| disease | Jaw Fracture |
| alias | Fracture of the Jaw |
Mandibular fractures include maxillary fractures and mandibular fractures, which are divided into open fractures and closed fractures. Based on the cause of injury, they can also be classified into firearm injuries and non-firearm injuries.
bubble_chart Clinical Manifestations
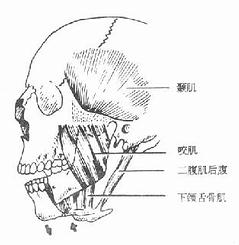
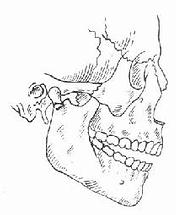
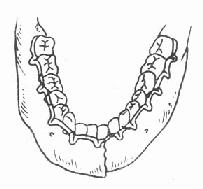
Based on the anatomically weak areas, there are three classic types of maxillary fractures (Figure 8). The first type (LeFort I fracture) has a fracture line passing through the lower edge of the piriform aperture, the lower part of the maxillary sinus, and extending horizontally to both maxillary tuberosities. The second type (LeFort II fracture) has a fracture line passing through the nasal bone, lacrimal bone, orbital floor, and below the zygomatic bone, reaching the posterior wall of the maxilla. The third type (LeFort III fracture) also has a fracture line passing through the nasal bone and lacrimal bone but crosses the orbital cavity and above the zygomatic bone, extending backward to the posterior wall of the maxilla, completely separating the maxilla and zygomatic bone from the skull, hence also termed craniofacial separation. The mandible is the only movable bone in the head and also has its own weak areas anatomically, such as the midline mental region, mental foramen area, mandibular angle, and condylar neck, which are common sites for mandibular fractures (Figure 9). Due to its prominent position and anatomical shape, the mandible has the highest incidence of fractures in the maxillofacial region.
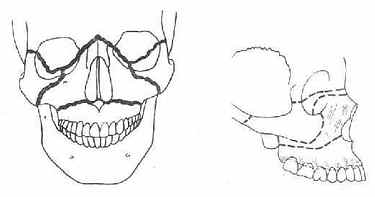
①Frontal view ②Lateral view
Figure 8 Three types of maxillary fractures
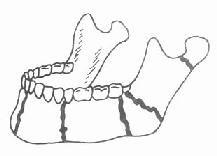
Figure 9 Common sites of mandibular fractures
Compared to other fractures, maxillofacial fractures share some common clinical symptoms, such as local pain, swelling, abnormal mobility or displacement of the fractured ends, and dysfunction, but they also have unique clinical characteristics determined by the anatomical and physiological structure of the jaw.
1. Displacement of fracture segments: The displacement of fractured segments in jaw fractures mainly depends on the type of fracture, direction of impact, muscle traction, and the weight of the fractured segment itself.In cases of transverse maxillary fractures, the fractured segment often droops due to gravity. If the impact direction is from front to back, the fractured segment may shift backward, causing midface depression; impacts from below upward often result in impacted fractures.
Displacement of mandibular fracture segments is primarily caused by muscle traction. In fractures at the mental foramen, the anterior segment is often pulled downward by the depressor muscles, while the posterior segment is pulled upward by the elevator muscles (Figure 10). In comminuted fractures of the mental region, the middle segment may be pulled backward by the genioglossus and geniohyoid muscles. The bilateral fracture segments are pulled toward the midline by the mylohyoid and hyoglossus muscles, narrowing the anterior arch of the mandible. Such fractures can cause tongue retraction, leading to respiratory distress or even asphyxia, requiring special attention. Condylar fractures are often caused by indirect force and may occur simultaneously with mental fractures, necessitating careful examination to avoid misdiagnosis. After a condylar fracture, the segment is often pulled anteromedially by the lateral pterygoid muscle, while the mandibular ramus is pulled upward by the elevator muscles, resulting in an inability to close the anterior teeth. Bilateral condylar fractures exacerbate this anterior open bite (Figure 11).
|
|
Figure 10 Displacement of fracture segments after mental foramen fracture | Figure 11 Displacement of the fractured segment after condylar fracture |
2. Malocclusion: The occlusal relationship between the upper and lower teeth is often disrupted due to the displacement of the fractured segments of the jawbone. This is the most obvious symptom of jawbone fractures and holds significant importance in diagnosis. In cases of transverse maxillary fractures, the fractured segment shifts downward, causing premature contact between the upper and lower posterior teeth and resulting in an open bite in the anterior teeth. Mandibular fractures frequently lead to malocclusion due to the displacement of the fractured segments. If there is no displacement of the fractured segments, the occlusion shows no significant disruption.
