| disease | Oral Lichen Planus |
| alias | Lichen Planus |
Lichen planus is a chronic inflammatory condition of the skin and mucous membranes. It can occur solely in the oral cavity or on the skin, or affect both simultaneously. Besides the oral cavity, lesions may also appear on the genitals, fingernails, and/or toenails, though these cases are relatively rare. Middle-aged women are more commonly affected, but some reports indicate no significant gender difference.
bubble_chart Etiology
The cause of lichen planus is unknown, but clinical and basic research has identified many related factors. Currently, it is generally believed that the onset may be associated with neuropsychiatric disorders, viral infections, or autoimmune reactions. Some reports indicate familial cases, but whether there is a genetic link remains unconfirmed. The use of drugs such as streptomycin, isoniazid, chlorpropamide, and tolbutamide may induce lichen planus-like rashes or exacerbate the condition.
bubble_chart Pathological Changes
The microscopic findings of oral mucosal and skin lesions are essentially the same and can be summarized as follows: hyperkeratosis and parakeratosis, accompanied by thickening of the granular layer, necrosis and liquefaction degeneration of basal cells, and a large number of lymphocyte infiltrations beneath the basement membrane. Additionally, round eosinophilic colloid bodies (Givatte bodies, Civatte bodies) may sometimes be observed in the spinous layer, basal layer, or connective tissue. These bodies are smaller than spinous cells, but colloid bodies can also be seen in various diseases such as discoid lupus erythematosus. Under electron microscopy, the desmosomes and hemidesmosomes of basal cells show degeneration and loosening, leading to extensive inflammatory cell infiltration and the formation of subepithelial blisters in the spaces created by the separation of basal cells from the basement membrane. The degenerated desmosomes may become antigens and trigger autoimmune reactions, which is why direct immunofluorescence examination sometimes reveals fluorescence in the basement membrane zone caused by the deposition of immune complexes. Furthermore, changes in the basement membrane can be observed: irregularity, thickening, fragmentation, and reformation. The fragmentation of the basement membrane allows inflammatory cells to enter the spinous layer, where the colloid bodies may represent degenerated or dead epithelial cells phagocytosed by macrophages.
bubble_chart Clinical Manifestations1. Skin lesions Lichen planus is one of many lichenoid skin diseases. The characteristic lesions are flat, shiny, pale purple-red, polygonal papules, about the size of a mung bean, with clearly defined borders, firm and dry texture, and a lichenoid appearance when fused. The affected area is rough, with visible skin folds between the papules, and scratch marks due to cutaneous pruritus. Applying paraffin oil to the surface of the papules and observing under a magnifying glass reveals fine white streaks, known as Wickham's striae. The treatment efficacy for skin lesions is generally better than that for mucous membrane lesions.
2. Nail and (or) toenail lesions These often appear symmetrically, but it is rare for all ten fingers (or toes) to be affected simultaneously. The nail plate becomes thin and loses its luster, showing indentation upon pressure. Sometimes, tiny red pinpoint dots appear on the nail bed, causing pain upon pressure. The nail surface may exhibit fine scaling, longitudinal grooves, pits, or a planed appearance (as if a layer has been shaved off with a sharp blade). Severe nail or toenail damage can lead to nail plate detachment or even ulcerative necrosis. In some cases, alopecia areata may occur alongside nail lesions.
3. Oral mucous membrane lesions The main feature is pearly white streaks. These streaks can extend in various directions, forming a dense network when numerous or appearing as branching patterns when sparse. They may also appear as single lines or rings. Although the patterns vary, classification holds little clinical significance. The lesions are often bilaterally symmetrical, with the mucous membrane remaining soft and elastic but feeling rough, accompanied by grade I irritation pain.
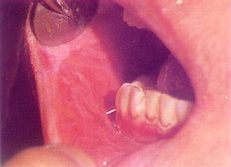
Color Figure 1 Buccal lichen planus
(2) Papules: Needle-sized, slightly raised, occasionally seen on the buccal mucosa alongside white streaks but should not be confused with Fordyce disease, as both can coexist. Ectopic sebaceous glands appear as pale yellow granules, clustered or scattered, mostly hidden beneath the mucosa and asymptomatic. The vermilion border is also a common site for ectopic sebaceous glands, more frequently on the upper lip than the lower.
