| disease | Abnormal Bony Birth Canal |
| alias | Abnormal Fetal Delivery |
A contracted pelvis refers to a condition where the pelvic dimensions are too short or the shape is abnormal, resulting in a pelvic cavity smaller than the limit through which the fetal presenting part can pass. This obstructs the descent of the fetal presenting part and hinders the normal progress of labor. A contracted pelvis may involve one or multiple shortened diameters, or a single or multiple narrowed planes. When one diameter is narrowed, it is necessary to assess the size of other diameters in the same plane, along with a comprehensive analysis of the overall size and shape of the pelvis, to make an accurate diagnosis.
bubble_chart Clinical Manifestations
1. Narrow pelvic inlet plane: This is relatively common among women in our country. Measurements show a sacral external diameter <18 cm, an anteroposterior diameter of the pelvic inlet <10 cm, and a diagonal diameter <11.5 cm. The following two types are commonly seen:
(1) Simple flat pelvis: The pelvic inlet is transversely flattened and oval-shaped, with the sacral promontory protruding forward and downward, shortening the anteroposterior diameter while the transverse diameter remains normal (Figure 7).
Figure 7: Simple flat pelvis
(2) Rickets-induced flat pelvis: Due to childhood rickets causing bone softening and pelvic deformation, the sacral promontory is pushed forward, significantly shortening the anteroposterior diameter of the pelvic inlet, giving it a kidney-shaped appearance. The lower segment of the sacrum shifts backward, losing its normal curvature and becoming straight and tilted backward. The coccyx is hook-shaped and protrudes toward the pelvic outlet plane. Due to the outward splaying of the iliac bones, the interspinous diameter equals or exceeds the intercristal diameter. The outward rotation of the ischial tuberosities increases the pubic arch angle, widening the transverse diameter of the pelvic outlet (Figure 8).
Figure 8: Rickets-induced flat pelvis
2. Narrow midpelvis and pelvic outlet plane:
(1) Funnel-shaped pelvis (funnel pelvis): The diameters of the pelvic inlet are normal. However, the pelvic walls on both sides incline inward, resembling a funnel, hence the name. Its characteristics include significant narrowing of both the midpelvis and pelvic outlet planes, shortening the interspinous and intertuberous diameters, with a pubic arch angle <90°. The sum of the intertuberous diameter and the posterior sagittal diameter of the outlet is <15 cm. This is commonly seen in android pelves (Figure 9).
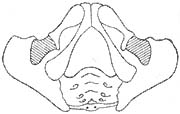
Figure 9: Funnel-shaped pelvic outlet
(2) Transversely contracted pelvis: Similar to the anthropoid pelvis. The transverse diameters of the pelvic inlet, midpelvis, and pelvic outlet are all shortened, while the anteroposterior diameter is slightly longer, and the sciatic notch is wide (Figure 10). The sacral external diameter measurement is normal, but the interspinous and intercristal diameters are both shortened.

Figure 10: Transversely contracted pelvis
3. Narrowing of all three pelvic planes: The pelvis appears gynecoid in shape, but the inlet, midpelvis, and outlet planes are all narrowed, with each plane's diameter reduced by 2 cm or more compared to normal. This is called a generally contracted pelvis (Figure 11) and is often seen in short-statured, proportionally built women.
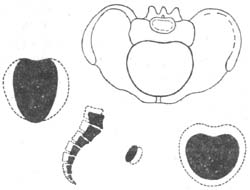
Figure 11: Generally contracted pelvis
4. Deformed pelvis: The pelvis loses its normal shape. Only the following two types are introduced here:
(1) Osteomalacic pelvis: Now rare. It is caused by deficiencies in calcium, phosphorus, vitamin D, and insufficient ultraviolet exposure, leading to impaired bone mineralization in adulthood, replaced by osteoid tissue, resulting in decalcification, osteoporosis, and softening. Due to the pressure from the trunk's weight and the inward-upward compression of the femurs, the sacral promontory protrudes forward, and the pubic symphysis bulges outward, giving the pelvic inlet a concave triangular shape. The intertrochanteric and intertuberous diameters are significantly shortened. In severe cases, the vagina cannot accommodate two fingers (Figure 12).

