| disease | Acute Suppurative Parotitis |
| alias | Acute Purulent Parotitis |
Acute purulent parotitis, also known as postoperative parotitis, was commonly seen after major abdominal surgeries in the past and was considered one of the serious complications. Due to advancements in antibiotic use and the emphasis on maintaining normal fluid intake and output as well as water and electrolyte balance, it is now rarely encountered. However, acute inflammation of the parotid gland can still be observed in patients under other circumstances.
bubble_chart Etiology
Acute suppurative parotitis is relatively rare. It is caused by pyogenic pathogens, with Staphylococcus aureus being the most common causative bacterium. It often occurs as a complication in patients with severe illnesses (such as acute pestilence) or after major surgeries.
Normally, the parotid gland secretes a large amount of saliva, which is discharged into the oral cavity through the parotid duct, aiding digestion and providing a self-cleaning effect. In critically ill or debilitated patients, such as those in the late stage [third stage] of acute pestilence or after major thoracic or abdominal surgeries, the body's resistance declines, and both systemic and oral immunity weaken. Salivary secretion dysfunction occurs, allowing pathogenic bacteria to enter the gland retrograde through the parotid duct, leading to acute suppurative parotitis. Additionally, trauma, the spread of surrounding tissue inflammation, sialolithiasis, or scar contracture affecting salivary excretion can also cause this condition.
bubble_chart Clinical Manifestations
The onset is abrupt. Most patients experience systemic symptoms such as high fever, shivering, general malaise, and leukocytosis. In a few patients, due to physical exhaustion, the aforementioned systemic reactions may not be apparent.
Acute suppurative parotitis mostly occurs on one side. The affected parotid area shows obvious redness and swelling, the mandibular posterior fossa disappears, and the earlobe tilts upward. Due to the dense parotid membrane, the swelling is constrained, and the internal pressure increases, resulting in severe pain and obvious tenderness upon palpation. There is varying degrees of restricted mouth opening. The opening of the parotid duct on the affected side is red and swollen, with purulent discharge. Because the fascia membrane separates the abscess, it often consists of multiple, scattered small foci of pus, so there is no typical fluctuation sensation in the early stage.During diagnosis, attention should be paid to differentiating it from epidemic parotitis. The latter is a pestilence caused by a virus. It is more common in children, with a history of pestilence contact, and is often bilateral. There is no purulent discharge at the opening of the parotid duct. The total white blood cell count is not elevated, and the proportion of lymphocytes in the differential count is increased.
1. History: There may be a history of systemic infection or fever caused by pestilence, fasting after major surgery, dehydration, or systemic chronic wasting diseases, as well as systemic and local parotid manifestations of acute infection.
2. Clinical Manifestations:
(1) Acute parotid swelling may occur unilaterally or bilaterally, either simultaneously or sequentially, accompanied by distending pain or persistent throbbing pain, limited mouth opening, systemic fever, and malaise.
(2) Local manifestations include parotid swelling centered around the earlobe, skin redness, increased skin temperature, and marked tenderness. Due to the dense parotid membrane, the swelling feels firm on palpation.
(3) The opening of the parotid duct in the mouth appears red and swollen, with reduced secretion. In the late stage [third stage] of the disease, squeezing the parotid gland may yield thick, yellowish purulent discharge.(4) Since the parotid gland is lobulated, abscess formation may present as multifocal, i.e., multiple scattered abscesses. Additionally, due to the tough parotid fascia, fluctuation is rarely palpable even if an abscess forms (clinical diagnosis is mainly based on the disease course, systemic toxic reactions, and local aspiration of pus for confirmation).
(5) In patients with poor systemic conditions, acute infection may spread to adjacent tissue spaces, manifesting as clinical signs of cellulitis in the corresponding spaces. In the late stage [third stage] of the disease, abscesses may perforate the parotid fascia and adjacent tissues, leading to pus discharge through the external auditory canal or the formation of subcutaneous abscesses in the retromandibular or mandibular angle regions.
bubble_chart Treatment Measures
Although this disease is rare, it is often severe and requires active prevention. For critically ill patients and those after major surgery, special attention should be paid to oral care, maintaining oral hygiene, encouraging chewing movements, and providing acidic beverages or foods to stimulate saliva secretion and enhance the flushing and self-cleaning effects.
After the onset of the disease, efforts should be made to improve the overall condition. For severely ill patients with weak constitutions, it is necessary to maintain the body's fluid balance, correct electrolyte disturbances, and, if needed, administer small amounts of fresh blood to boost the body's resistance. High-dose antibiotics should be promptly selected to control infection, along with oral and topical Chinese herbal medicine. If an abscess forms, incision and drainage are required. During the incision, care must be taken to avoid injury to the facial nerve. Typically, an incision is made in front of the tragus, cutting through the skin and subcutaneous tissue to expose the parotid gland. A small vascular clamp is used to perform blunt dissection along the course of the facial nerve, with multiple drainage sites created for scattered small abscesses (Figure 1).
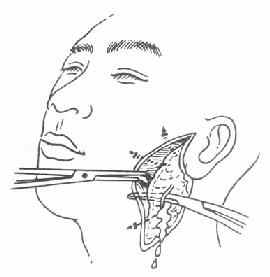
Figure 1 Incision and drainage of acute suppurative parotitis.
1. Mumps Mostly occurs in children, with a history of epidemic contact, often involving both parotid glands. The parotid gland is swollen but with mild pain, the duct orifice is not red or swollen, and the saliva secretion is clear without pus. The total white blood cell count in peripheral blood does not increase, but the lymphocyte ratio rises. The parotid gland does not form an abscess and usually recovers within 7-10 days.
2. Masseteric Space Infection Primarily caused by odontogenic infection, manifested as swelling and tenderness centered around the mandibular angle, with significant limitation of mouth opening. However, the parotid duct orifice is not red or swollen, and the secretion is clear. If an abscess forms, a deep fluctuation can be palpated.
3. Parotid Lymphadenitis Also known as pseudoparotitis, it presents as localized swelling and pain in the parotid region. The lesion does not match the anatomical shape of the parotid gland, the duct orifice is not red or swollen, and the saliva secretion is clear.




