| disease | Branchial Cleft Fistula |
| alias | Lateral Cervical Fistula |
A branchial cleft fistula is formed when a branchial pouch connects with a branchial groove or when the branchial groove fails to disappear. The external fistula opening and the entire course of the branchial cleft fistula are located in the neck, hence it is also called a lateral cervical fistula. The formation of a branchial cleft fistula is related to the following factors: ① rupture of the membrane between the branchial groove and the branchial pouch; ② incomplete closure of the branchial groove; ③ residual epithelium of the branchial organ; ④ abnormal development of the branchial organ; ⑤ non-closure of the cervical sinus. One or several of these factors may coexist.
bubble_chart Pathological Changes
The cyst or fistula is lined with stratified squamous epithelium, occasionally containing other epithelial components. The outer layer of the epithelium is surrounded by a connective tissue membrane, which is easily separated during surgery. The cystic cavity contains desquamated epithelium, mucus, and pus, often with cholesterol crystals.
Classification: Based on the different embryonic origins of branchial cleft fistulas, they can be divided into the following four types:
(1) First branchial cleft fistula: Relatively rare in clinical practice. Its external opening is usually located below the mandibular angle, near the anterior border of the upper end of the sternocleidomastoid muscle, on the lateral neck skin above the hyoid bone. The internal opening is located in the cartilaginous part of the external auditory canal or in front of or behind the auricle, the tympanic cavity, and the eustachian tube. The fistula runs below the eustachian tube, behind the tensor veli palatini muscle, and in front of the carotid artery or stylopharyngeus muscle, with some cases close to the facial nerve trunk.
(2) Second branchial cleft fistula: More common in clinical practice. The external opening is usually located at the junction of the middle and lower third of the anterior border of the sternocleidomastoid muscle. The fistula penetrates the platysma from the external opening, ascends along the carotid sheath, passes between the internal and external carotid arteries, crosses superficially to the glossopharyngeal nerve, stylopharyngeus muscle, and hypoglossal nerve, and reaches the upper part of the tonsillar fossa, where the internal opening is located.(3) Third branchial cleft fistula: Relatively rare. The external opening is located in the lower part of the anterior border of the sternocleidomastoid muscle, similar in position to that of the second branchial cleft fistula. The fistula penetrates deep to the platysma, passes behind the internal carotid artery, ascends superficially to the vagus nerve, crosses the hypoglossal nerve, and terminates at the internal opening in the pyriform fossa.
(4) Fourth branchial cleft fistula: Rare. The external opening is similar to that of the second branchial cleft fistula. The fistula penetrates deep to the platysma, descends along the carotid sheath to the chest, then ascends below the subclavian artery or aortic arch back to the neck, terminating at the internal opening in the upper esophagus.
bubble_chart Clinical Manifestations
The first branchial cleft fistula primarily manifests as ear discharge, with a mass below the mandibular angle {|###|} to be decocted later. Pressure on the mass increases ear secretions, and secondary infections may cause symptoms such as pain and fever.
The second, third, and fourth branchial cleft fistulas present with openings along the anterior border of the sternocleidomastoid muscle. Sometimes, these openings are very fine, as small as a needle tip or a tiny depression, often accompanied by slight discharge. Patients often perceive a foul odor in the mouth.
bubble_chart DiagnosisThe diagnosis is relatively easy to make based on medical history and typical clinical manifestations. First branchial cleft fistulas, often presenting with ear discharge, can be easily misdiagnosed as suppurative otitis media, so differentiation between the two is crucial. Second, third, and fourth branchial cleft fistulas are located at the junction of the middle and lower thirds of the anterior border of the sternocleidomastoid muscle, with external openings nearby and internal openings in the tonsillar fossa, pyriform fossa, or upper esophagus. Palpation along the external opening upward may reveal a firm, cord-like structure extending upward. X-ray contrast imaging with iodized oil through the fistula can confirm the diagnosis. Differential diagnosis should include subcutaneous nodular fistulas of the neck and fistulas caused by actinomycosis.
bubble_chart Treatment Measures
(1) Non-surgical therapy: Iodine oil, trichloroacetic acid, etc., can be used to cauterize the fistula, electrocauterize the fistula, or rinse the fistula with hydrochloric quinine or 25% sodium salicylate. These methods are mainly used as temporary measures for patients who are unsuitable for or need to delay surgical treatment.
(2) Surgical excision: This is the definitive treatment for branchial cleft fistula. The surgical procedure is as follows:
1. Incision: Make a spindle-shaped incision around the external fistula opening (Figure 1), cutting through the skin, subcutaneous tissue, and platysma muscle. Use tissue forceps to grasp the fistula opening and dissect along the periphery of the fistula deep into the carotid sinus. Then, make a transverse incision at the carotid sinus and pull out the freed lower half of the fistula through this incision (Figure 2).
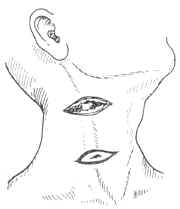
Figure 1: Incision for branchial cleft fistula excision
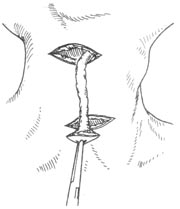
Figure 2: Pulling out the lower half of the fistula through the second incision
2. Fistula excision: Retract the sternocleidomastoid muscle outward to expose the carotid triangle, then dissect along the upper half of the fistula deep into the lateral pharyngeal wall at the tonsillar fossa (Figure 3). For third or fourth branchial cleft fistulas, dissect along the fistula tract to the pyriform fossa or upper esophagus. Excise the fistula, and if it communicates with the pharyngeal cavity, suture it immediately.
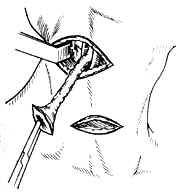
Figure 3: Continuing dissection along the fistula until reaching the tonsillar fossa
3. Close the wound layer by layer and place a drainage tube (Figure 4).
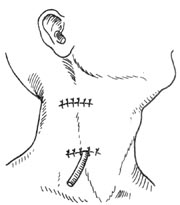
Figure 4: Wound closure and drainage tube placement