Figure 12 Osteomalacia Pelvis
(2) Obliquely Contracted Pelvis: Caused by underdevelopment of one iliac wing and hip bone, resulting in sacroiliac joint fixation, as well as diseases of the lower limbs and hip joint, leading to a shortened oblique diameter of the pelvis on one side (Figure 13).

Figure 13 Obliquely Contracted Pelvis
Effects of Contracted Pelvis on Mother and Fetus
1. Effects on the Mother: If the pelvic inlet plane is contracted, it affects the engagement of the fetal presenting part, increasing the likelihood of abnormal fetal positions and secondary uterine inertia, leading to prolonged or arrested labor. If the midplane of the pelvis is contracted, it affects the internal rotation of the fetal head, increasing the likelihood of persistent occiput transverse or occiput posterior positions. Prolonged impaction of the fetal head in the birth canal compresses soft tissues, causing local ischemia, edema, necrosis, and sloughing, which may result in genital fistulas postpartum. Premature rupture of membranes and operative deliveries increase the risk of infection. Severe obstructive dystocia, if not managed promptly, can lead to threatened uterine rupture or even uterine rupture, endangering the mother's life.
2. Effects on the Fetus and Newborn: Cephalopelvic disproportion increases the risk of premature rupture of membranes and umbilical cord prolapse, leading to fetal distress or even fetal death. Prolonged labor and compression of the fetal head may cause ischemia and hypoxia, increasing the risk of intracranial hemorrhage. A narrow birth canal raises the likelihood of operative deliveries, increasing the risk of neonatal birth injuries and infections.
During the process of childbirth, the pelvis is a constant factor. A narrow pelvis affects the descent and internal rotation of the fetal position and presenting part in the mechanism of childbirth, as well as uterine contractions. When estimating the difficulty of childbirth, the pelvis is an important factor to consider. During pregnancy, it is essential to identify any abnormalities in the pelvis, such as cephalopelvic disproportion, and make an early diagnosis to determine the appropriate mode of childbirth.
1. Medical history: Inquire whether the pregnant woman had rickets, poliomyelitis, subcutaneous nodules of the spine and hip joints, or a history of trauma during childhood. For multiparous women, it is important to understand whether there was a history of difficult delivery and its causes, as well as whether the newborn suffered any birth injuries.
2. General examination: Measure the height. If the pregnant woman is shorter than 145 cm, be alert to the possibility of a generally contracted pelvis. Observe the pregnant woman’s body shape, gait for any limping, spinal or hip joint deformities, whether the Michaelis rhomboid is symmetrical, and whether there is a pointed or pendulous abdomen.
3. Abdominal examination
(1) Abdominal shape: Observe the abdominal contour, measure the uterine height above the pubis and abdominal circumference with a tape, and use B-ultrasound to assess the relationship between the fetal presenting part and the pelvis. Additionally, measure the fetal biparietal diameter, chest diameter, abdominal diameter, and femur length to predict fetal weight and determine whether the fetus can pass smoothly through the bony birth canal.
(2) Abnormal fetal position: Narrow pelvic inlet often leads to cephalopelvic disproportion, making it difficult for the fetal head to engage, resulting in abnormal fetal positions such as breech or shoulder presentation. A narrow midpelvis affects the internal rotation of the engaged fetal head, leading to persistent occiput transverse or occiput posterior positions.