(3) Patches: Mostly round or oval, often located on the mid or lateral dorsum of the tongue, usually symmetrical but sometimes unilateral. The papillae in the affected area disappear, leaving a flat surface. Square patches are occasionally seen on the buccal mucosa or attached gingiva in smokers, actually representing a rare form of leukoplakia, which gradually disappears after quitting smoking, with white streaks reappearing. (Color Figure 2)
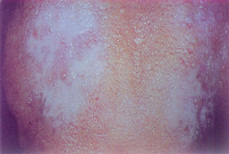
Color Figure 2 Dorsal tongue lichen planus
(4) Blisters: Typically the size of foxtail millet, most commonly found on the soft palate but may occur elsewhere. The blisters rupture easily and reappear within a day.
(5) Erosion: The erosive type is common, with a relatively extensive range that can almost involve the entire oral mucosa. Although faint white striae-like lesions may still be vaguely visible in some areas, the lack of typical manifestations means it cannot provide a clinical basis for diagnosis. Erosions on the attached gingiva often show remnants of blister walls, resembling "epithelial desquamation." This desquamative clinical presentation can be seen in various inflammatory diseases (such as pemphigus, pemphigoid, etc.), hence the former term "desquamative gingivitis," which is no longer considered an independent disease. This type often shows resistance to antibiotics and immunosuppressive therapy, necessitating comprehensive systemic examinations to avoid delays in diagnosis and treatment. (Color Figure 3)

Color Figure 3 Gingival Lichen Planus
4. Genital Mucosal Lesions Often appear as dark red round or oval patches, with visible white reticular lesions on the surface, prone to erosion.
bubble_chart Treatment Measures
There is currently no perfect mental therapeutics. It is essential to eliminate mental stress, treat chronic sexually transmitted disease foci, and strive for a regular lifestyle.
1. Based on medical history, clinical and laboratory examination results, treatment should target relevant factors: For lesions without erosion and with limited scope, consider alternating rinses with 2–4% sodium bicarbonate solution and 0.2% chlorhexidine solution several times a day. Review monthly, focusing on high-risk areas.
2. Remove mechanical irritants, such as scraping tartar from the buccal surfaces of molars. To avoid damaging the mucosal area with toothbrush bristles, it is best to use cotton swabs for cleaning instead of brushing.
3. For localized erosions, sprinkle compound steroid powder several times a day. If symptoms are pronounced, local injections of triamcinolone acetonide may be administered twice weekly, along with or without antibiotics. For the vermilion border, fluocinolone acetonide can be applied, but if crusts are present, wet compresses should be used first until the crusts fall off, followed by a thin layer of ointment several times daily.
4. Systemic use of adrenal corticosteroids should be approached cautiously, as the effects are not ideal. A low-dose, short-term regimen may be tried, such as prednisone 15mg daily in three divided doses for about 1–2 weeks. During medication, stool occult blood and blood pressure should be monitored.
Local injections of adrenal corticosteroids are more effective than systemic use. Alternatively, Tripterygium hypoglaucum or Root Leaf or Flower of Common Threewingnut tablets may be taken orally.
Tripterygium hypoglaucum and Root Leaf or Flower of Common Threewingnut belong to the same family (Celastraceae) and are suitable for connective tissue and autoimmune diseases such as lupus erythematosus. The former inhibits delayed-type hypersensitivity, reduces capillary permeability, alleviates edema, and strongly suppresses inflammatory proliferation. Higher doses may inhibit specific antibody production, with mild side effects such as occasional nausea, abdominal distension, rash, leukopenia, and thrombocytopenia. However, Root Leaf or Flower of Common Threewingnut is highly toxic, primarily affecting the heart, and is contraindicated in unmarried or married but childless male patients and pregnant women.
The usual doses are: Tripterygium hypoglaucum, 2 tablets three times daily; Root Leaf or Flower of Common Threewingnut, 3–4 tablets twice daily.
5. Local antifungal treatment may aid in symptom improvement.
6. Oral vitamin A or retinoic acid
Take vitamin A orally, 50,000 U daily, or retinoic acid 35–50mg/day. Initial use may cause headache or dizziness, in which case the dose should be reduced. Tolerance usually develops within a few days. From weeks 2–3, gradually increase to 30–60mg daily in three divided doses, with a treatment course of about 1–2 months. Common side effects include dry lips and alopecia areata. Contraindicated in patients with coronary heart disease, liver or kidney dysfunction, or hyperlipidemia.
