| disease | Chronic Cor Pulmonale |
| alias | Chronic Cor Pulmonale, Lung Heart Disease, Obstructive Emphysematous Heart Disease |
The most common type of chronic pulmonary heart disease is chronic hypoxic pulmonary heart disease, also known as obstructive emphysematous heart disease, abbreviated as lung heart disease. It refers to a category of heart disease caused by chronic pathological changes in the lungs, thorax, or pulmonary arteries, leading to increased pulmonary circulation resistance, pulmonary hypertension, and right ventricular hypertrophy, with or without right heart failure. Lung heart disease is a common and frequently occurring condition in China. A decade ago, a nationwide survey of over 20 million people revealed an average prevalence rate of 0.4%. In 1992, a screening of over 100,000 farmers in certain areas of Beijing, Hubei, and Liaoning showed an average prevalence rate of 0.47%, largely consistent with previous findings. The prevalence is higher among populations living in high-altitude regions (such as Northeast, North, and Northwest China), the humid and sun-deficient Southwest, and among smokers. It also increases with age, with over 91.2% of patients aged 41 or older. There is no significant difference between genders. Prevalence varies by occupation, ranking highest among workers, followed by farmers and general urban residents, with the highest rates reaching 15.7% to 49.8%. This disease accounts for 46% to 38.5% of hospitalized heart disease cases. In most regions, it ranks third or fourth. At Zhongshan Hospital of Shanghai Medical University from 1980 to 1989, it constituted only 2.49%, ranking eighth, which is related to the increased incidence and hospitalization rates of coronary heart disease and myocarditis. In the frigid northern regions and the humid Southwest, it ranks first.
bubble_chart Etiology(1) Bronchopulmonary diseases are divided into two categories: ① Obstructive diseases, such as chronic bronchitis, bronchial asthma, and bronchiectasis, which are collectively referred to as chronic obstructive pulmonary disease (COPD). ② Restrictive diseases, such as diffuse pulmonary interstitial fibrosis, pulmonary subcutaneous nodules, pneumoconiosis, exposure to toxic gases (e.g., chlorine, carbon dioxide, nitrous oxide, etc.), extensive pulmonary fibrosis caused by chest radiation therapy, sarcoidosis, scleroderma, disseminated lupus erythematosus, dermatomyositis, idiopathic pulmonary hemosiderosis, etc.
(2) Diseases affecting respiratory activity include kyphoscoliosis and other thoracic deformities, post-thoracoplasty, pleural fibrosis, neuromuscular disorders (e.g., poliomyelitis, muscular dystrophy, etc.), and excessive obesity accompanied by alveolar ventilation disorders. Pulmonary blood vessels may become curved or twisted.
Additionally, chronic hypoxia in high-altitude sickness leading to prolonged pulmonary vasoconstriction is also a disease cause of lung heart disease.
bubble_chart Pathological Changes
Chronic hypoxic pulmonary heart disease has the following main pathological features:
(1) Bronchial lesions: Inflammation, thickening of the bronchial mucosa, hyperplasia of mucous glands, hypersecretion, dilation of acini with abundant secretions, retention of inflammatory exudates and mucus in the bronchial lumen, forming inflammatory or mucous plugs that cause obstruction. The bronchial ciliated epithelium is damaged to varying degrees, impairing its cleansing function. The lesions extend to the bronchioles, leading to smooth muscle hypertrophy, resulting in irregular narrowing of the lumen. Additionally, bronchospasm, destruction of cartilage, and collapse of the lumen during respiration contribute to partial or complete obstruction of the bronchioles.
(2) Alveolar lesions: Due to the aforementioned bronchial changes, impaired airflow leads to increased residual air volume and elevated pressure in the alveoli, causing overinflation. The alveolar walls passively dilate due to damaged elastic fibers, eventually rupturing and fusing several small alveoli into larger ones, forming emphysema.(3) Pulmonary vascular lesions: Chronic obstructive pulmonary disease often involves recurrent peribronchitis and pneumonia, which affect the bronchial arteries and nearby pulmonary artery branches. This results in varying degrees of arterial wall thickening, muscularization of small pulmonary arteries, hypertrophy of the tunica media, increased collagen types I and II, and fibrous thickening of the intima in small pulmonary arteries. Additionally, nonspecific pulmonary vasculitis and thrombosis may occur. In about 30% of patients, dilated collateral vessels may develop, leading to arteriovenous shunting.
