| disease | Thumb Reconstruction |
The thumb can abduct, oppose, and accurately and powerfully perform grasping and pinching actions in opposition to the other fingers. The thumb accounts for approximately 40% of hand function. The loss of the thumb will severely affect hand function. Therefore, how to reconstruct the thumb and restore its function after thumb injury is an important topic in hand surgery. Proper management of acute thumb trauma is key to preserving function. In cases of traumatic thumb amputation, thumb replantation should be the first priority. If replantation is not feasible, thumb reconstruction can be achieved through nerve anastomosis and tube pedicle embedding. This involves removing the skin and nail of the amputated finger, preserving the bilateral digital nerves and tendons, cross-fixing the bones with Kirschner wires, anastomosing the nerves and tendons, embedding a subclavian tube pedicle, and severing the pedicle after 3-4 weeks. This method can create a thumb with good sensation. Increasingly, people are using the nail flap for emergency thumb reconstruction, achieving satisfactory results.
bubble_chart Treatment Measures
Depending on the extent of the defect and functional requirements, different reconstruction methods can be chosen.
(1) Interphalangeal joint defect (Grade I defect) - Partial function of the thumb is still retained, and unless required by a specific occupation, generally no treatment is necessary.
(2) Mid-segment defect of the proximal phalanx - The preserved thumb length is relatively short, significantly affecting function. The following methods can be chosen to improve thumb function.
1. Purlicue deepening procedure - Can relatively lengthen the thumb. The method involves a Z-shaped incision of the purlicue skin, cutting the contracted adductor pollicis muscle band, and if necessary, transferring the dorsal skin flap of the index finger to deepen the purlicue.
2. Cap-shaped flap elevation method - Also known as the degloving bone grafting technique. Suitable for cases where 1/2 or 1/3 of the proximal phalanx remains and the skin at the thumb stump is very loose. Method: Circumferentially incise the skin 3-4 cm proximal to the stump, free the nerves and arteries/veins proximally. Fully free the distal flap to form a cap-shaped flap, perform bone grafting at the fingertip, elevate the cap-shaped flap to cover the bone end, and graft skin to repair the proximal wound (Figure 1). This method can lengthen the thumb by about 1-1.5 cm.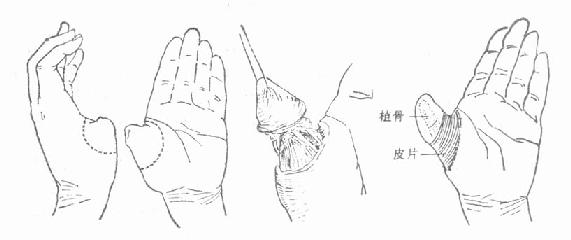
Figure 1 Cap-shaped flap elevation bone grafting method
3. First metacarpal lengthening procedure - Surgically expose the first metacarpal shaft, cut the metacarpal under the bone membrane and embed a bone graft to lengthen the metacarpal. Alternatively, after cutting the metacarpal, install a spreader, close the wound, and gradually spread to lengthen the metacarpal, with secondary bone grafting.
4. Partial free transplantation of the second toe using the metatarsal base stirred pulse as the blood supply stirred pulse for thumb reconstruction. This method provides satisfactory appearance and function.
(3) Metacarpophalangeal joint or partial metacarpal defect (Grade II-III defect)
The thumb is completely absent, only the first metacarpal or part of the metacarpal remains, with partial or complete thenar function. Depending on the specific situation, the following methods can be chosen:
1. Transfer of a neighboring residual finger for thumb reconstruction - Utilizing a neighboring residual finger with little function for thumb reconstruction should be the preferred method. The transferred residual finger should have good circulation and sensation, with uninjured nerves and vessels. Design to use a residual finger of appropriate length, along with tendons, nerves, stirred pulse, veins, and surrounding soft tissues, and transfer it to the first metacarpal. Fix the bones in opposition with crossed Kirschner wires, enabling contact with the fingertips of other fingers (Figure 2). This method does not require cutting nerves and vessels, resulting in a thumb with good sensory and motor function and a satisfactory appearance.
