial shape appears elongated. Upon palpation, a depression can be felt in front of the tragus. In cases of unilateral anterior dislocation, the mandible slightly protrudes forward, and the midline of the chin deviates toward the unaffected side.
1. Dislocation side: It can be either unilateral or bilateral dislocation.
2. Time characteristics of dislocation: When the patient seeks medical attention, they are in a state of dislocation of the temporomandibular joint. If the dislocation occurred within two weeks, it is termed acute dislocation; if it exceeds two weeks, it is called protracted dislocation (chronic dislocation); recurrent dislocations are referred to as habitual dislocation.
3. Direction of dislocation: Due to the bony constraints formed by the articular fossa above and behind, anterior dislocation is the most common. Dislocations in other directions only occur when external force is applied to the mandible along with a temporal fracture. The mandible functions as a single unit, with both joints operating as an integrated system. The medial displacement restriction of one joint also helps prevent outward dislocation of the contralateral joint. Therefore, outward dislocation of the joint only occurs when the opposite side is accompanied by a condylar cervical fracture.4. Symptoms and signs of dislocation: In anterior dislocation, the condylar process shifts anteriorly and superiorly to the articular eminence, presenting as a visibly and palpably distinct triangular depression between the tragus and the lateral ridge of the temporomandibular fossa. In unilateral dislocation, the mandible protrudes and deviates to the opposite side, with possible premature contact of the posterior teeth on the affected side and an open bite in the remaining teeth, while the chin midline shifts to the opposite side. In bilateral dislocation, bilateral posterior teeth may exhibit premature contact, with an open bite in the remaining teeth, mandibular protrusion, anterior crossbite, and facial elongation. Other accompanying symptoms include restricted mouth opening and closing, pain in the affected joint area and face, inability to chew, and impaired swallowing, speech, and facial expressions. Therefore, dislocation of the temporomandibular joint should be regarded as a dental emergency.
Anterior dislocation without fracture can be diagnosed clinically alone. Dislocations in other directions are often accompanied by fractures and require confirmation via X-ray examination.
The treatment principle is to perform manual reduction as early as possible and restrict mandibular movement for about two weeks.
The procedure for manual reduction: The patient sits in a low position with the head resting against the back of a chair or a wall, ensuring that the occlusal plane of the mandibular teeth is lower than the surgeon's elbow joint when the arms are hanging down. The surgeon stands in front of the patient, placing both thumbs (which may be wrapped with gauze) backward on the occlusal surfaces of the mandibular molars on both sides, while the remaining fingers grasp the mandibular body. During reduction, the patient is instructed to relax the muscles. The surgeon gradually applies downward pressure on the posterior part of the mandibular body with both thumbs, while slightly lifting the chin upward with the other fingers. When the condylar process descends below the plane of the articular eminence, the mandible is pushed backward, allowing the condylar process to slide back into the glenoid fossa for reduction (Figure 1). After reduction, immediate fixation with a head-jaw bandage is applied to restrict mouth opening for about two weeks.
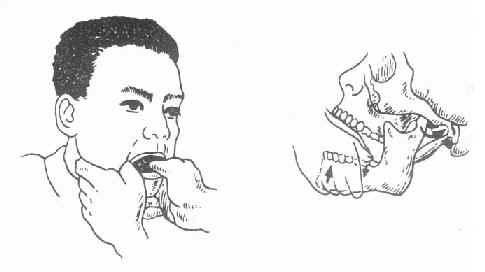
Figure 1: Reduction technique for anterior dislocation of the temporomandibular joint
Before reduction, efforts should be made to alleviate the patient's anxiety. Sometimes, massage of the temporal and masseter muscles or infiltration anesthesia with 1-2% procaine around the temporomandibular joint or the mandibular branch of the trigeminal nerve may assist in reduction. For chronic dislocations, reduction under general anesthesia or even surgical open reduction may be necessary.






