| disease | Prickly-ash-like Sore (Trachoma) |
| alias | Trachoma |
Trachoma is a chronic infectious conjunctivitis and keratitis caused by Chlamydia. It is named "trachoma" because the surface of the palpebral conjunctiva becomes rough and uneven, resembling sand grains. The English term "trachoma" originates from the Greek word "trachys," which also means rough or uneven. In the early stages of the disease, the conjunctiva shows infiltration, such as papillae and follicle proliferation, along with corneal vascular pannus. In advanced stages, scarring of the affected palpebral conjunctiva leads to eyelid deformities like entropion, exacerbating corneal damage, which can severely impair vision or even cause blindness. Before liberation, trachoma was the leading cause of blindness in China. After liberation, under the care of the Party and government, extensive prevention and treatment efforts were carried out. With the improvement in living standards and healthcare conditions, the incidence of trachoma has significantly decreased. Epidemiological sampling surveys on blindness and low vision conducted in Shunyi County, Beijing, as well as Shanghai, Yunnan, and Shaanxi (1988) show that in most of these areas, the primary causes of blindness are non-infectious conditions such as cataracts and glaucoma. However, in Yunnan Province, among 180,000 bilateral blind patients, cataracts rank first, affecting approximately 80,000 people, while trachoma and its complications rank second, affecting about 30,000 people. Therefore, the significant role of trachoma as a cause of blindness in China cannot be overlooked. Additionally, this disease remains a major cause of blindness in many developing countries across Asia and Africa.
bubble_chart EtiologyThe secretion of prickly-ash-like sore (trachoma) can spread pestilence, which has long been known. In 1907, Halberstaedter and Von Prowazek used optical microscopy and Giemsa staining to discover inclusion bodies in the conjunctival epithelial cells of prickly-ash-like sore (trachoma). These inclusion bodies contained aggregates of red-blue elementary bodies and dark-blue initial body particles, surrounded by a matrix resembling an outer coat, leading to their mistaken designation as "Chlamydozoa." Subsequently, numerous studies were conducted, but the pathogen remained unisolated. In 1954, Tang Feifan and Zhang Xiaolou in China collaborated to examine and treat a large number of patients. They inoculated monkey eyes with secretions from patients' eyes and attempted to isolate and culture the pathogen by injecting prickly-ash-like sore (trachoma) secretions into mouse brains, but the results were entirely negative. In 1955, they switched to chick embryo inoculation, carefully selecting active, uncomplicated, and untreated prickly-ash-like sore (trachoma) cases. By using streptomycin to eliminate bacteria in the specimens, they finally succeeded in isolating and culturing the pathogen for the first time in 1956. This achievement sparked a new wave of global research on prickly-ash-like sore (trachoma). Because this pathogen could pass through bacterial filters, resided intracellularly, and formed inclusion bodies, it was initially considered a virus. However, due to its size and morphology differing from typical viruses, it was termed an atypical or large virus. Further studies by researchers worldwide on its molecular biology and metabolic functions revealed that it possessed both RNA and DNA, certain enzymes, reproduced by binary fission, had a cell membrane and wall, and was sensitive to antibiotics—properties inconsistent with the fundamental characteristics of viruses. Instead, it showed significant similarities to Gram-negative bacteria. In 1971, Storz and Page proposed classifying these microorganisms into a new order, Chlamydiales. The 1974 edition of *Bergey's Manual of Determinative Bacteriology* adopted this classification, placing them in the kingdom Prokaryotae, phylum Gracilicutes, class Rickettsiae, order Chlamydiales, family Chlamydiaceae, genus *Chlamydia*, and species *Chlamydia*, including the prickly-ash-like sore (trachoma) inclusion conjunctivitis species and the psittacosis species. The 10th edition of the manual, published in 1989, added the pneumonia species. The prickly-ash-like sore (trachoma) inclusion conjunctivitis species was further divided into three biovars: prickly-ash-like sore (trachoma), lymphogranuloma, and mouse pneumonia. Among these, the prickly-ash-like sore (trachoma) biovar was subdivided into 12 immunotypes based on strain resistance: A, B, Ba, C, D, E, F, G, H, I, J, and K, while the lymphogranuloma biovar was divided into three immunotypes: L1
prickly-ash-like sore (trachoma) Chlamydia can infect the conjunctival membrane and corneal epithelial cells of humans. In its life cycle, there are two biological phases: the elementary body is the infectious phase, measuring about 0.3μm in size, possessing a cell wall, and capable of surviving outside cells; the initial body, also known as the reticulate body, is the reproductive phase, larger in size (about 0.8μm) and non-infectious. After invading host cells, the elementary body develops and transforms into an initial body within the cytoplasm, then divides by binary fission to form progeny elementary bodies. Once the cytoplasm is filled, the cell ruptures and releases elementary bodies, which then invade normal epithelial cells to begin a new cycle. Each cycle lasts approximately 48 hours.
