| disease | Peritonsillar Abscess |
| alias | Purulent Phlegmonous Angina, Throat Abscess |
Peritonsillar abscess is a suppurative inflammation of the peritonsillar space, also known as suppurative cellulitis angina, referred to as "throat abscess" in Chinese medicine. It is commonly seen in young adults.
bubble_chart Etiology
Peritonsillar abscess is mostly a complication of acute suppurative tonsillitis. Due to poor drainage of the tonsillar crypts, especially the upper crypts, or deep follicular suppuration, the infection spreads deeper, penetrating the tonsillar capsule into the peritonsillar space. Inflammation around the molars can also extend to the peritonsillar space. Initially, it presents as inflammatory infiltration, known as peritonsillitis, which then progresses to abscess formation. The abscess is most commonly located in the anterior-superior part of the tonsil, between the palatoglossal arch and the lingual tonsil, while posterior-superior or other locations are rare. It usually occurs unilaterally. The causative bacteria include Staphylococcus aureus, beta-hemolytic streptococcus, alpha-hemolytic streptococcus (viridans group), and anaerobic streptococci (foul-smelling).
bubble_chart Clinical Manifestations
Most cases occur 3-5 days after the onset of acute tonsillitis or just as the condition begins to improve. The patient's body temperature rises, with severe cases presenting high fever, shivering, and systemic toxic symptoms. The pain on one side of the throat worsens compared to tonsillitis, often radiating to the same-side ear and teeth. Due to severe throat pain and swelling of the soft palate, the patient experiences difficulty swallowing, excessive drooling, nasal regurgitation of water, and slurred speech. If the surrounding inflammation affects the medial pterygoid muscle, trismus occurs. A large abscess may cause upper respiratory tract obstruction.
The patient appears distressed, with the head tilted slightly forward toward the affected side. Fetid mouth odor, excessive salivation, thick and greasy tongue coating, limited mouth opening, and swollen, tender cervical lymph nodes are present. In anterior-superior abscesses, the upper part of the palatoglossal arch and soft palate on the affected side are congested, swollen, and markedly bulging, with the tonsils covered in purulent discharge and pushed inferomedially. The uvula is congested, swollen, and deviated to the opposite side. In posterior-superior abscesses, the palatopharyngeal arch on the affected side is significantly swollen and bulging, pushing the tonsils anteroinferiorly. Inferior abscesses are rare but may be complicated by pharyngeal and laryngeal edema and cervical stirred pulse sheath inflammation, with prominent swelling between the root of the nose and the base of the tongue, while congestion and swelling of the soft palate and uvula are less noticeable.Based on the medical history, symptoms, and signs, the diagnosis is not difficult. Typically, the formation of an abscess can be determined by the following points: restricted mouth opening, obvious local swelling, and localized tenderness occurring 4–5 days after onset. If necessary, pus can be aspirated by puncturing the highest point of the soft palate swelling to confirm the diagnosis.
bubble_chart Treatment Measures
1. Treatment before abscess formation The treatment is the same as for acute tonsillitis. Intravenous administration of sufficient antibiotics is necessary to control the spread of inflammation, prevent abscess formation, and avoid complications. Local injection of penicillin with procaine or gentamicin can also be used for its anti-inflammatory and analgesic effects.
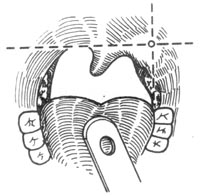
2. Needle aspiration Aspiration can confirm whether an abscess has formed and determine its location, while also serving as a treatment. Under surface anesthesia with 0.5–1% dicaine, select the most prominent and softened area of the abscess for exploratory needle insertion. Pay attention to the direction and avoid inserting too deeply to prevent accidental injury to major blood vessels in the parapharyngeal space. A hollow sensation is felt when the needle enters the abscess cavity, and pus is aspirated upon withdrawal. Aspirate as much pus as possible, then keep the needle in place, replace the syringe, and rinse the cavity with antibiotic solution (Figure 1).Figure 1: Aspiration site
3. Incision and drainage Under local anesthesia, perform incision and drainage at the site of abscess aspiration. If the incision site cannot be determined, draw an imaginary horizontal line from the base of the uvula and an imaginary vertical line from the lower end of the free edge of the palatoglossal arch. The incision should be made slightly outside the intersection of these two lines. The incision should be 1–1.5 cm long, cutting through the mucosa and superficial tissue (avoiding excessive depth). Use a hemostat to separate the soft tissue layer by layer along the muscle fibers posteriorly and laterally until the abscess cavity is reached for pus drainage. No drainage strip is left postoperatively. The incision is dilated and the cavity rinsed daily until healing occurs in a few days (Figure 2).
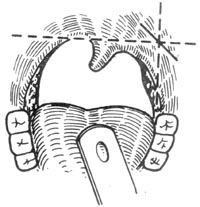
Figure 2: Incision and drainage site
4. Tonsillectomy during the abscess stage Generally, tonsillectomy is performed 2–3 weeks after acute inflammation subsides. However, for peritonsillar abscess, the affected tonsil can be removed under adequate antibiotic control shortly after diagnosis or a few days after incision and pus drainage. At this stage, the abscess has already separated the tonsil from its bed, making surgical dissection easier with less bleeding and pain. After tonsillectomy, the abscess cavity is fully exposed, facilitating complete drainage and healing. Early removal of the lesion reduces complications and avoids the difficulty of dissection due to scar formation in future surgeries.
bubble_chart ComplicationsInflammation spreading downward can cause acute inflammation of the pharynx and larynx, especially in the case of abscess formation, which may lead to upper respiratory tract obstruction and rapidly result in difficulty breathing. The inflammation can spread through the lateral pharyngeal wall into the parapharyngeal space, forming a parapharyngeal abscess. A few cases may be complicated by carotid sheath infection, jugular vein thrombosis, sepsis, or suppurative cervical lymphadenitis. If the abscess ruptures during deep sleep and pus flows into the larynx and trachea, it may cause asphyxia or aspiration pneumonia, though this is rare.
It needs to be differentiated from the following diseases.
1. Parapharyngeal abscess The lateral pharyngeal wall on the affected side, together with the tonsil, is displaced inward and bulges. Trismus may also occur, but pharyngeal inflammation is mild, and the tonsil itself shows no significant lesions. Severe radiating pain is present in the lateral neck, often accompanied by inflammatory abscess and marked tenderness.
2. Wisdom tooth pericoronitis Often associated with impacted mandibular wisdom teeth and the formation of periodontal pockets. The gingival flap and surrounding soft tissues are red, swollen, and painful. Inflammatory swelling may extend to the palatoglossal arch, but the tonsil and uvula are unaffected.
3. Tonsillar abscess This is an abscess within the tonsil itself. Pus can be aspirated by puncturing the tonsil, and pus may be seen draining from the tonsillar crypts. The affected tonsil is swollen, with inflammation infiltrating the surrounding tissues, but trismus is absent.
4. Ludwig's angina An acute infection of the floor of the mouth, leading to diffuse cellulitis. Inflammatory masses in the floor of the mouth and submental region elevate the tongue, causing pain upon tongue depression and difficulty in tongue protrusion. Trismus is present but not lockjaw. If the infection spreads to the pharynx and larynx, upper respiratory obstruction may occur. The soft palate and palatoglossal arch are congested and swollen. This condition is often caused by odontogenic infections.