| disease | Ossification of the Cervical Ligamentum Flavum |
Following Elsberg's first report on ligamentum flavum hyperplasia, there have been numerous literature reports on ligamentum flavum folding into the spinal canal and thickening of the ligamentum flavum. Gradually, attention has been drawn to spinal canal stenosis caused by abnormalities in the ligament components within the spinal canal. In 1912, Le Double was the first to describe the phenomenon of ossification of the ligamentum flavum (OLF). In 1920, Polgar first reported the X-ray manifestations of OLF. Subsequently, Schmorl, Shore, Yamaguchi, and Koizumi, among others, reported on the condition. After the 1970s, many scholars, particularly Japanese researchers, conducted extensive and in-depth studies on this topic. With the continuous advancements in myelography, CT scans, and MRI examinations, OLF has been recognized as an independent clinical disease and is increasingly attracting attention.
bubble_chart Epidemiology
Ossification of the ligamentum flavum is a disease predominantly affecting the elderly, with a higher incidence in males, with a male-to-female ratio of 2:1. The 50-60 age group shows a higher proportion, and there is a trend of increasing incidence with age. Regarding the incidence of ligamentum flavum ossification, reports vary significantly. A radiographic survey of 333 cases conducted by Qimu found that 25% exhibited ossification of the ligamentum flavum.
The etiology of ossification of the ligamentum flavum remains unclear. It is generally believed to be closely related to various factors such as local mechanical factors, metabolic abnormalities, and familial inheritance. Any factors that abnormally increase the load on the osseous attachment sites of the ligamentum flavum may cause ligament injury, and repeated injury accumulation and reactive repair processes can lead to ligament ossification.
Similar to the occurrence of ossification of the posterior longitudinal ligament, ossification of the ligamentum flavum is more prevalent in regions such as Japan and Southeast Asia, where diets are high in sugar (mainly rice-based), as well as among populations with diabetes. This suggests that ossification of the ligamentum flavum is associated with systemic conditions such as glucose metabolism. Many authors propose that ossification of the ligamentum flavum is actually part of spinal ligament ossification syndrome, while others suggest that the disease is related to genetic factors, such as the HLA antigen system and racial differences. There has been a reported case of identical twins both suffering from ossification of the ligamentum flavum complicated by ossification of the posterior longitudinal ligament.bubble_chart Pathological Changes
The ligamentum flavum is a ligament that connects adjacent vertebral laminae in the spine. It has the highest content of elastic fibers among all ligaments in the human body and is named for its yellowish appearance. The ligamentum flavum extends from the lower edge of the second cervical vertebra to the upper edge of the first sacral vertebra and participates in forming the posterior wall of the spinal canal. Its lower edge attaches to the upper edge and posterior superior surface of the lower vertebral lamina and the anteromedial aspect of the superior articular process, while its upper edge attaches to the lower edge and anterior inferior surface of the upper vertebral lamina and the anteromedial aspect of the inferior articular process. Additionally, the slight forward tilt of the upper edge of the vertebral lamina ensures the posterior wall of the spinal canal is very smooth. From a posterior view, the ligamentum flavum is divided into two symmetrical halves, fusing with the interspinous ligament at the midline and extending laterally to the intervertebral foramen to form the posterior wall, where it merges with the joint capsule at the lateral aspect of the intervertebral foramen. The ligamentum flavum is typically divided into two parts: the interlaminar portion and the capsular portion. At the midline of the ligamentum flavum, small veins penetrate at nearly every level.