(3) Estimation of cephalopelvic relationship: Under normal circumstances, some primiparous women experience fetal head engagement two weeks before the due date, while multiparous women experience it after labor begins. If the fetal head has not engaged after labor begins, the cephalopelvic relationship should be thoroughly assessed. The specific method to check for cephalopelvic disproportion is as follows: The pregnant woman empties her bladder, lies supine with legs straight. The examiner places a hand above the pubic symphysis and pushes the floating fetal head toward the pelvic cavity. If the fetal head is below the plane of the pubic symphysis, it indicates that the fetal head can engage, and cephalopelvic disproportion is unlikely; this is called a negative "overlapping pubic sign." If the fetal head is at the same level as the pubic symphysis, it suggests possible cephalopelvic disproportion, termed a "suspiciously positive overlapping pubic sign." If the fetal head is above the plane of the pubic symphysis, it indicates obvious cephalopelvic disproportion, termed a "positive overlapping pubic sign" (Figure 1). For pregnant women with a positive overlapping pubic sign, have them assume a semi-recumbent position with legs flexed and recheck the overlapping pubic sign. If it turns negative, it suggests abnormal pelvic inclination rather than cephalopelvic disproportion.
|
|
|
|
(1) Cephalopelvic proportion | (2) Possible cephalopelvic disproportion | (3) Cephalopelvic disproportion |
Figure 1: Assessing the degree of cephalopelvic proportion
4. Pelvic measurement
(1) External pelvic measurement: If all diameters of the external pelvic measurement are <2cm or more below the normal value, it is a generally contracted pelvis; a sacral external diameter <18cm indicates a flat pelvis. An intertuberous diameter <8cm and a pubic arch angle <90° suggest a funnel-shaped pelvis. If the difference between the two oblique diameters of the pelvis (the distance from the anterior superior iliac spine on one side to the posterior superior iliac spine on the opposite side) and the ipsilateral diameter (the distance from the anterior superior iliac spine to the posterior superior iliac spine on the same side) exceeds 1cm, it is an oblique pelvis.
(2) Internal Pelvic Measurement: When abnormalities are detected in external pelvic measurements, internal pelvic measurements should be performed. A diagonal conjugate diameter <11.5 cm with a prominent sacral promontory indicates a narrowed pelvic inlet plane, characteristic of a flat pelvis. Narrowing of the mid-pelvic plane and pelvic outlet plane often coexist. The following should be measured: the curvature of the anterior sacral surface (Figure 2), the interspinous diameter (between the ischial spines), and the width of the sciatic notch (i.e., the width of the sacrospinous ligament) (Figure 3). If the interspinous diameter is <10 cm and the sciatic notch width is less than two fingerbreadths, it indicates mid-pelvic plane narrowing. If the intertuberous diameter is <8 cm, the posterior sagittal diameter of the outlet should be measured, and the mobility of the sacrococcygeal joint should be assessed (Figure 4) to estimate the degree of pelvic outlet plane narrowing. If the sum of the intertuberous diameter and the posterior sagittal diameter is <15 cm, it indicates pelvic outlet plane narrowing.

Figure 2 Examination of the anterior sacral curvature
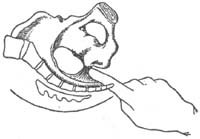
Figure 3 Examination of the sciatic notch width

Figure 4 Examination of sacrococcygeal joint mobility
bubble_chart Treatment Measures
The management principles for childbirth with a narrow pelvis are: identify the type and degree of pelvic narrowing, assess fetal position, fetal size, fetal heart rate, strength of uterine contractions, cervical dilation, and whether the membranes have ruptured. Combine these factors with the mother's age, parity, and previous childbirth history to make a comprehensive judgment and determine the mode of delivery.
1. General Management During childbirth, the mother should be comforted to maintain a positive and confident mindset. Ensure adequate nutrition and hydration, with intravenous fluids administered if necessary. Monitor the mother's rest, the strength of uterine contractions, fetal heart rate, and the descent of the fetal presenting part.
2. Management of Narrow Pelvic Inlet
(1) Significant cephalopelvic disproportion (absolute pelvic narrowing): If the external conjugate diameter is <16 cm and the anteroposterior diameter of the pelvic inlet is <8.5 cm, a full-term live fetus cannot engage and vaginal delivery is impossible. Cesarean section should be performed near the due date or after the onset of labor.
