| disease | Sacroiliac Joint Tuberculosis |
This disease is not uncommon, often coexisting with subcutaneous nodes in adjacent lumbosacral vertebrae or hip joints. Among 4,140 cases, 175 involved subcutaneous nodes in the sacroiliac joint, accounting for 4.23% of all bone and joint subcutaneous nodes. It predominantly affects young adults, with 114 cases (65.14%) occurring in individuals aged 21 to 40, and is more frequent in women of childbearing age. It is rare in children under 10 years old, with only 4 cases (2.29%); Oxford reported 35 cases, none of which were in this age group, while Tianjin's 67 cases included only 1 child under 10. The age distribution is noteworthy during diagnosis.
bubble_chart Clinical Manifestations
The disease progresses insidiously, often presenting with a limp, and pain is usually confined to the affected hip, potentially radiating along the sciatic nerve. Patients tend to sit with their weight on the unaffected side and may find it difficult to cross their legs or put on shoes and socks. Abscesses or sinuses may appear in the hip, groin, or greater trochanter of the femur.
bubble_chart Auxiliary Examination
In the early stage of X-ray imaging, the joint surface appears blurred, with marginal erosion and widened joint space. In the advanced stage, the joint space narrows. Additionally, sinus formation is present, often leading to secondary infection. The joint exhibits sclerosis.
In cases of severe joint destruction, the ipsilateral ilium and pubis may shift upward, resulting in pathological dislocation.
The hip abduction test and pelvic compression test on the affected side are often positive.
The diagnosis can be easily made based on clinical manifestations and X-ray findings.
bubble_chart Treatment Measures1. This disease is often associated with subcutaneous nodes in other parts of the body, and systemic chemotherapy should not be overlooked. Patients in poor general condition, especially elderly patients, should receive internal medical supportive therapy before surgery. For those with secondary infection of the sinus, sensitive antibiotics should be administered preoperatively. Patients with large abscesses or sequestra, or those with sinuses that do not heal after prolonged treatment, may undergo surgical intervention; otherwise, drug therapy alone may suffice.
2. The surgical approach depends on the location of the abscess and sinus, either anterior or posterior. If the abscess is located in the iliac fossa, it can be accessed through the anterior abdominal membrane to reach the lesion, taking care not to injure nerves and blood vessels. Whenever possible, the posterior approach is preferred, as it provides a wider surgical field and facilitates lesion management.
**Lesion Debridement:**
1. **Anesthesia:** Local anesthesia, continuous epidural anesthesia, or general anesthesia with endotracheal intubation.
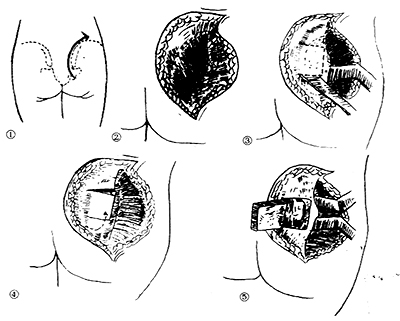
2. **Positioning:** The patient is placed in an oblique prone position with the trunk at a 60° angle to the operating table, the affected side uppermost. A pillow is placed under the waist, the healthy hip joint is flexed at 45°, and the affected hip and lumbar joints are slightly flexed. The trunk and lower limbs are secured with restraints.
3. **Operative Steps:**
(1) **Incision:** Selected based on the location of the gluteal abscess and bone lesion. ① A 12 cm incision along the line from the posterior superior iliac spine to the greater trochanter (Roaf) (Figure 1). ② An incision starting from the posterior third of the iliac crest, following the outer lip of the iliac crest in an arc to the iliac spine. The gluteus maximus is stripped laterally from beneath the iliac periosteum to expose the outer iliac plate and the posterior aspect of the sacroiliac joint (Figure 2).
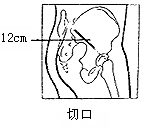
**Figure 1:** Sacroiliac Joint Lesion Debridement (after Roaf)
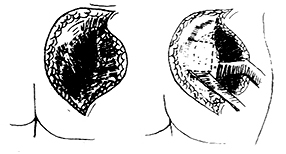
**Figure 2:** Sacroiliac Joint Lesion Debridement
(2) **Exposure of the Lesion:** The gluteus maximus is split along the direction of its fibers to reach the posterior aspect of the sacroiliac joint. The sacroiliac joint is located 2–3 cm above the greater sciatic notch. A 3 cm square bone window is chiseled here to expose the sacral surface of the sacroiliac joint (Figure 3). The excised bone block is preserved and repositioned after debridement. During exposure, care must be taken not to injure the superior gluteal artery running above the greater sciatic notch. Through this bone window, all subcutaneous nodular material, granulation tissue, and sequestra are thoroughly removed. Occasionally, abscesses in the sacrum within the pelvis can be aspirated through small openings in the sacroiliac lesion, avoiding injury to the blood vessels anterior to the sacroiliac joint. The lesion is then irrigated. Cancellous bone harvested from the posterior superior iliac spine is used to fill the joint cavity, and the preserved bone block is repositioned to achieve joint fusion.
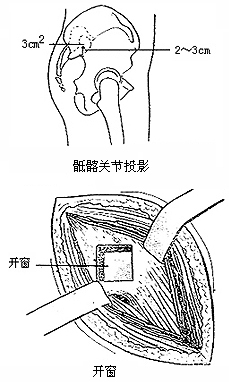
**Figure 2:** Sacroiliac Joint Lesion Debridement (after Roaf)
The wound is closed in layers, usually without drainage.
If an abscess is present in the iliac fossa, it may be debrided during the same operation or at an intermediate [second] stage, depending on the patient's condition.
4. **Postoperative Management:** The patient continues anti-subcutaneous node drug therapy and remains on a hard bed for 8–12 weeks until joint fusion is achieved before resuming activity.
**Figure 2:** Sacroiliac Joint Lesion Debridement
In 50% of cases, sacroiliac joint subcutaneous nodules are accompanied by subcutaneous nodules in other areas, such as pulmonary subcutaneous nodules, pleuritis, or lymphatic subcutaneous nodules.
It should be differentiated from lumbar disc herniation, acute suppurative arthritis, rheumatoid arthritis, lumbosacral subcutaneous nodules, osteitis condensans ilii, and metastatic cancer of the sacrum and ilium.