(4) Cardiac lesions: Right ventricular hypertrophy, thickened ventricular walls, dilated cardiac chambers, bulging of the pulmonary conus, myocardial fiber hypertrophy and atrophy, interstitial edema, focal necrosis, and subsequent replacement by fibrous tissue. Some patients may also exhibit concurrent coronary atherosclerotic changes.
bubble_chart Clinical Manifestations
The disease progresses slowly and can be divided into two stages: compensation and decompensation, although the boundary between them is sometimes unclear.
(1) Functional Compensation Stage: Patients typically have a history of chronic cough, expectoration, or asthma, gradually developing weakness and dyspnea. Physical examination reveals significant signs of lung qi distension, including barrel chest, hyperresonance on lung percussion, lowered upper border of liver dullness, and diminished or even absent cardiac dullness. Auscultation shows diminished breath sounds, possibly with dry or moist rales, and faint heart sounds, sometimes audible only below the xiphoid process. The second heart sound is accentuated in the pulmonary stirred pulse area, and prominent cardiac pulsations are visible below the xiphoid in the upper abdomen, which are the main manifestations of cardiac involvement. Grade I jugular vein distension may be present, but venous pressure is not significantly elevated.
(2) Functional Decompensation Stage: Severe damage to lung tissue causes hypoxia and carbon dioxide retention, leading to respiratory and/or heart failure.1. Respiratory Failure: In the early stages of hypoxia, the main symptoms include cyanosis, palpitations, and chest tightness. As the condition worsens, hypoxemia and hypercapnia develop, leading to various neuropsychiatric symptoms, known as pulmonary encephalopathy. These symptoms include headache, head distension, dysphoria, restlessness, speech impairment, hallucinations, confusion, spasms, or tremors. When the stirred pulse blood oxygen partial pressure falls below 3.3 kPa (25 mmHg) and the stirred pulse blood carbon dioxide partial pressure exceeds 9.3 kPa (70 mmHg), central nervous system symptoms become more pronounced, manifesting as apathy, drowsiness, and eventually unconsciousness or death.
2. Heart Failure: This often occurs after acute respiratory infections and is frequently accompanied by respiratory failure. Patients exhibit panting, palpitations, oliguria, worsening cyanosis, upper abdominal distension and fullness, pain, loss of appetite, nausea, or even vomiting—symptoms of right heart failure. Physical examination reveals jugular vein distension, tachycardia, gallop rhythm or systolic murmurs due to relative tricuspid insufficiency in the precordial area, which may disappear as the condition improves. Various arrhythmias, particularly atrial arrhythmias, may occur, along with hepatomegaly and tenderness, positive hepatojugular reflux, edema, and ascites. Severe cases may lead to shock.
Additionally, since lung heart disease is a multi-organ disorder primarily affecting the heart and lungs, severe cases may present with renal insufficiency, disseminated intravascular coagulation, and pigmentation of the cheeks due to adrenal cortical insufficiency.
bubble_chart Auxiliary Examination
(1) Blood Tests Red blood cell count and hemoglobin are often elevated, hematocrit is normal or slightly high, whole blood viscosity, plasma viscosity, and platelet aggregation rate are frequently increased, red blood cell electrophoresis time is prolonged, and erythrocyte sedimentation rate (ESR) is generally accelerated. Arterial oxygen saturation is often lower than normal, and carbon dioxide partial pressure is higher than normal, becoming more pronounced during respiratory failure. In the heart failure stage, impaired liver and kidney function may manifest as elevated alanine aminotransferase, plasma urea nitrogen, creatinine, blood and urine β2-microglobulin (β2-M), plasma renin activity (PRA), plasma angiotensin II, and other markers. In cases of concurrent respiratory infection, white blood cell count may be elevated. During different stages of respiratory failure, changes such as hyperkalemia, hyponatremia, hypokalemia, hypochloremia, hypocalcemia, or hypomagnesemia may occur.