The ligamentum flavum contains 60–80% elastic fibers, with those in the cervical region arranged longitudinally. When the spine is in maximum flexion, it can elongate by 35–45% compared to the neutral position, whereas during maximum extension, the ligamentum flavum thickens and shortens by 10%. Under normal conditions, due to the ligament's pre-tension, it does not fold or buckle into the spinal canal during hyperextension. Biomechanical studies also show that the ligamentum flavum only ruptures when stretched by 70%, allowing it to facilitate free movement of the spine within a normal range while absorbing excessive energy to stabilize the spine and protect the spinal cord.Ossification of the ligamentum flavum often begins at its attachment to the upper edge of the vertebral lamina and the medial side of the superior articular process, gradually extending upward, laterally, and toward the midline. Anterior progression may also lead to so-called hyperostosis of the pedicle. Histopathological studies indicate that ossification of the ligamentum flavum primarily occurs through endochondral ossification. In the early stages of the disease, the fibrous structure becomes disorganized, collagen fibers proliferate significantly, and elastic fibers are drastically reduced. Within the swollen collagen fibers, numerous fibrocartilage cells and abundant island-like ossification foci are present, containing trabecular bone, marrow cavities, and Haversian canals. Normally, the nutrient vessels of the ligamentum flavum are located at the midline of the vertebral lamina edge and the anterior part of the superior articular process. During ossification, a large number of vascular tissues can be observed at the edges of the ossification foci.
Some researchers have found cartilage metaplasia and endochondral ossification within calcified foci of the ligamentum flavum, suggesting that calcification and ossification are different stages of the same pathological process. However, most believe that calcification and ossification of the ligamentum flavum are two distinct pathological processes. During calcification, the ligamentum flavum thickens significantly and contains sand-like or milky calcified nodules. Microscopic examination reveals calcium salt deposition in fibrous or cartilaginous matrices, surrounded by numerous multinucleated giant cells, histiocytes, and lymphocytes, presenting as a granulomatous foreign body reaction. This is entirely different from ossification, which is characterized by trabecular bone and marrow structures. X-ray diffraction analysis of calcified deposits shows they consist of mineral crystals such as hydroxyapatite, calcium pyrophosphate, and calcium phosphate.Ossification of the cervical ligamentum flavum forms nodular protrusions, causing bony spinal canal stenosis due to ligamentous pathology. Depending on whether ossification occurs in the interlaminar or capsular portion, it can lead to stenosis in the central spinal canal, the nerve root canal, or both, compressing the local cervical spinal cord and nerve roots. This results in pathological changes such as neural congestion, edema, thinning of the diameter, and demyelination. Neurological damage is not only caused by repeated minor local compression but is also associated with long-standing grade I microcirculatory disturbances.
bubble_chart Clinical Manifestations
Ossification of the ligamentum flavum can occur in the cervical, thoracic, and lumbar spine, but it is relatively rare in the cervical spine, with the thoracic and lumbar regions being more common. Such patients often also exhibit ossification of other spinal ligaments, such as the anterior longitudinal ligament, posterior longitudinal ligament, and supraspinous ligament.
Ossification of the ligamentum flavum is frequently observed in the middle and lower cervical vertebrae, particularly at C5–6 and C6–7. The affected area typically spans 1–2 vertebral segments, while multilevel ossification is very rare. Within the same segment, the incidence of bilateral and unilateral lesions is similar. Among unilateral lesions, the left side is more commonly affected.
Clinically, ossification of the cervical ligamentum flavum manifests as spinal cord compression symptoms due to cervical spinal canal stenosis. Most patients initially experience limb pain and numbness, especially in the upper limbs and fingers. As symptoms worsen, swelling, lack of strength, stiffness, and limb inflexibility may occur, accompanied by neck pain, stiffness, limited mobility, and aching. Some patients may report a sensation of tightness around the chest, varying degrees of lower limb muscle weakness, and unsteady gait, described as a "walking-on-cotton" feeling. In severe cases, dysfunction of bowel and bladder control and sexual dysfunction may arise. When spinal cord compression is significant, pyramidal tract symptoms may appear, including hyperreflexia, increased muscle tone, positive knee and ankle clonus, and positive pathological reflexes. Sensory disturbances vary and may include segmental spinal cord sensory deficits, localized sensory disturbances along nerve root distributions, and Brown-Sequard syndrome.
bubble_chart Auxiliary Examination
Since the clinical manifestations of this disease are often similar to those of cervical spondylosis and cervical spinal canal stenosis, lacking specificity, the diagnosis primarily relies on imaging examinations.