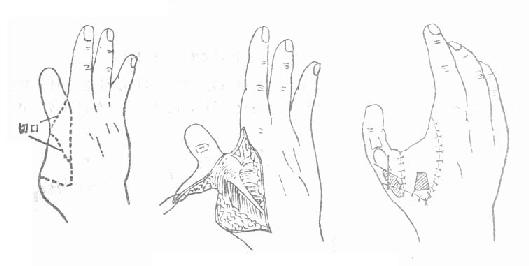
Figure 2 Transfer of a neighboring residual finger for thumb reconstruction
2. Free transplantation of the second toe for thumb reconstruction - First used by Yang Dongyue et al. in China in 1966, it provides a relatively ideal new method for thumb reconstruction. This method can add a finger and is suitable for Grade II and III thumb defects, especially those accompanied by the absence of more than two fingers. Additionally, this method can also be used for finger reconstruction in cases of four-finger absence. Free transplantation of the second toe can also provide fingers for hand reconstruction.
The second toe is relatively long and similar in appearance to the thumb. Removal of the second toe and the second metatarsal head has little impact on walking function and appearance. Method: (Figure 3) Incise the skin as shown, free the dorsal stirred pulse, great saphenous vein, toe flexor and extensor tendons, and toe nerves distally and cut them at a high level, disarticulate the metatarsophalangeal joint or metatarsal neck, completely free the toe, and transplant it to the thumb site. Fix the bones in opposition with crossed Kirschner wires, and anastomose with the thumb flexor and extensor tendons, digital nerves, and radial stirred pulse and cephalic vein, completing the reconstruction surgery in one session. The reconstructed thumb not only has a good appearance but also satisfactory sensory and motor functions, although it requires higher technical skills.
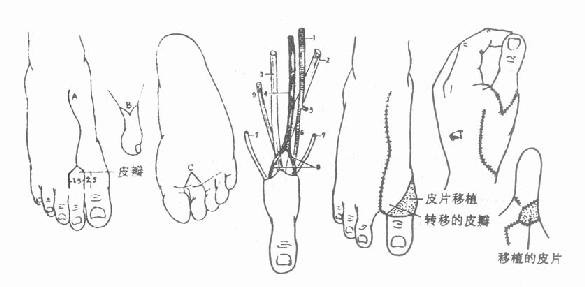
Figure 3 Second toe free transplantation for thumb reconstruction
In recent years, some have used a similar method, employing a free toe nail flap combined with iliac bone grafting to reconstruct the thumb, achieving a thumb with a good appearance, but with a significant impact on foot function.
3. Transfer of a Normal Index Finger for Thumb Reconstruction Also known as index pollicization. For grade II and III thumb defects, if the aforementioned methods for thumb reconstruction cannot be applied, transferring a normal index finger may be considered. The advantage of this method is that it preserves the continuity of nerves, blood vessels, and tendons, making it easier to succeed, and the reconstructed thumb has good sensory and motor functions. The drawback is that it uses a normal index finger, which comes at a higher cost. The surgical method is the same as the residual finger transfer method, but attention should be paid to the length of the thumb, which should not be too long.4. Thumb Reconstruction Using a Tubed Pedicle Flap and Bone Graft The method involves bone grafting at the residual end of the first metacarpal and covering it with a tubed pedicle flap (such as a subclavian tubed pedicle). The pedicle is severed after 3-4 weeks to form a thumb. Thumbs reconstructed using this method have poor circulation and sensation, often leading to frostbite or burns, and poor functionality. This method is now largely obsolete and is only used in specific cases. To improve sensory function, a neurovascular island flap from the side of the ring finger can be harvested and transferred to the thumb tubed pedicle (usually to the fingertip and ulnar side), providing good sensation to that area (Figure 4).
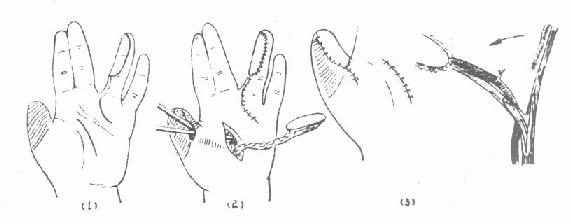
Figure 4: Reconstruction of Thumb Sensation Using a Ring Finger Neurovascular Island Flap




