| disease | Oral Herpes Simplex |
| alias | Herpes Simplex |
Herpes simplex is a skin and mucous membrane disease caused by the herpes simplex virus.
bubble_chart Etiology
The pathogenic microorganism causing infections in the oral cavity and perioral skin is the herpes simplex virus type I. Humans are the natural hosts of this virus. When the herpes virus comes into contact with susceptible host cells, viral particles enter the cells and their nuclei. The nucleic acid at the core synthesizes proteins and amino acids within the nucleus, utilizing the host cell's amino acids and enzymes to replicate new viral particles. These particles then spread through the cytoplasm and cell membrane to surrounding areas, causing an acute outbreak known as primary herpes simplex. If the body develops antibodies after exposure to the virus, but the quantity is insufficient, factors such as a common cold, excessive fatigue, digestive dysfunction, or local mechanical irritation—which lower the body's resistance—can reactivate the latent virus within the cells, leading to replication and recurrence, known as recurrent herpes simplex.
The disease spreads through contact with saliva droplets.
bubble_chart Pathological Changes
The epithelial cells undergo degeneration, exhibiting acantholytic ballooning degeneration and reticular degeneration. After ballooning degeneration, the epithelial cells significantly swell into a round shape, with uniformly eosinophilic-stained cytoplasm. The nucleus may be single, multiple, or absent, and the intercellular bridges may disappear, causing the cells to separate and form vesicles. Ballooning-degenerated epithelial cells are mostly located at the base of the vesicles. Reticular liquefaction involves intracellular edema in the epithelial cells, with swollen and ruptured cell walls that fuse to form multilocular vesicles. The cell nuclei contain eosinophilic viral inclusion bodies. The connective tissue beneath the epithelium shows edema and inflammatory cell infiltration.
bubble_chart Clinical Manifestations1. Primary Herpetic Stomatitis This disease is mostly an initial occurrence, also known as primary herpetic stomatitis. It is commonly seen in infants or children, with the highest incidence between the ages of 2 and 3. After the herpes simplex virus enters the body, there is an incubation period of about 10 days. Affected children may exhibit symptoms such as restlessness, fever, headache, sore throat, crying, and refusal to eat. After 2–3 days, the body temperature gradually decreases, and lesions may appear on any part of the oral mucosa, such as the lips, cheeks, tongue, as well as the well-keratinized hard palate, gums, and dorsum of the tongue. Initially, the mucosa becomes congested, red, and edematous, followed by the appearance of numerous clustered, pinhead-sized, thin-walled, transparent small blisters with a diameter of about 1–2 mm, round or oval in shape, surrounded by a narrow red halo. The blisters rupture quickly, leaving superficial ulcers that may coalesce into larger ulcers covered with yellowish-white pseudomembranes, surrounded by congested and reddened areas. At this stage, saliva production increases significantly, accompanied by severe pain, swollen local lymph nodes, and tenderness. The disease is self-limiting, with a course of about 7–14 days (Figure 1).
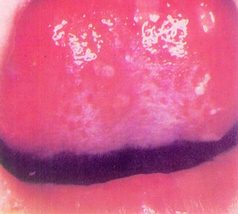
Figure 1 Herpetic Stomatitis
2. Herpes Labialis Commonly seen in adults, it often occurs after primary herpes infection when systemic resistance is reduced. It manifests as a burning pain, swelling, and itching at the junction of the vermilion mucosa and skin of the lips, followed by erythema and blisters, numerous in number, resembling foxtail millet in size, often clustered. In the initial stage, the blister fluid is slightly yellow and transparent, but later the blisters rise, enlarge, and coalesce, and the fluid becomes turbid. After rupture, the blisters dry and form yellowish crusts, which shed without leaving scars but may cause temporary pigmentation. If secondary infection occurs, pustules may form, intensifying the pain. This condition is also self-limiting and can heal on its own (Figure 2).

Figure 2 Herpes Labialis
Based on the following characteristics, the diagnosis can be easily made:
1. Herpetic stomatitis: Mostly seen in infants and young children. After high fever and sore throat, clusters of small blisters or ulcers appear on the oral mucosa, which may merge to form larger ulcers. It usually heals on its own within 7–14 days.
2. Herpes labialis: Mostly seen in adults. The lesions typically occur on the vermilion border of the lips and adjacent skin, presenting as clusters of blisters accompanied by itching. After rupture, they form scabs. The condition is self-limiting and recurrent.
During the onset, the diagnosis can be confirmed by viral inoculation of the blister fluid, a smear from the base of the blister, or an elevated serum antibody titer against herpes simplex virus.
bubble_chart Treatment Measures
There is still a lack of specific antiviral therapy, and symptomatic treatment is mainly adopted to shorten the course of the disease, alleviate suffering, and promote healing.
(1) Local treatment: Use anti-inflammatory and analgesic agents, but avoid hormonal drugs.
1. Topical application: 1% chlortetracycline glycerin, neomycin or bacitracin or boric acid ointment, 1% Chinese Gentian violet solution, 0.1% idoxuridine eye drops, etc.
2. Wet compress: 0.1% ethacridine lactate (Rivanol) solution, 0.025%~0.05% zinc sulfate solution.
3. Mouthwash: If the pain is severe, use 1~2% procaine or 0.5~1% dyclonine solution for gargling to relieve pain.
4. Laser irradiation: Can stop itching, relieve pain, and promote the absorption of blister fluid and scab formation.
(2) Systemic treatment
2. Systemic medication: Moroxydine (ABOB) can be taken, 0.2g per tablet, 1~2 tablets each time, three times daily. Oral Isatis Root tablets or infusion granules, stomatitis infusion granules, etc.
For severe cases, drugs such as levamisole, poly I:C, and interferon may be selected.
Herpetic stomatitis should be differentiated from herpetiform stomatitis (see table).
Table Differentiation between Herpetic Stomatitis and Herpetiform Stomatitis
| Herpetic Stomatitis | Herpetiform Stomatitis | |
| Age of Onset | Infants and young children | Adults |
| Ulcer Characteristics | The mucous membrane shows extensive congestion, with clusters of multiple small ulcers on the congested mucosa. Ulcers may merge to form larger ones with irregular edges. | The mucous membrane lacks extensive congestion, with ulcers surrounded by a red halo. Ulcers are mostly distributed in areas of the oral mucosa with poor keratinization, do not cluster, and generally do not merge. |
| Skin Lesions | May sometimes affect the vermilion border of the lips | No concurrent skin lesions |
| Recurrence | Rarely recurs | Characterized by recurrent episodes |