(2) Sputum Bacterial Culture Common pathogens include Streptococcus pneumoniae, Haemophilus influenzae, pneumococci, staphylococci, Neisseria, and viridans streptococci. In recent years, Gram-negative bacilli such as Pseudomonas aeruginosa and Escherichia coli have become more prevalent.
(3) X-ray Examination ① Pulmonary changes: Vary depending on the disease etiology, with pulmonary emphysema being the most common. ② Manifestations of pulmonary hypertension: The main pulmonary artery segment is prominent, and the hilar pulmonary arteries are dilated and elongated, along with the first branch of the pulmonary artery. Generally, if the transverse diameter of the first lower branch of the right pulmonary artery is ≥15 mm, or the ratio of the transverse diameter of the right lower pulmonary artery to the tracheal transverse diameter is ≥0.17, or dynamic observation shows the right lower pulmonary artery widening by more than 2 mm compared to the original, dilation of this branch can be considered. In severe pulmonary hypertension, the central pulmonary arteries dilate with enhanced pulsation, while the peripheral arteries abruptly narrow, appearing truncated or rat-tailed. ③ Cardiac changes: The heart is vertically positioned, so early-stage cardiac enlargement is not apparent. When the right ventricular outflow tract enlarges, the pulmonary conus becomes significantly prominent. Subsequently, the right ventricular inflow tract also hypertrophies and enlarges, with the cardiac apex tilting upward. Right atrial enlargement may sometimes be observed. In heart failure, generalized cardiac enlargement may occur, but the heart can return to its original size after heart failure is controlled. The left heart is generally not enlarged, though left ventricular enlargement may occasionally occur.
(4) Electrocardiogram (ECG) Right ventricular hypertrophy and/or right atrial hypertrophy are characteristic ECG changes in cor pulmonale. These changes are somewhat variable. During acute exacerbations, hypoxia, acidosis, alkalosis, and electrolyte imbalances can cause ST-segment and T-wave changes, as well as various arrhythmias. These abnormalities often resolve after the triggering factors are addressed and the condition improves. Common ECG changes include:
1. P-wave changes: The frontal P-wave axis is right-deviated between +70° and +90°. In leads II, III, and aVF, the P waves are tall and peaked, with amplitudes reaching 0.22 mV or higher, termed "P pulmonale." If the P wave exceeds 0.25 mV, the sensitivity, specificity, and accuracy of diagnosing cor pulmonale increase.
2. Changes in QRS complex and T wave The mean frontal plane QRS axis is rightward deviated ≥+90°. Sometimes, extreme right axis deviation may mimic left axis deviation with SⅠ, SⅡ, and SⅢ. Tall R waves appear in the right precordial leads. A deep S wave in V5 indicates significant right ventricular hypertrophy. Occasionally, a q wave may appear in leads V3R and V1, or QS and rS patterns may be present in leads V1 to V5. In patients with grade III lung qi, a transition from a normal ECG to incomplete right bundle branch block often suggests right heart overload and has certain diagnostic value. A very small number of patients may show ECG changes of left ventricular hypertrophy, possibly due to coexisting hypertension, coronary artery disease, or bronchial stirred pulse branch dilation with left-to-right shunting, leading to increased left ventricular output and hypertrophy. T wave inversions may occur in leads II, III, aVF, and the right precordial leads. Various arrhythmias may also appear. Additionally, limb lead low voltage and clockwise rotation are common ECG findings in lung heart disease, which are also seen in lung qi tumors; thus, these changes cannot be considered diagnostic of lung heart disease (Figure 1).
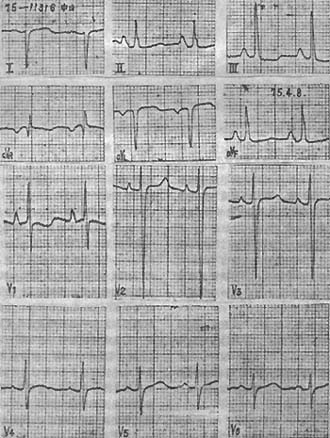
Figure 1 Electrocardiogram of chronic cor pulmonale
Illustration: Hypertrophy of the right atrium and right ventricle, right axis deviation, tall and peaked P waves in leads II, III, and aVF, PV1peaked at 3mm, aVR showing a qR pattern. V1 R/S ratio >1, deep S waves in V5and V6, R/S ratio nearly equal to 1, flattened T waves in leads II, III, and aVF.