0.2% retinoic acid solution is suitable for topical application but not for lesions with congestion or erosion. Before application, dry the saliva and use a fine brush to apply a small amount along the white area, avoiding the vermilion mucosa. Ointment formulations are unsuitable as they do not adhere well to moist oral mucosa. Newer formulations like isotretinoin and arotinoid function similarly to retinoic acid, with the main advantages of lower doses (0.5mg/kg daily), reduced toxicity, and fewer side effects (e.g., dry lips, alopecia areata), though they are teratogenic.
In recent years, there have been reports of malignant transformation of this disease, with a malignancy rate of about 1%, which meets the diagnostic criteria for precancerous conditions. Lesions with long-term congestion and erosion that do not heal should be closely monitored, and biopsies should be performed promptly.
Lichen planus should be differentiated from the following diseases:
1. Oral erythroplakia (referred to as erythroplakia or oral red patch) Erythroplakia is a red oral mucosal precancerous lesion, very similar to precancerous dermatitis—Bowen disease. The histopathological changes of the two are often difficult to distinguish. To avoid confusion with benign inflammatory erythema (macule) in terminology, it is called erythroplakia to emphasize their fundamental differences.
Erythroplakia commonly occurs in "danger zones": the ventral (margin) of the tongue—floor of the mouth, the buccal mucosa in the commissure area, and the soft palate complex. It is more prevalent in middle-aged women than in men. The initial stage [first stage] of erythroplakia is characterized by epithelial atrophy and dysplasia. Clinically, it presents as a bright blood-red, smooth, "skinless" round or oval patch with very clear boundaries. On palpation, it feels very soft, resembling "velvet," and the lesion may be slightly depressed or flat. There is no significant pain or discomfort. The lesion, about the size of a mung bean, gradually expands outward. This type, with a bright red surface and no white components, is called homogeneous erythroplakia. Conversely, if white granules are present within the erythroplakia, it is termed granular erythroplakia. If larger nodules accompany the granules, it is called granular-nodular erythroplakia. Since this type involves two precancerous lesions—erythroplakia and leukoplakia—it may also be referred to as granular-nodular leukoplakia (see the section on leukoplakia).
During the slow expansion of erythroplakia, its clinical features include a gradual reduction in softness and blood-red color, blurred boundaries, and grade I surface elevation. Palpation reveals a tough texture, indicating that the erythroplakia has progressed from the atrophy and dysplasia stage to carcinoma in situ or invasive carcinoma. Hence, it is sometimes called "proliferative erythroplakia" or "erythroplasia," and a biopsy should be performed immediately for definitive diagnosis.
The initial stage [first stage] of erythroplakia is marked by epithelial atrophy, so microscopic examination shows: disappearance or indistinctness of the keratin layer, with only 2–3 layers of spinous cells in the papillary layer. These spinous cells often exhibit precancerous cellular abnormalities, such as altered nuclear-to-cytoplasmic ratios and hyperchromatic nuclei. Additionally, due to the proximity of the papillary layer to the surface and capillary dilation and congestion, the lesion appears distinctly blood-red and soft.
Common mucositis is a general term for benign red mucosal inflammation. Various causes, such as trauma, infection, or drug rash, can induce inflammatory reactions in any part of the oral cavity. This inflammatory reaction is also commonly referred to as erythema. Erythema appears dark red, lacks the distinctive blood-red color, and is often accompanied by noticeable pain and a short course. For localized lesions suspected to be erythroplakia, corticosteroids such as triamcinolone can be injected beneath the lesion twice weekly. If no signs of regression appear within two weeks, a biopsy should be performed.
2. Discoid lupus erythematosus More common in women, lesions often occur on the lips, buccal mucosa, dorsal tongue, floor of the mouth, and ventral tongue. Skin lesions are frequently seen on the face and scalp. The mucosal lesions are characterized by central atrophy surrounded by white or yellowish-white, hardened patches with irregular but clearly defined edges. The location of the lesions can serve as a reference for differentiation.
The differentiation between the above diseases and lichen planus can also be aided by histological examination: - Erythroplakia lesions show disappearance of the keratin layer, only 2–3 layers of spinous cells, altered nuclear-to-cytoplasmic ratios, and hyperchromatic nuclei. - Lupus erythematosus lesions exhibit hyperkeratosis but insignificant epithelial hyperplasia. - Leukoplakia shows obvious epithelial dysplasia. - Lichen planus presents with hyperkeratosis or parakeratosis, sometimes atrophy, disordered arrangement, liquefaction, or necrosis of basal cells, and dense lymphocytic infiltration beneath the basement membrane.