prickly-ash-like sore (trachoma) Primary infection may heal without leaving scars. However, in endemic areas with poor sanitary conditions, reinfection is common. The primary infection sensitizes the conjunctival tissue to the chlamydia of prickly-ash-like sore (trachoma), and when re-exposed to the chlamydia of prickly-ash-like sore (trachoma), it triggers a delayed hypersensitivity reaction. During the chronic sexually transmitted disease course of prickly-ash-like sore (trachoma), acute episodes often occur, which may be manifestations of reinfection. Multiple recurrent infections exacerbate the existing prickly-ash-like sore (trachoma) vascular nebula and scar formation, even leading to thickening and deformation of the tarsal plate, causing entropion and trichiasis, worsening corneal opacity, impairing vision, and even causing blindness. In addition to reinfection, concurrent bacterial infections can also aggravate the condition.bubble_chart Pathological Changes
The chlamydia only invades the epithelial cells of the palpebral conjunctiva and fornix conjunctiva, but the pathological changes it causes extend to deep tissues. Initially, the superficial epithelial cells degenerate and shed, while the deeper ones proliferate. As the disease progresses, the epithelial cells proliferate rapidly, causing the epithelial layer to lose its smoothness and form papillae. The papillae contain dilated capillaries, lymphatic vessels, and lymphocytes within their substance. Simultaneously, diffuse lymphocyte infiltration occurs in the subepithelial tissue of the conjunctiva, along with localized aggregation, forming follicles. The central part of the follicles contains many lymphoblasts, macrophages, and reticular cells, surrounded by a large number of small lymphocytes. As the disease advances, the follicles undergo degeneration and necrosis, followed by connective tissue proliferation, leading to scar formation. The tarsal plate also exhibits diffuse lymphocyte infiltration, resulting in thickening. In severe cases, connective tissue proliferation causes deformation. Corneal vascular pannus typically begins at the superior corneal limbus, with dilated capillaries extending toward the central cornea, accompanied by cellular infiltration. Initially, this occurs in the superficial layers, but later extends to the lower and deeper layers of the cornea. Early manifestations appear as a curtain-like pattern, and in severe cases, the entire cornea may be affected.
bubble_chart Clinical Manifestations
The incubation period is approximately 5 to 12 days. It usually affects both eyes and mostly occurs during childhood and adolescence.
1. Symptoms The onset is often acute, with patients experiencing a foreign body sensation, photophobia, tearing, and a significant amount of mucus or mucopurulent discharge. After a few weeks, the acute symptoms subside, entering the chronic phase, during which there may be no discomfort or only mild eye fatigue. If treated or self-healed at this stage, no scarring may remain. However, in endemic areas, repeated infections during the chronic sexually transmitted disease course can worsen the condition. When active vascular nebula appears on the corneal membrane, the irritation symptoms become more pronounced, and vision may decline. In the advanced stage, due to sequelae such as entropion, trichiasis, corneal membrane ulcer, and dry eye, symptoms become more severe and significantly impair vision, potentially leading to blindness.
2. Signs
(1) Acute prickly-ash-like sore (trachoma): Presents with acute follicular conjunctival membrane inflammation, eyelid redness and swelling, severe conjunctival membrane congestion, rough and uneven palpebral conjunctival membrane due to papillary hyperplasia, and follicles covering the upper and lower fornix conjunctival membranes. It may also involve diffuse corneal membrane epithelial inflammation and preauricular lymphadenopathy. After a few weeks, the acute inflammation subsides, transitioning to the chronic phase.
(2) Chronic prickly-ash-like sore (trachoma): Due to repeated infections, the course may extend for several years to over a decade. Although congestion lessens, there is diffuse cellular infiltration in the subcutaneous tissue, making the conjunctival membrane appear dirty and thickened, accompanied by papillary hyperplasia and follicle formation (Figure 1). Follicles vary in size and may appear gelatinous, with the most prominent lesions occurring in the upper fornix and the conjunctival membrane near the upper tarsal plate. Similar lesions may also appear on the lower palpebral conjunctival membrane and lower fornix conjunctival membrane, and in severe cases, may even affect the semilunar fold. Corneal membrane vascular nebula: This occurs when the normal capillary network at the corneal limbus extends into the transparent corneal membrane, impairing vision and gradually progressing toward the pupillary area, accompanied by cellular infiltration and the development of superficial small ulcers. Healing may result in small corneal facets. Severe cellular infiltration can lead to thick, fleshy vascular nebula (pannus crassus).