(2) Grade I cephalopelvic disproportion (relative pelvic narrowing): If the external conjugate diameter is 16–18 cm, the anteroposterior diameter of the pelvic inlet is 8.5–9.5 cm, the full-term fetus weighs <3000 g, and the fetal heart rate is normal, a trial of labor under close monitoring is appropriate. If uterine contractions are weak and the membranes are intact during labor, artificial rupture of membranes may be performed when the cervix is dilated to 3 cm. If contractions strengthen after membrane rupture and labor progresses smoothly, vaginal delivery is often possible. If after 2–4 hours of trial labor, the fetal head still fails to engage, or signs of fetal distress appear, cesarean section should be performed promptly. If the membranes have already ruptured, the trial labor period should be shortened to reduce the risk of infection.
In women with a narrow pelvic inlet (primarily flat pelvis), by the end of pregnancy or after labor begins, the sagittal suture of the fetal head can only align with the transverse diameter of the inlet. Lateral flexion of the fetal head allows the two parietal bones to engage sequentially, resulting in an unevenly inclined entry into the pelvic inlet, known as uneven cephalopelvic inclination. If the anterior parietal bone engages first and the sagittal suture is posterior, it is called anterior asynclitism; if the posterior parietal bone engages first and the sagittal suture is anterior, it is called posterior asynclitism (Figure 5). Once both parietal bones pass through the pelvic inlet, vaginal delivery can proceed more smoothly.
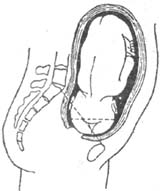
Figure 5: Fetal Head Engagement in the Pelvis—Posterior Asynclitism
3. Management of Narrow Midpelvis and Pelvic Outlet During childbirth, the fetus completes flexion and internal rotation at the midpelvis. If the midpelvis is narrow, flexion and internal rotation of the fetal head may be obstructed, leading to persistent occiput transverse or occiput posterior positions. If the cervix is fully dilated and the biparietal diameter of the fetal head reaches or descends below the ischial spines, assisted vaginal delivery may be attempted. If the biparietal diameter does not reach the ischial spines or signs of fetal distress appear, cesarean section should be performed.
The pelvic outlet is the lowest part of the birth canal. Before labor, fetal size and the cephalopelvic relationship should be thoroughly assessed to determine the feasibility of vaginal delivery, avoiding trial labor if contraindicated. If the transverse outlet diameter is narrow and the subpubic arch space cannot be utilized, the presenting part may shift posteriorly to utilize the posterior outlet triangle for delivery (Figure 6). Clinically, the sum of the transverse outlet diameter and the posterior sagittal diameter is used to estimate outlet size. If the sum exceeds 15 cm, vaginal delivery is usually possible; if the sum is 13–15 cm, vacuum extraction or forceps delivery may be required; if the sum is less than 13 cm, a full-term fetus generally cannot be delivered vaginally, and cesarean section should be performed.
|
|
|
|
| (1) Normal | (2) Although the transverse diameter is small, the posterior sagittal diameter is long, and the fetal head can utilize the posterior triangular area for delivery | (3) Both the transverse diameter and posterior sagittal diameter are small, and the fetal head cannot be delivered |
Figure 6 Relationship between the transverse diameter of the outlet and the posterior sagittal diameter
4. Management of Narrowing in All Three Planes of the Pelvis Primarily refers to the generally contracted pelvis. If the fetus is estimated to be not too large and cephalopelvic disproportion is absent, a trial of labor may be attempted. If the fetus is relatively large with absolute cephalopelvic disproportion, and the fetus cannot pass through the birth canal, a cesarean section should be performed as early as possible.
5. Management of Deformed Pelvis A detailed analysis should be conducted based on the type of pelvic deformity, the degree of narrowing, fetal size, uterine contractions, and other factors. If the deformity is severe and cephalopelvic disproportion is evident, a seasonal epidemic cesarean section should be performed promptly.