| disease | Congenital Vertebral Malformation |
Congenital vertebral malformations are caused by incomplete segmentation or formation during the embryonic development of the vertebral body.
bubble_chart Etiology
Congenital vertebral malformations are generally considered to be related to autosomal dominant and recessive inheritance. Winter reported that 1% of cases have a family history.
bubble_chart Pathological Changes
Depending on the vertebral anomalies, they can generally be classified into vertebral segmentation defects and vertebral formation defects.
1. Vertebral Segmentation Defects Based on Winter's observations, they are divided into the following four types:
(1)Lateral Unsegmented Bar The segmentation defect occurs on one side, ultimately leading to severe scoliosis (Figure 1).

Figure 1 Vertebral Segmentation Defect (Lateral Unsegmented Bar)
(2)Anterior Unsegmented Bar The anterior part of the vertebra fails to segment, resulting in kyphosis (Figure 2).

Figure 2 Vertebral Segmentation Defect (Anterior Unsegmented Bar)
(3)Posterior Bilateral Unsegmented Bar Leads to kyphosis (Figure 3).

Figure 3 Vertebral Segmentation Defect (Posterior Bilateral Unsegmented Bar)
(4)Symmetric Bilateral Unsegmented Bar The vertebral longitudinal axis does not grow, and no angular or rotational deformity occurs (Figure 4).

Figure 4 Vertebral Segmentation Defect (Bilateral Unsegmented Bar)
2. Vertebral Formation Defects It can be partial or complete. In partial unilateral vertebral formation defects, the vertebra appears wedge-shaped or rhomboid. On X-rays, it presents as a small hypoplastic vertebra. A hemivertebra is caused by complete unilateral formation failure. A hemivertebra may be unsegmented, semi-segmented, or segmented with adjacent vertebrae. Segmented hemivertebrae lead to asymmetric vertebral growth, especially when two hemivertebrae occur on one side, resulting in severe scoliosis (Figure 5). When a hemivertebra occurs posteriorly, it causes angular kyphosis (Figure 6). Semi-segmented hemivertebrae fuse with one adjacent vertebra, resulting in relatively milder scoliosis. Unsegmented hemivertebrae fuse with two adjacent vertebrae and generally do not cause progressive scoliosis (Figure 7). According to Nasca's report on 60 cases of hemivertebrae, they are classified into 6 types: ① Simple supernumerary hemivertebra: May fuse with one or two adjacent vertebrae. When occurring in the thoracic spine, it may have pedicles and supernumerary ribs. ② Simple wedge-shaped hemivertebra. ③ Multiple hemivertebrae. ④ Multiple hemivertebrae with unilateral vertebral fusion. ⑤ Balanced hemivertebrae: Equal numbers of hemivertebrae on both sides, usually not causing scoliosis. ⑥ Posterior hemivertebra: Prone to causing kyphosis (Figure 8).

Figure 5 A. A hemivertebra with mild scoliosis B. Two hemivertebrae on one side causing severe scoliosis
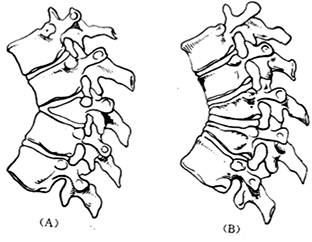
Figure 6 Anterior vertebral formation deficiency (A) One hemivertebra at the posterior of the vertebral body (B) Two hemivertebrae at the posterior of the vertebral body