Figure 1: Prickly-ash-like sore (trachoma) follicles
During the chronic sexually transmitted disease course, conjunctival membrane lesions are gradually replaced by connective tissue, forming scars. The earliest scars appear as horizontal white streaks in the subtarsal groove of the upper palpebral conjunctival membrane, later becoming网状. Once the active sexually transmitted disease changes completely subside, the affected conjunctival membrane becomes entirely white and smooth scar tissue (Figure 2).
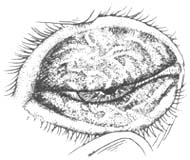
Figure 2: Prickly-ash-like sore (trachoma) scars
The course and prognosis of prickly-ash-like sore (trachoma) vary depending on the severity of infection and whether there are repeated infections. Mild cases or those without reinfection may heal within months, leaving minimal or no noticeable scarring. Severe cases with repeated infections may persist for years to over a decade. During the chronic sexually transmitted disease phase, other bacterial infections or reinfections can trigger acute flare-ups. Eventually, extensive scarring occurs, eliminating the pestilence nature of the disease, but severe complications and sequelae often lead to vision impairment or even blindness.
For the prevention, treatment, and research of prickly-ash-like sore (trachoma), various clinical staging methods have been developed. In 1979, China's Second National Ophthalmology Academic Conference revised the staging of prickly-ash-like sore (trachoma) as follows:
Stage I — Stage of progress (active phase): Papillae and follicles coexist, with blurred conjunctival membrane tissue in the upper fornix and corneal membrane vascular nebula.
Stage II — Stage of retrogress: Scars begin to appear until most of the tissue becomes scarred, with only minor active sexually transmitted disease changes remaining.
Stage III — Complete scarring phase: Active sexually transmitted disease changes disappear entirely, replaced by scars, with no pestilence activity.
Additionally, a grading standard was established based on the extent of active sexually transmitted disease changes (papillae and follicles) relative to the total area of the upper palpebral conjunctival membrane: - Mild (+): Affecting less than 1/3 of the area. - Moderate (++): Affecting 1/3 to 2/3 of the area. - Severe (+++): Affecting more than 2/3 of the area.
and established a grading method for corneal membrane vascular nebula: dividing the corneal membrane into four equal parts. Those with vascular nebula invading the upper 1/4 are graded as (+), reaching 1/4 to 1/2 as (++), reaching 1/3 to 3/4 as (+++), and exceeding 3/4 as (++++) (Figure 3).

Figure 3 Corneal membrane vascular nebula
1. Normal blood vessels do not invade the transparent corneal membrane. 2. Vascular nebula (+)
3. Vascular nebula (++) 4. Vascular nebula (+++) 5. Vascular nebula (++++)
The internationally more commonly used method is the MacCallan staging system:
Stage I – Infiltration initial stage [first stage]: Congestion and hypertrophy of the palpebral conjunctiva and fornix conjunctiva, especially in the upper part, with possible initial stage [first stage] follicles and early corneal vascular nebula.
Stage II – Active stage: There are obvious active sexually transmitted disease changes, namely papillae, follicles, and corneal vascular nebula.
Stage III – Pre-scarring stage: Same as China's Stage II.
Stage IV – Complete scarring stage: Same as China's Stage III.
The typical prickly-ash-like sore (trachoma) is relatively easy to diagnose clinically based on the presence of papillary and follicular hyperplasia on the palpebral conjunctiva, corneal vascular nebula, and conjunctival scarring. However, diagnosing early-stage prickly-ash-like sore (trachoma) can still be somewhat challenging. Sometimes, it can only be preliminarily diagnosed as "suspected prickly-ash-like sore (trachoma)." According to the 1979 decision by the Ophthalmology Branch of the Chinese Medical Association, the diagnostic criteria for prickly-ash-like sore (trachoma) are as follows: ① Blurred vascular congestion, papillary hyperplasia, or follicular formation, or both, in the upper fornix and upper tarsal conjunctiva. ② Corneal vascular nebula visible under a magnifying lens or slit lamp. ③ Scarring in the upper fornix and/or upper palpebral conjunctiva. ④ Inclusion bodies of prickly-ash-like sore (trachoma) found in conjunctival scrapings. Based on the first criterion, if any one of the other three criteria is also met, a diagnosis of prickly-ash-like sore (trachoma) can be made.
