| disease | Persistent Occiput Posterior, Occiput Transverse Position |
| alias | Persistent Occipitoposterior Position, Persistent Occipitotransverse Position |
Abnormal fetal position is one of the common factors leading to difficult delivery. During childbirth, the occiput anterior position (normal fetal position) accounts for about 90%, while abnormal fetal positions account for about 10%, with the majority being abnormal head positions. These include persistent occiput transverse position and persistent occiput posterior position due to obstructed rotation of the fetal head within the pelvic cavity, as well as face presentation and brow presentation caused by poor flexion of the fetal head, resulting in varying degrees of extension. Other conditions include high straight position and anterior asynclitism, totaling approximately 6–7%. Abnormal fetal lie, such as breech presentation, accounts for about 3–4%, while shoulder presentation is now extremely rare. Additionally, there is compound presentation. During childbirth, the fetal head engages in an occiput posterior or transverse position. As it descends, the occiput of the fetal head, due to strong uterine contractions, can usually rotate forward by 135° or 90° to convert to an occiput anterior position, allowing for natural delivery. If the occipital bone of the fetal head persistently fails to rotate forward and remains in the posterior or lateral part of the maternal pelvis until the late stage of childbirth (third stage), resulting in difficult delivery, it is termed persistent occiput posterior position or persistent occiput transverse position.
bubble_chart Etiology
1. Abnormal pelvis. This often occurs in android or anthropoid pelvises. These two types of pelvises are characterized by a narrower anterior half of the pelvic inlet, which is unsuitable for the engagement of the fetal occiput, while the posterior half is wider, making it easier for the fetal head to engage in an occiput posterior or occiput transverse position. Such pelvises are often accompanied by a narrowed mid-pelvis, which hinders the forward rotation of the fetal head at the mid-pelvic plane, leading to persistent occiput posterior or persistent occiput transverse positions.
2. Poor flexion of the fetal head. If engagement occurs in an occiput posterior position, the fetal spine is close to the maternal spine, which is unfavorable for fetal head flexion. The anterior fontanelle becomes the lowest part of the descending fetal head, and the lowest point often turns toward the anterior pelvis. When the anterior fontanelle rotates to the front or side, the fetal occiput turns to the back or side, forming a persistent occiput posterior or occiput transverse position.3. Other factors. Uterine contractions lacking strength can affect fetal head flexion and internal rotation, easily resulting in persistent occiput posterior or occiput transverse positions. Some scholars have reported a higher incidence of occiput posterior positions with anterior placenta.
The fetal head usually engages in the occiput transverse position. Even if it engages in the occiput posterior position, strong uterine contractions during childbirth can often rotate the occiput forward by 90° to 135°, converting it to an occiput anterior position for spontaneous delivery. If it fails to rotate to the occiput anterior position, the following two mechanisms of childbirth may occur:
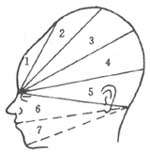
1. Left (Right) Occiput Posterior Position The occiput of the fetal head reaches the mid-pelvis and undergoes internal rotation posteriorly by 45°, aligning the sagittal suture with the anteroposterior diameter of the pelvis. The fetal occiput faces the sacrum, forming a true occiput posterior position. There are two modes of delivery in this case: ① Good flexion of the fetal head: When the head continues to descend until the anterior fontanel reaches beneath the pubic arch, the anterior fontanel serves as the pivot point. The head flexes, allowing the vertex and occiput to emerge over the perineal margin. Subsequently, the head extends, delivering the forehead, nose, mouth, and chin in sequence from beneath the pubic symphysis [Figure 1 (1)]. This is the most common mode of assisted vaginal delivery for occiput posterior positions. ② Poor flexion of the fetal head: When the nasal root appears beneath the pubic symphysis, it serves as the pivot point. The head first flexes, delivering the anterior fontanel, vertex, and occiput over the perineal margin, then extends to deliver the nose, mouth, and chin in sequence from beneath the pubic symphysis [Figure 1 (2)]. Due to the larger occipitofrontal circumference rotating, delivery becomes more difficult, often requiring operative assistance.
|
|
|
|
|
|
(1) Occiput posterior delivery with the anterior fontanel as the pivot point |
(2) Occiput posterior delivery with the nasal root as the pivot point |
Figure 1 Mechanism of occiput posterior childbirth
2. Occiput Transverse Position Some occiput transverse positions do not undergo internal rotation during descent, or the occiput of an occiput posterior position rotates only 45° forward, resulting in a persistent occiput transverse position. Although vaginal delivery is possible with a persistent occiput transverse position, most cases require manual rotation or vacuum extraction to convert the head to an occiput anterior position for delivery.
bubble_chart Clinical Manifestations
In labor, the engagement of the fetal head is delayed, and flexion is poor. Because the presenting part of the occiput posterior position does not easily adhere closely to the cervix and the lower segment of the uterus, it often leads to a lack of strength in coordinated uterine contractions and slow cervical dilation. Due to the persistent pressure of the occipital bone on the rectum in the posterior pelvis, the mother experiences a sensation of rectal distension and the urge to defecate. This can lead to premature use of abdominal pressure before the cervix is fully dilated, easily causing edema of the anterior cervical lip and maternal fatigue, which affects the progress of labor. Persistent occiput posterior position often results in a prolonged second stage of labor. If fetal hair is visible at the vaginal opening but the fetal head does not continue to descend smoothly after multiple contractions with bearing-down efforts, persistent occiput posterior position should be considered.