On plain X-ray films, the ossified shadow of the ligamentum flavum often overlaps with the vertebral body image, making it difficult to distinguish. On lateral views, a hyperdense ossified mass shadow can be seen on the ventral side of the lamina or between the laminae, with the lower edge starting from the upper edge of the next lamina and the upper edge ending at the midpoint of the lamina. The shape is often triangular. If the ossification is small or difficult to identify, tomography can be performed to further clarify the diagnosis.
It is worth noting that X-rays often reveal ossification in other ligaments at different locations. Literature indicates that nearly half of patients with cervical ligamentum flavum ossification also exhibit ossification in other spinal ligaments, such as thoracic ligamentum flavum ossification or cervical posterior longitudinal ligament ossification. Additionally, other cervical conditions, such as degenerative changes, developmental spinal canal stenosis, and congenital cervical deformities, may also be observed.
Myelography shows complete or incomplete obstruction at the level of ossification. On X-ray films, the source of incomplete obstruction often appears to originate from the posterior aspect of the dura mater.
CT scans can clearly display the mass-like ossification located on the ventral side of the cervical lamina, protruding into the spinal canal and compressing the cervical spinal cord (Figure 1). The CT value is similar to that of bone. If CT myelography is performed, the compression and displacement of the cervical spinal cord and dura mater can be observed, further assessing the degree of compression.
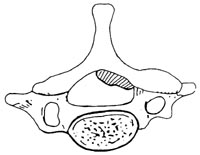
Figure 1: Ossification of the cervical ligamentum flavum.
On MRI, T1- and T2-weighted sagittal images show thickened and ossified ligamentum flavum as low-signal masses protruding into the spinal canal, compressing the dorsal dura mater. When the ligamentum flavum degenerates and thickens, it also appears as isointense or low-signal masses on T1- and T2-weighted images, but the morphology often differs. Degenerative changes typically present as multisegmental, semicircular shadows, whereas ossification appears as a single-segmental triangular shadow with more severe compression.
Some scholars have pointed out that ossified ligamentum flavum, like other bone tissues, contains bone marrow and fat, which may appear as high-signal areas on T1-weighted images. Studies correlating MRI signal intensity with pathological and immunohistochemical findings have revealed that isointense regions on MRI represent small proliferating blood vessels in the hypertrophic ligament, marking the onset of the ossification progression phase.
Although MRI is less clear than CT in displaying cervical ligamentum flavum ossification on axial images, it allows direct sagittal imaging. Besides showing the degree of spinal cord compression, it can also reveal signal changes in the compressed spinal cord, aiding in prognosis assessment.
bubble_chart Treatment Measures
Non-surgical treatment
For patients with mild symptoms, non-surgical treatment can be adopted, including neck immobilization, cervical collar fixation, physical therapy, medication, etc. However, most patients often show poor response to non-surgical treatments.
Surgical treatment
It is generally believed that when symptoms of spinal cord or nerve root compression are evident, posterior cervical surgery should be performed to completely remove the ossified and thickened ligamentum flavum. This is an effective measure to relieve compression and restore spinal cord function. Surgical methods include simple laminectomy and laminoplasty. Since the ossified ligamentum flavum is often continuous with the lamina edge and adherent to the dura mater, extreme care must be taken during the operation to prevent spinal cord injury and cerebrospinal fluid leakage. If the dura mater is damaged, surgical repair should be performed.
Compared to ossification of the cervical ligamentum flavum, calcification of the cervical ligamentum flavum is more common. The two conditions share similar clinical and imaging manifestations, and differentiation between them should be noted (Table 1).
Table 1 Differentiation Between Ossification and Calcification of the Ligamentum Flavum
| Ossification of the Ligamentum Flavum | Calcification of the Ligamentum Flavum | |
| Gender | More common in males | More common in females |
| Level of Lesion | Occurs throughout the spine, more common in the lower thoracic spine | Only seen in the lower cervical segment |
| Location of Lesion | Attachment to the lamina | Between the laminae |
| Morphology of Lesion | Spinous, plate-like, or nodular | Round or oval |
| Relationship to Lamina | Continuous, does not move with posture changes | Discontinuous |
| Relationship to Dura Mater | Often adherent or fused | Not adherent |
| Association with Calcification in Other Body Parts | None | Common |