Suspected prickly-ash-like sore (trachoma): Conjunctival congestion in the upper fornix and canthus, with slight papillary (papillae are normal tissue) hyperplasia or follicles, and other forms of conjunctivitis have been ruled out.
bubble_chart Treatment Measures
Since the application of sulfonamides and antibiotics, significant progress has been made in the treatment of prickly-ash-like sore (trachoma). Experimental studies have demonstrated that rifampicin, tetracycline, chlortetracycline, oxytetracycline, erythromycin, sulfonamides, and chloramphenicol can inhibit the chlamydia of prickly-ash-like sore (trachoma).
1. Topical medication 0.1% rifampicin or 0.5% chlortetracycline or tetracycline eye drops administered 3–6 times daily show good efficacy. However, these drugs gradually lose effectiveness within weeks after being dissolved in water and must be freshly prepared. If formulated as an eye medicinal paste or suspension, they can be preserved for a longer period. 10–30% sulfonamide vinegar sodium and 0.25%–0.5% chloramphenicol eye drops are easy to store and also effective. The aforementioned medications generally require continuous use for 1–3 months. Intermittent therapy is also feasible, where medication is administered for 3–5 days, followed by a 2–4 week break before resuming treatment. This approach is equally effective and easier to adhere to. For cases where most of the lesion has scarred but residual papillary proliferation ("small islands") remain, a copper sulfate stick can be used for cauterization to promote scarring.
2. Systemic treatment For acute or severe prickly-ash-like sore (trachoma), in addition to topical eye drops, adults may take oral sulfonamide preparations. A treatment course consists of continuous administration for 7–10 days, followed by a 1-week break before repeating. Two to four courses are typically required, and attention should be paid to the side effects of the drugs.
3. Surgical treatment For severe papillary proliferation, drug friction can be performed using a cotton swab or cuttlebone stick dipped in sulfonamide or tetracycline to rub the palpebral conjunctiva and fornix. For cases with numerous follicles, expression surgery can be performed under local anesthesia, where a ring forceps is used to rupture the follicles and expel their contents, combined with drug therapy to promote healing. For sequelae such as a few ingrown eyelashes, electrolysis can be performed. For entropion with ingrown eyelashes, surgical correction is required.
prickly-ash-like sore (trachoma) Chlamydia often attaches to the eye secretions of patients, and any contact with these secretions can create an opportunity for the transmission and infection of prickly-ash-like sore (trachoma).
Therefore, it is essential to strengthen publicity and education, disseminate knowledge on preventing and treating eye diseases to the public, and implement the principle of prevention first. Cultivate good hygiene habits. Avoid rubbing eyes with hands; towels and handkerchiefs should be washed frequently and dried in the sun. Collective units such as nurseries, schools, and factories should use separate basins and towels or water from rivers for face washing. Patients with prickly-ash-like sore (trachoma) should receive active treatment. Strengthen hygiene management in service industries such as barbershops, bathhouses, and hotels, strictly enforce disinfection protocols for towels and washbasins, and pay attention to the cleanliness of water sources.
1. Conjunctival folliculosis is commonly seen in children, always bilateral, with no subjective symptoms. Follicles are mostly found in the lower fornix and lower palpebral conjunctiva. The follicles are small, uniform in size, translucent, and clearly demarcated, with normal conjunctiva between the follicles, no congestion, no corneal vascular nebula, and no scarring. The follicles of prickly-ash-like sore (trachoma) are mostly found in the upper fornix and upper palpebral conjunctiva, appearing turbid, uneven in size, and irregularly arranged, accompanied by symptoms such as conjunctival congestion and hypertrophy.
2. Chronic follicular conjunctivitis is commonly seen in school-age children and adolescents, always unilateral, and Bacillus granulosis may be the causative agent. There is often discharge in the morning, with a feeling of ocular discomfort. Follicles are mostly found in the lower fornix and lower palpebral conjunctiva, uniform in size and neatly arranged. Although the conjunctiva is congested, it is not hypertrophic. The condition resolves spontaneously within 1–2 years without scarring or corneal vascular nebula.
3. Vernal conjunctivitis is seasonal, with the main symptom being itching. The papillae on the palpebral conjunctiva are large, flat, and hard, with no lesions in the upper fornix, making it easy to differentiate. Increased eosinophils can be observed in the secretion smear.
4. Inclusion conjunctivitis: Both adult and neonatal inclusion conjunctivitis show inclusions in conjunctival scrapings, which are morphologically identical to those of prickly-ash-like sore (trachoma) and difficult to distinguish. However, inclusion conjunctivitis always begins acutely, with follicles predominantly in the lower fornix and lower palpebral conjunctiva, no corneal vascular nebula, and spontaneous resolution within several months to a year without scarring, allowing differentiation from prickly-ash-like sore (trachoma). {|103|}