(5) Vectorcardiogram Examination Main manifestations include right ventricular hypertrophy and/or right atrial enlargement. As the degree of right ventricular hypertrophy increases, the QRS axis shifts from the normal left, inferior, and anterior or posterior direction progressively to posterior, then inferior, and finally to right anterior, though the terminal portion remains right posterior. The QRS loop evolves from counterclockwise or figure-8 movement to grade III clockwise rotation. The P loop is often narrow, with increased amplitude in the left sagittal and frontal planes, and the maximum vector points anteriorly, inferiorly, left, or right. Generally, the more pronounced the right atrial hypertrophy, the more the P loop vector shifts to the right.
(6) Echocardiographic Examination Can reveal significant enlargement of the pulmonary artery diastolic diameter, increased diameter of the right pulmonary artery, widened right ventricular outflow tract with increased end-diastolic diameter, enlarged right ventricular cavity, thickened right ventricular anterior wall and interventricular septum, and enhanced pulsation amplitude (Figure 2). Doppler echocardiography may show tricuspid regurgitation and elevated right ventricular systolic pressure. Doppler spectral analysis can demonstrate shortened right ventricular ejection time and prolonged right ventricular pre-ejection period.
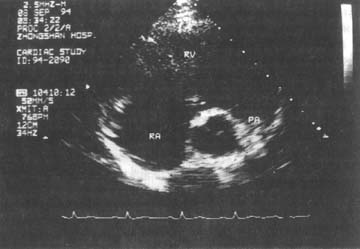
Figure 2 Two-dimensional echocardiogram of chronic cor pulmonale
Parasternal short-axis view at the great vessel level. Shows significant enlargement of the right ventricle and right ventricular outflow tract.
(7) Pulmonary Function Testing This test is not advisable during cardiopulmonary failure but may be considered during remission. Patients typically exhibit impaired ventilation and gas exchange, manifested as reduced timed vital capacity and maximum voluntary ventilation, and increased residual volume. Using a four-probe function instrument and γ-camera with intravenous bolus injection of radionuclide 133Xe, the half-clearance time of the upper and lower lung fields can reflect regional ventilation function, with a higher detection rate for lung heart disease compared to conventional pulmonary function tests.
(8) Right Heart Catheterization A floating catheter is inserted via the vein into the pulmonary artery to directly measure pulmonary artery and right ventricular pressures, which can aid in the early diagnosis of lung heart disease.
Additionally, pulmonary impedance plethysmography and its differential graph can reflect changes in pulmonary blood volume to some extent, providing insights into pulmonary hemodynamics, pulmonary artery pressure, and right heart function. Radionuclide cardiography helps assess right ventricular function changes. Lung perfusion scans showing increased blood flow in the upper lungs and decreased flow in the lower lungs suggest the presence of pulmonary artery hypertension.
This disease develops from chronic generalized pulmonary and thoracic conditions, with symptoms of the respiratory and circulatory systems often intermingled. Since it is difficult to determine whether heart disease has already manifested, early diagnosis is challenging. It is generally believed that in patients with chronic generalized pulmonary or thoracic diseases, once pulmonary arterial hypertension and right ventricular enlargement are detected while other possible causes of right heart enlargement are ruled out, the diagnosis of this disease can be established.
bubble_chart Treatment Measures
Since the vast majority of lung heart disease is a consequence of chronic bronchitis, bronchial asthma complicated by lung qi swelling, actively preventing and treating these conditions is the fundamental measure to avoid the occurrence of lung heart disease. Emphasis should be placed on hygiene, quitting smoking, and strengthening constitution to enhance overall resistance, thereby reducing the incidence of common cold and various respiratory diseases. For patients already suffering from lung heart disease, treatment should be tailored to the stage of remission and acute phase separately. Respiratory infections are a common trigger for respiratory failure and thus require active control.