Figure 7 (A) Semi-segmented hemivertebra (B) Non-segmented hemivertebra
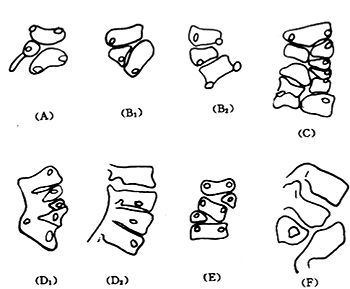
Figure 8 Nasca classification (A) Single-line supernumerary hemivertebra (B) Simple wedge-shaped hemivertebra (C) Multiple hemivertebrae (D) Multiple hemivertebrae with unilateral vertebral fusion (E) Balanced hemivertebra (F) Posterior hemivertebra
bubble_chart Clinical Manifestations
In vertebral anomalies, hemivertebrae are the most common, and the majority of congenital scoliosis cases are caused by hemivertebrae. The progression of spinal deformities varies depending on the vertebral pathology, leading to differing degrees of deformity development. Nasca reported that the progression rate of scoliosis ranges from 1° to 33° per year, with an average of 4°. Generally, the following points should be noted:
1. Specificity of the deformity: Unilateral unsegmented cases progress rapidly, and deformities in the thoracic spine also develop more quickly. Additionally, hemivertebrae tend to progress rapidly during the peak growth period of adolescence (ages 11–19), requiring close monitoring.
2. Extent of spinal involvement: Deformities in the cervicothoracic and lumbar regions progress more slowly than those in the thoracic region. Due to head and neck tilt and shoulder lowering, the visible deformity may appear less severe. In the lumbar region, unless pelvic tilt decompensates, it generally does not cause noticeable deformity. In congenital scoliosis, the more posterior the hemivertebra is located, the more severe the kyphoscoliosis and the worse the prognosis.
bubble_chart DiagnosisRecord the patient's height in detail, including standing and sitting height, the degree of thoracic and lumbar rotation and scoliosis, and the results of the lower limb neurological examination. Note any associated anomalies such as congenital heart disease, Sprengel deformity, cleft palate, etc. X-rays can determine the type of vertebral deformity and should include full-length anteroposterior and lateral spine films to estimate the potential correction angle during surgery. Patients with neurological symptoms must undergo myelography, and MRI should be performed if available to rule out diastematomyelia or tethered cord syndrome.
bubble_chart Treatment Measures
1. Non-surgical therapy: The Milwaukee brace can prevent the progression of long-segment flexible scoliosis but is less effective for short-segment and rigid cases. X-rays taken in both traction and natural states can measure the flexibility of the spinal curvature. During brace wear, the angles of the primary and compensatory curves should be recorded to monitor progression. If the curvature significantly worsens during bracing, surgical treatment should be considered. Bracing is not recommended for curves exceeding 50°.
2. Surgical treatment: The surgical approach is determined by the type and severity of the spinal deformity, the progression rate of scoliosis, the location of the deformity, and the patient's age.
(1) **In situ posterior spinal fusion**: Suitable for mild to Grade II spinal deformities with acceptable appearance and slow progression, particularly in cases of unilateral unsegmented vertebrae. The optimal timing for surgery is before 5 years of age to better control deformity progression. Autologous iliac bone can be used as the graft source, and the fusion range should include two normal vertebrae above and below the affected segment.
(2) **Unilateral vertebral epiphyseal fixation**: Fusion is performed on the anterior and posterior aspects of the convex side to inhibit overgrowth, allowing the concave side to continue growing for corrective purposes. This procedure is not suitable for patients with excessive kyphosis.(3) **Scoliosis correction and fusion**: Suitable for severe spinal deformities. Preoperative spinal traction is necessary to prevent sudden spinal elongation during surgery, which may cause spinal cord injury. Internal fixation methods such as Harrington rods or Luque rods can be used for correction.
(4) **Hemivertebra resection**: Indicated for spinal tilt and decompensation caused by lumbosacral junction abnormalities. Early surgery is recommended to prevent secondary bony changes. After hemivertebra resection, compression rods are used for fixation. If accompanied by incomplete spinal cord or neural tube defects (e.g., diastematomyelia or amenorrhea), a preliminary convex-side hemifusion between the lumbar and sacral 1 vertebrae may be performed first.
(5) **Spinal osteotomy**: Suitable for older or adolescent patients with unilateral unsegmented vertebrae, rigid deformities, or severe angular scoliosis. If rib fusion is present on the convex side, it should be excised during surgery. A wedge osteotomy and fusion are performed via an anterior spinal approach. This procedure is technically demanding and should be performed by experienced spinal deformity surgeons. Due to the high risk of spinal cord {|injury|}, the risks must be clearly explained to the patient and family preoperatively.




