| disease | Simple Periodontitis |
| alias | Simple Periodontitis |
Simple periodontitis refers to a chronic inflammation of the periodontal supporting tissues primarily caused by local factors. It is more commonly seen after the age of 35, hence also known as adult periodontitis. It often develops from gingivitis; if gingivitis is not treated promptly, the inflammation can spread from the gums to deeper layers, affecting the periodontal membrane, alveolar bone, and cementum, leading to periodontitis. Since early symptoms are often not obvious and easily overlooked, by the time symptoms prompt a visit to the doctor, the condition is often severe, and sometimes the teeth cannot be saved. Therefore, it is essential to enhance education to encourage early consultation and timely treatment.
bubble_chart Etiology
1. Plaque refers to the microbial community adhering to the surface of teeth, which cannot be removed by rinsing or water flushing.
2. Dental calculus is mineralized plaque deposited on the tooth surface. Dental calculus is further divided into supragingival calculus and subgingival calculus based on its deposition site and properties.
1) Supragingival calculus is located on the tooth surface above the gingival margin and can be directly seen with the naked eye. It deposits more at the neck of the tooth, especially opposite the openings of the major salivary gland ducts, such as the buccal side of the maxillary molars and the lingual side of the mandibular anterior teeth. The main sources of inorganic salts in supragingival calculus are calcium, phosphorus, and other mineral salts from saliva.
2) Subgingival calculus is located below the gingival margin, on the root surface within the gingival sulcus or periodontal pocket, and cannot be directly seen with the naked eye. It must be probed to determine its deposition site and amount. Subgingival calculus can form on any tooth but is more common on the proximal and lingual surfaces. Subgingival calculus is mainly provided with mineral salts by gingival crevicular fluid and exudates.
The harm of dental calculus to periodontal tissues is mainly that it provides a favorable environment for plaque attachment and bacterial growth. Dental calculus itself hinders the maintenance of oral hygiene, thereby accelerating plaque formation and irritating the gingival tissues.3. Traumatic occlusion occurs when the occlusal force is too large or the direction is abnormal, exceeding the combined force that the periodontal tissues can withstand, causing injury to the periodontal tissues. Traumatic occlusion includes premature contact during occlusion, occlusal interference, and nocturnal bruxism.
4. Other factors, including food impaction, poor restorations, and mouth breathing, also contribute to the inflammatory process of periodontal tissues.
bubble_chart Clinical Manifestations
Early symptoms are often not obvious, and patients may only experience spontaneous gingival bleeding or fetid mouth odor, which is similar to symptoms of gingivitis. Upon examination, swelling of the gingival margin, gingival papilla, and attached gingiva can be observed, with a soft texture and a deep red or dark red color. Probing easily causes bleeding. As the inflammation further spreads, the following symptoms appear:
Periodontal pocket formation: Due to the expansion of inflammation, the periodontal membrane is destroyed, the alveolar bone is gradually absorbed, and the gingiva separates from the tooth root, deepening the gingival sulcus and forming a periodontal pocket. The depth of the periodontal pocket can be measured with a probe. X-ray examination may reveal varying degrees of alveolar bone absorption, as shown in Figures 2-6.
Periodontal pus discharge: The wall of the periodontal pocket develops ulcers and inflammatory granulation tissue, and purulent secretions accumulate within the pocket. Therefore, light pressure on the gingiva may cause pus discharge, often accompanied by fetid mouth odor.
Tooth loosening: Due to the destruction of periodontal tissues, especially with increased alveolar bone absorption, the support for the teeth becomes insufficient, leading to tooth loosening and displacement.At this stage, patients often experience weak bite, dull pain, increased gingival bleeding, and worsened fetid mouth odor. When the body's resistance decreases and the drainage of periodontal pocket fluid is obstructed, periodontal abscesses may form. The gingiva then appears as an oval-shaped protrusion, red and swollen, with increased tooth mobility and percussion pain. Patients may feel intense throbbing pain locally, and sometimes multiple abscesses may occur simultaneously, known as multiple periodontal abscesses. At this point, patients may also experience elevated body temperature, general discomfort, and swollen, tender submandibular lymph nodes.
|
|
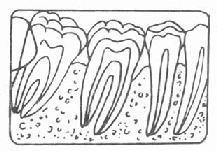
Figure 2: Normal alveolar bone | Figure 3: Grade I alveolar bone absorption |
|
|
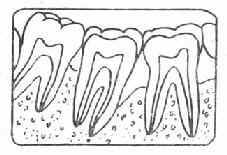
Figure 4: Grade II alveolar bone absorption | Figure 5: Grade III alveolar bone absorption |
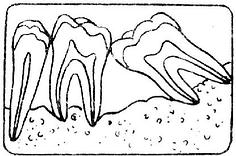 | |
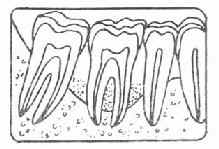
Figure 6: Grade IV alveolar bone absorption | |
Simple periodontitis, also known as marginal periodontitis, is a chronic inflammation of the periodontal tissues that develops from chronic gingivitis. In terms of disease cause, simple periodontitis is fundamentally similar to simple gingivitis, but the extent and severity of the lesions are greater.