**(1) Treatment During the Stage of Remission** This is key to preventing the progression of lung heart disease. The following approaches may be adopted: ① Cold-water rubdowns, diaphragmatic breathing, and pursed-lip exhalation to improve lung ventilation, along with cold tolerance and rehabilitation exercises. ② Symptomatic treatments such as cough suppression, dispelling phlegm, asthma relief, and anti-infection measures. ③ Immune-boosting medications, such as nucleic acid casein injections (or expired measles attenuated vaccine) administered subcutaneously or intramuscularly and/or via nebulization (2–4 ml per dose, twice weekly), or nucleic acid casein oral solution (10 ml per dose, three times daily for 3–6 months). Other options include subcutaneous injections of bronchitis vaccine, intramuscular immunoribonucleic acid or placental lipopolysaccharide, oral Ginseng, transfer factor, or levamisole. ④ Chinese medicine Chinese medicinals treatment. Chinese medicine views the primary symptom and sign of this disease as lung qi deficiency, mainly manifesting as pulmonary insufficiency. Treatment should focus on reinforcing healthy qi and securing the root, invigorating blood and resolving stasis to enhance the body’s resistance and improve pulmonary circulation. Herbs such as Tangshen, Astragalus Root, Coastal Glehnia Root, Ophiopogon Tuber, Salvia, and Carthamus may be selected. Rehabilitation therapy and home-based care for patients in the stage of remission can significantly reduce acute-phase episodes.
**(2) Acute Phase Treatment**
**1. Controlling Respiratory Infections** Respiratory infections are a common trigger for respiratory failure and heart failure, necessitating aggressive pharmacological intervention. Current practice favors combination therapy. Drug selection should ideally be guided by sputum culture and sensitivity testing, though not strictly bound by it. If the causative pathogen is unclear, options include penicillin (1.6–6 million units/day intramuscularly) or gentamicin (120,000–240,000 units/day, divided into intramuscular or intravenous doses). If efficacy is unclear after 2–3 days, alternative antibiotics such as ampicillin (2–6 g/day), carbenicillin (4–10 g/day), or lincomycin (1.2–2.4 g/day) may be administered intravenously or intramuscularly. Oral options include amoxicillin (2–4 g/day, divided doses). Cephalothin, cefazolin, or cefoperazone (2–4 g/day, divided intramuscular doses) or equivalent oral cephalexin may also be used. However, unnecessary frequent switching should be avoided. For Staphylococcus aureus infections, erythromycin plus chloramphenicol, oxacillin, cephalothin, or cefazolin combined with kanamycin or gentamicin may be employed. For Pseudomonas aeruginosa infections, combinations such as carbenicillin, sulbenicillin, furbenicillin, piperacillin, or ceftazidime with amikacin or gentamicin are recommended. In addition to systemic therapy, localized nebulization or endotracheal drug instillation may be used. Prolonged antibiotic use requires vigilance against fungal infections. If fungi become the primary pathogen, antibiotics should be adjusted or discontinued in favor of antifungal treatment.
**2. Improving Respiratory Function and Managing Respiratory Failure** Comprehensive measures include relieving bronchospasm, clearing sputum, ensuring airway patency, continuous low-concentration oxygen (24–35%), and respiratory stimulants. If necessary, moving qi tracheostomy, intubation, or mechanical ventilation may be employed. Recently, heparin (25–100 mg or 50 mg) combined with 654-2 (10 mg) in glucose solution has been administered intravenously for 7–10 days to reduce sputum and blood viscosity, relieve bronchospasm, and counteract allergies. However, prothrombin time should be monitored to avoid bleeding.
3. Managing Heart Failure For grade I heart failure, symptoms can be alleviated or eliminated by providing oxygen, improving respiratory function, and controlling respiratory tract infections. For more severe cases, adding diuretics can also achieve quicker control.
⑴The use of diuretics should generally involve intermittent, small doses of slow-acting agents in rotation, except in specific cases where potent, fast-acting preparations are needed. Besides reducing sodium and water retention, this approach can also improve abnormal blood gas levels. However, it should be noted that diuretics may cause hemoconcentration, thickening of sputum, and worsening airway obstruction, as well as electrolyte imbalances—particularly hypokalemia, hypochloremia, hypomagnesemia, and alkalosis—leading to refractory edema and arrhythmias. Therefore, when using potassium-depleting diuretics such as hydrochlorothiazide, bumetanide, or furosemide, potassium chloride supplementation or the addition of potassium-sparing diuretics like triamterene or spironolactone is necessary. Chinese herbal medicines such as the compound formula Wujianong Decoction, Plantain Seed, and Christina Loosestrife also have certain diuretic effects.