Effects on the mother: Abnormal fetal position leads to secondary lack of strength in uterine contractions, prolonging labor and often necessitating operative delivery, which increases the risk of soft tissue injury, postpartum metrorrhagia, and infection. Prolonged pressure of the fetal head on the soft birth canal can cause ischemic necrosis and sloughing, resulting in genital tract fistulas.
1. Clinical manifestations: After labor begins, the engagement of the fetal head is delayed, and flexion is poor. Because the presenting part of the occiput posterior position does not easily adhere closely to the cervix and the lower segment of the uterus, it often leads to a lack of strength in coordinated uterine contractions and slow cervical dilation. Due to the continuous pressure of the occipital bone on the rectum in the posterior part of the pelvis, the mother experiences a sensation of anal distension and the urge to defecate. This causes her to bear down prematurely before the cervix is fully dilated, which can easily lead to edema of the anterior cervical lip and maternal fatigue, affecting the progress of labor. Persistent occiput posterior position often results in a prolonged second stage of labor. If fetal hair is visible at the vaginal opening but the fetal head does not continue to descend smoothly after multiple contractions, persistent occiput posterior position should be considered.
2. Abdominal examination: The fetal buttocks can be palpated at the fundus of the uterus, with the fetal back偏向 the mother’s posterior or lateral side, and the fetal limbs can be clearly palpated on the opposite side. If the fetal head has engaged, sometimes the fetal chin can be felt above the pubic symphysis on the side of the fetal limbs. Fetal heart sounds are heard most clearly below the umbilicus and偏向 the外侧. In the occiput posterior position, because the fetal back is extended and the anterior chest is close to the mother’s abdominal wall, the fetal heart can also be heard on the side of the fetal limbs near the fetal chest.
3. Rectal or vaginal examination: During rectal examination, if the cervix is partially dilated or fully dilated and the position is occiput posterior, the posterior part of the pelvis feels empty. The sagittal suture of the fetal head is found to be on the oblique diameter of the pelvis, with the anterior fontanel in the right anterior part of the pelvis and the posterior fontanel (occiput) in the left posterior part, indicating left occiput posterior position. The opposite would indicate right occiput posterior position. If the sagittal suture is on the transverse diameter of the pelvis and the posterior fontanel is on the left side of the pelvis, it is left occiput transverse position; the opposite would indicate right occiput transverse position. If there is fetal head edema, overlapping cranial bones, or unclear palpation of the fontanels, a vaginal examination is needed to determine the fetal position based on the location and direction of the fetal auricle and tragus. If the auricle faces the posterior part of the pelvis, it is diagnosed as occiput posterior position; if the auricle faces the lateral side of the pelvis, it is occiput transverse position.
4. B-ultrasound examination: The position of the fetal head can be accurately determined based on the location of the fetal face and occiput, allowing for a clear diagnosis.
bubble_chart Treatment Measures
1. First Stage of Labor: Closely monitor the progress of labor, paying attention to fetal head descent, cervical dilation, the strength of uterine contractions, and any changes in fetal heart rate. Anticipate a prolonged labor and ensure the mother receives adequate nutrition and rest. Encourage the mother to lie on her side opposite the fetal back to facilitate the rotation of the fetal occiput anteriorly. If uterine contractions are inadequate, initiate intravenous oxytocin infusion as early as possible. Before full cervical dilation, advise the mother to avoid premature pushing to prevent cervical anterior lip edema, which may impede labor progress. If labor shows no significant progress, the fetal head remains high, or signs of fetal distress appear, consider cesarean section to terminate childbirth.
2. Second Stage of Labor: If the second stage progresses slowly—lasting nearly 2 hours for primiparas or 1 hour for multiparas—perform a vaginal examination. If the biparietal diameter of the fetal head has reached the level of the ischial spines or lower, manually rotate the fetal occiput anteriorly to align the sagittal suture with the anteroposterior diameter of the pelvic outlet, allowing for either spontaneous childbirth or assisted vaginal delivery (low forceps or vacuum extraction). If rotating to an occiput anterior position is difficult, rotate posteriorly to an occiput posterior position and then proceed with forceps-assisted delivery. If delivery occurs in an occiput posterior position, perform a generous episiotomy to prevent perineal lacerations. If the fetal head remains high or cephalopelvic disproportion is suspected, proceed with cesarean section; mid-forceps should not be used.
3. Third Stage of Labor: Due to prolonged labor, postpartum uterine atony is more likely to occur. Administer intramuscular uterotonics immediately after placental delivery to prevent postpartum hemorrhage. Repair any lacerations of the soft birth canal promptly. Provide intensive neonatal monitoring. Administer antibiotics postpartum to prevent infection in cases of operative delivery or soft birth canal lacerations.