1. Medical history: There is often a history of gingivitis, with the incidence increasing after the age of 30-40 and gradually worsening.
2. The color and shape of the gums are similar to those of gingivitis, with attached gingival edema and loss of stippling.
3. Upon probing, loss of periodontal attachment can be observed, forming periodontal pockets, and the teeth may have varying degrees of looseness, with severe cases leading to periodontal abscesses.4. Local factors such as plaque, calculus, food impaction, or poor restorations may be present.
5. The extent of periodontal tissue destruction can be determined using indices such as the Periodontal Index (PI) and the Periodontal Disease Index (PDI).
6. X-rays may show varying degrees of alveolar bone resorption. In severe cases, tooth mobility and occlusal relationship disorders may occur.
7. When occlusal trauma factors are also present, it is referred to as complex periodontitis. Examination may reveal premature contacts, malocclusion, occlusal interferences during protrusive or lateral movements, excessive wear, and other phenomena.
bubble_chart Treatment Measures
Local Treatment
1. For local irritants, supragingival scaling (Figure 1) or subgingival scaling can be performed. If necessary, adjust the occlusion, eliminate food impaction, and correct poor restorations.
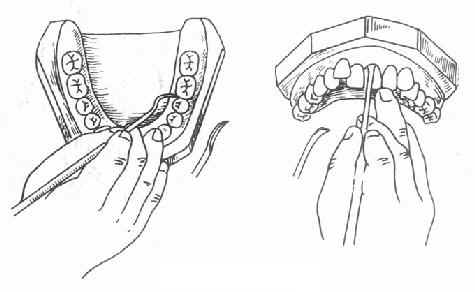
Figure 1 Dental Calculus Removal
2. Treatment of periodontal pockets: When there is pus discharge from the periodontal pocket, it can be rinsed with 1-3% hydrogen peroxide solution, and 10% iodine mixture, spiramycin, metronidazole, or other medications can be placed inside the pocket. After removing local factors, shallow pockets can be cauterized with iodine phenol solution. Deeper pockets require periodontal surgery to eliminate periodontitis. If the periodontal pocket reaches the root apex and the tooth is significantly loose, extraction may be considered.
3. Loose tooth fixation: After the above treatments, if the inflammation has been eliminated but the tooth is still loose, temporary or permanent periodontal splints can be used to stabilize the loose tooth.
4. Treatment of periodontal abscess: When the abscess is localized, it can be incised and drained. The periodontal pocket should also be rinsed and medicated with membrane or iodine glycerin.
Systemic Treatment
Mainly involves enhancing systemic resistance and actively treating systemic diseases related to periodontitis. For patients with severe systemic reactions due to periodontal abscess, oral antibiotics should be administered to control infection, and rest should be emphasized.
Chinese Medicine Pattern Identification and Treatment.
Traditional Chinese medicine has long documented the understanding of periodontal diseases and emphasizes pattern identification and treatment. For example:
1. Kidney Yin Deficiency Type: It is advisable to enrich yin and tonify the kidney, using modified Liuwei Dihuang Decoction.
2. Kidney Yang Deficiency Type: It is advisable to warm and tonify kidney yang, using modified Fuguibaihu Decoction.
3. Stomach Meridian Excess Fire Type (Periodontal Abscess): It is advisable to clear stomach fire, using modified Stomach-Clearing Decoction.
In summary, the treatment of periodontitis is completed through a series of comprehensive treatment measures. To consolidate the efficacy and prevent recurrence, oral hygiene education should be conducted, regular follow-ups should be scheduled, and appropriate treatments such as plaque and calculus removal or medication should be administered as necessary.
In the early stages of simple periodontitis, attention should be paid to distinguishing it from marginal gingivitis.
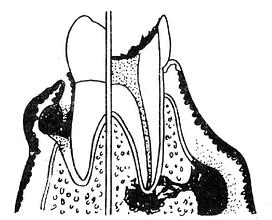
When periodontal abscess occurs, it should be differentiated from alveolar abscess (Figure 7, 8, Table 1).
|
|
Figure 7 Differences between gingivitis and periodontitis | Figure 8 Differentiation between periodontal abscess and alveolar abscess |
Table 1 Differential diagnosis of periodontal abscess and alveolar abscess
| Periodontal abscess | Alveolar abscess | |
| Location of abscess | Periodontal pocket area | Apical area near the vestibular sulcus |
| Condition of the tooth crown | Generally no caries | Presence of caries or other dental diseases |
| Periodontal pocket | Present | Absent |
| Tooth mobility | Present | May be present |
| Pulp vitality | Present | Absent |
| X-ray findings | Alveolar bone resorption, normal periapical area | No change in alveolar ridge, periapical area shows bone rarefaction |