⑵Before respiratory function improves, the efficacy of digitalis drugs is poor, and the dose should be small to avoid toxic reactions, such as arrhythmias. Fast-acting and rapidly excreted preparations like lanatoside C (Cedilanid) or strophanthin K are preferred. For oral digitalis, a common regimen is digoxin 0.25 mg once daily. If heart failure remains inadequately controlled after small-dose digoxin, captopril 25–75 mg/d may be added in divided doses. Side effects such as hypotension, neutropenia, and proteinuria should be monitored.
⑶Vasodilators like phentolamine, an α-adrenergic receptor blocker, can be administered at 10–20 mg in 250–500 ml of 5% glucose solution, optionally with 50 mg heparin, as a slow intravenous drip once daily. Other effective drugs include sodium nitroprusside, nitroglycerin, nifedipine, dopamine, and dobutamine.
4. Management of Arrhythmias In addition to conventional treatment, attention should be paid to addressing the underlying causes, including infection control, hypoxia correction, and restoring acid-base and electrolyte balance. Arrhythmias often resolve spontaneously once the underlying cause is eliminated. Furthermore, when using antiarrhythmic drugs, β-adrenergic receptor blockers like propranolol should be avoided to prevent bronchospasm.
5. Use of Adrenocortical Hormones Under effective infection control, short-term high-dose adrenocortical hormones can play a role in rescuing early-stage respiratory or heart failure. Common regimens include hydrocortisone 100–300 mg or dexamethasone 10–20 mg in 500 ml of 5% glucose solution as a daily intravenous drip (dexamethasone may also be given as an IV push). Discontinue after 2–3 days if the condition improves. Use with extreme caution in cases of gastrointestinal bleeding.
6. Management of Complications Treat complications such as acid-base imbalance, electrolyte disturbances, gastrointestinal bleeding, shock, and disseminated intravascular coagulation (DIC).
7. Traditional Chinese Medicine Treatment In the acute stage of lung-heart disease, the condition manifests as root deficiency with excess manifestations and is highly variable. Treatment should follow the principles of "treating the tip in acute disease" and "treating both the tip and root."
⑴Lung-kidney qi deficiency with external contraction type (respiratory insufficiency with infection): - For cold predominance: Ventilate the lung, dispel cold, resolve phlegm, and relieve asthma. Modified Minor Green-Blue Dragon Decoction or True Warrior Decoction may be used. - For heat predominance: Clear heat and resolve phlegm, with adjunctive asthma relief. Modified Ephedra, Apricot Kernel, Gypsum, and Licorice Decoction combined with Shensu Drink or White-Draining Powder may be used.
⑵Heart-lung-kidney yang deficiency with water flooding type (predominantly cardiac insufficiency): Warm the kidney, fortify the spleen, promote diuresis, tonify qi, and calm the heart, with adjunctive blood activation and stasis resolution. Modified Poria, Cinnamon Twig, Atractylodes Macrocephala, and Licorice Decoction combined with True Warrior Decoction, Astragalus Root and Turtle Shell Powder, or Perilla Fruit Qi-Descending Decoction may be used. For dual deficiency of qi and yin (heart failure often accompanied by hyponatremia, hypokalemia, or hypoosmolarity): Nourish qi and yin with modified Pulse-Reinforcing Powder.
⑶Phlegm-turbidity clouding the orifices type (pulmonary encephalopathy): Clear heat, eliminate phlegm, open the orifices, and revive consciousness. Modified Nutrient-Clearing Decoction, Danxi’s Pubescent Angelica Decoction, or Phlegm-Cleansing Decoction may be used.
⑷Collapse of yang type (shock): Use Yang-Rescuing Emergency Decoction or Ginseng Alone Decoction.
