| disease | Sublingual Space Infection |
Sublingual space infection refers to the acute suppurative infection of the sublingual space. This condition is relatively uncommon, with primary clinical manifestations including swelling in the sublingual caruncle or sublingual sulcus area of the mouth floor, either unilaterally or bilaterally.
bubble_chart Etiology
The sublingual space is located beneath the tongue and the oral floor mucosa, and above the mylohyoid and hyoglossus muscles. Its anterior and lateral boundaries are the medial surfaces of the mandibular body, while its posterior boundary extends to the root of the tongue. The genioglossus and geniohyoid muscles further divide the sublingual space into left and right portions, which communicate with each other deep to the sublingual caruncle. The sublingual space communicates posteriorly and superiorly with the parapharyngeal space and the pterygomandibular space, and {|###|} connects inferiorly with the submandibular space (Figure 2).
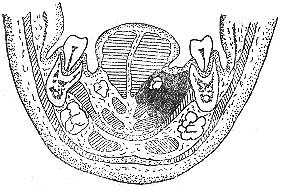
Figure 2: Anatomical location of the sublingual space
Odontogenic infections of mandibular teeth, injuries or ulcers of the oral floor mucosa, as well as inflammation of the sublingual and submandibular gland ducts can all lead to sublingual space infections.
bubble_chart Clinical Manifestations
Swelling occurs in the unilateral or bilateral sublingual caruncle or sublingual sulcus of the floor of the mouth, with mucosal congestion. The tongue is compressed, elevated, and pushed toward the unaffected side, resulting in restricted movement. This leads to varying degrees of difficulty and pain in speech, eating, and swallowing. When the infection spreads to the posterior part of the floor of the mouth, it may cause difficulty in opening the mouth and breathing. Fluctuation can be palpated in the floor of the mouth after abscess formation; if it ruptures spontaneously, pus may discharge. If the infection originates from the salivary glands, pus may be discharged from the submandibular duct orifice. When adjacent spaces are involved, perimandibular and submandibular abscesses may develop, accompanied by corresponding clinical symptoms.
bubble_chart Diagnosis1. Medical History Adults have a history of suppurative periapical periodontitis of mandibular molars and pericoronitis of mandibular wisdom teeth. In infants and children, a history of submandibular lymphadenitis secondary to upper respiratory tract infection can often be elicited.
2. Clinical Manifestations Inflammatory redness, swelling, and tenderness in the submandibular triangle. Initially, it presents as an inflammatory infiltrative mass with tenderness. During the suppurative stage, there is throbbing pain, fluctuation, and skin erythema. Pus is easily aspirated upon puncture. Patients exhibit systemic symptoms such as varying degrees of fever and leukocytosis.
3. Differential Diagnosis Acute suppurative submandibular sialadenitis often occurs as an acute exacerbation of chronic submandibular sialadenitis. It also presents with acute inflammatory signs such as redness, swelling, and tenderness in the submandibular triangle, fever, and leukocytosis. However, it usually does not form a submandibular abscess. Additionally, there is redness and swelling in the sublingual caruncle area and the orifice of the submandibular duct on the affected side, and pressure on the submandibular gland may cause purulent discharge from the duct orifice. X-ray occlusal films of the mouth floor often reveal calculi in the submandibular duct.
bubble_chart Treatment Measures
After the formation of an abscess, an incision is generally made parallel to the mandibular body at the most swollen or fluctuant area of the mouth floor, bluntly separating the mucous membrane to enter the abscess cavity for drainage. Care should be taken to avoid damaging the
tongue spirit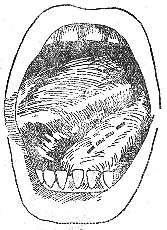 nerve, the
nerve, the stirred pulse
of the tongue, and the submandibular gland duct. For cases where the abscess has already ruptured, simply enlarging the rupture slightly and inserting a drainage strip is sufficient (Figure 1).
Figure 1 Intraoral incision for drainage of sublingual space abscess
Infections in the sublingual space can easily spread to the submandibular space via the posterior border of the mylohyoid muscle along the submandibular gland. Once a submandibular abscess forms, drainage solely from the mouth floor is ineffective, and timely incision and drainage from the submandibular region should be performed.