(5) For the type of heat stasis damaging collaterals (with bleeding tendency), it is advisable to clear heat and cool blood, invigorate the blood to stop bleeding. Rhinoceros Horn and Rehmannia Decoction can be used in combination with Ten-Ash Powder, Jisheng Huisheng Pill, or Oven Yellow Earth Decoction with modifications. Additionally, for qi deficiency and fluid injury (treated with hormones, antibiotics, and diuretics in the late stage [third stage]), it is advisable to tonify qi, nourish yin, moisten dryness, and resolve phlegm, using Adenophora and Ophiopogon Decoction with modifications. Moreover, the integration of Chinese and Western medicine is an excellent therapeutic approach.
This disease persists year-round but often leads to respiratory failure and heart failure due to respiratory infections in winter, with a relatively high mortality rate. Before 1973, the in-hospital mortality rate for lung heart disease was around 30%. However, with enhanced prevention and treatment, it dropped below 15% by 1983 and has remained around 15% in the past 12 years. This is related to multiple factors, including the shift of the peak onset age to older populations, multi-organ complications, changes in infectious bacterial populations, and increased Pseudomonas aeruginosa infections. The main causes of death, in order, are pulmonary encephalopathy, respiratory failure, heart failure, shock, gastrointestinal bleeding, disseminated intravascular coagulation, and systemic failure. Most aspects of this disease are reversible. With appropriate treatment, cardiopulmonary function can recover to some extent. The occurrence of heart failure does not necessarily indicate that the myocardium has lost its contractile ability.
The most common are acid-base imbalance and electrolyte disturbances. Others include upper gastrointestinal bleeding and shock, followed by liver and kidney dysfunction and pulmonary encephalopathy. Rare complications include spontaneous pneumothorax and disseminated intravascular coagulation, the latter of which has a high mortality rate.
1. Coronary heart disease Both this disease and coronary heart disease are seen in elderly patients, and both can present with cardiac enlargement, arrhythmia, and heart failure. A few patients may exhibit Q waves in leads I, aVL, or chest leads on the electrocardiogram (ECG), resembling old myocardial infarction. However, lung heart disease lacks the typical clinical manifestations of heart disease or myocardial infarction. Additionally, there is often a history of chronic bronchitis, asthma, lung qi swelling, or other thoracic or pulmonary conditions. The ST-T changes on the ECG are usually not prominent, and the patterns resembling old myocardial infarction mostly occur during the acute stage of attack of lung heart disease and in cases of significant right heart failure. These patterns may disappear quickly as the condition improves.
2. Rheumatic heart disease Patients with lung heart disease may have a blowing systolic murmur audible in the tricuspid valve area, which may sometimes radiate to the apex. Occasionally, a blowing diastolic murmur due to pulmonary stirred pulse valve insufficiency may also be present. Combined with manifestations such as right heart hypertrophy and pulmonary stirred pulse hypertension, these findings can easily be confused with wind-dampness-related valvular membrane disease. Generally, a detailed history of chronic pulmonary or thoracic diseases, signs of lung qi swelling and right ventricular hypertrophy, along with findings from X-rays, ECG, vectorcardiogram, echocardiography, and significantly reduced stirred pulse oxygen saturation or elevated carbon dioxide partial pressure, can help differentiate the conditions.
3. Primary dilated cardiomyopathy and constrictive pericarditis The former often presents with a globular cardiac enlargement, frequently accompanied by heart failure and murmurs due to relative insufficiency of the atrioventricular valves. The latter manifests with palpitation, shortness of breath, cyanosis, jugular vein distension, hepatomegaly, ascites, edema, and low-voltage ECG, all of which require differentiation from lung heart disease. Generally, differentiation is not difficult based on medical history, X-rays, ECG, and other examinations. Additionally, in cases of obvious cyanosis with thoracic deformities, differentiation from various cyanotic congenital heart diseases is necessary. The latter often presents with characteristic murmurs, more pronounced clubbing of fingers, and absence of pulmonary edema, making differentiation relatively straightforward.
4. Other unconscious states In cases of pulmonary encephalopathy-related unconsciousness, differentiation is required from hepatic unconsciousness, uremic unconsciousness, and unconsciousness due to a few space-occupying sexually transmitted disease lesions or cerebrovascular accidents. These unconscious states generally have distinct clinical features of their primary diseases, making differentiation not particularly difficult. {|103|}