3. Abnormal mobility of fractured segments: The maxilla is an immobile bone; if mobility is observed, it is a sign of fracture. The mandible normally moves as a whole through the joint. The presence of segmented abnormal movement indicates a fracture.
4. Abnormal sensations: In maxillary fractures, if the infraorbital nerve is injured, numbness may occur in the infraorbital region, upper lip, and nose. In mandibular fractures, if the inferior alveolar nerve is injured, numbness may be present in the ipsilateral lower lip.
5. Restricted mouth opening: After a jawbone fracture, mouth opening may be limited due to pain, displacement of fractured segments, incoordination of masticatory muscles, reflexive spasms, or temporomandibular joint injuries. Mandibular fractures, in particular, have a greater impact on mouth opening.
6. Impaired breathing and swallowing: Jawbone fractures may affect breathing and swallowing functions due to the displacement of fractured segments.
7. Visual disturbances: Fractures of the maxilla or zygoma involving the orbital region can lead to diplopia if the eyeball is displaced. Injury to the oculomotor nerve or muscles may result in abnormal eye movement.
The diagnosis of a jaw fracture should first involve understanding the cause of injury, the exact location of the direct trauma, and the circumstances of the injury. Following this, a thorough examination of local and systemic signs should be conducted. Based on the clinical features mentioned above, the presence of a fracture, its location, and type should be determined. If conditions permit, further X-ray and CT examinations can be performed to obtain detailed information about the fracture line's location, number, direction, and displacement. It is crucial to emphasize that the examination should be comprehensive to avoid missing any fistulous diseases. For diagnosing multiple injuries to the maxillofacial region and systemic trauma, a complete assessment is essential to provide a solid foundation for developing a comprehensive treatment plan.
bubble_chart Treatment Measures
After a jaw fracture, the primary treatments are reduction and fixation. The key indicator for successful reduction of a jaw fracture is the restoration of the normal occlusal relationship between the upper and lower teeth, i.e., the broad contact relationship of the teeth. Otherwise, it will affect the recovery of masticatory function after the fracture heals. There are three commonly used reduction methods:
1. Manual reduction: In the early stages of a jaw fracture, when the fractured segments are still relatively mobile, the displaced segments can be manually repositioned to their normal alignment.
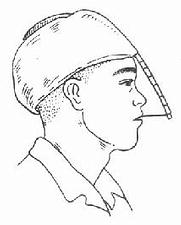
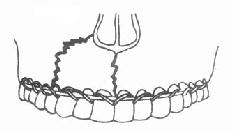
2. Traction reduction: If a jaw fracture has been present for an extended period (over three weeks for the maxilla and over four weeks for the mandible), and fibrous tissue has partially healed at the fracture site, making manual reduction unsuccessful, traction reduction can be employed. For mandibular fractures, intermaxillary traction is often used. This involves placing sectional arch bars on the displaced fracture segments of the mandible (Figure 1), followed by elastic traction using small rubber bands between the arch bars of the upper and lower jaws to gradually restore the normal occlusal relationship. For maxillary fractures where the fractured segment is displaced backward, an arch bar can be placed on the maxillary dental arch, and a gypsum cap with a metal frame is constructed on the head. Elastic traction is then applied between the arch bar and the metal frame to reposition the maxillary fracture segment forward (Figure 2). For cases requiring greater traction force, horizontal gravitational traction may also be used.
|
|
Figure 1 Sectional arch bar | Figure 2 Metal-framed gypsum cap for forward traction reduction of the maxillary fracture segment |
3. Open reduction: The indications for open reduction are broader. If the fractured segments have been displaced for a long time and have developed fibrous or bony malunion, making manual or traction reduction ineffective, surgical open reduction should be performed. The fibrous tissue or callus formed between the malunited fracture ends is excised or chiseled away, and the segments are re-separated to restore the jaw to its normal position. Open reduction is generally used for fresh fractures that are difficult to reduce manually or remain unstable after reduction, as well as for open fractures.
Fixation after jaw fracture reduction is a critical step in treatment. Common fixation methods include single-jaw arch splinting, intermaxillary fixation, intermaxillary wiring fixation, miniplate or microplate fixation, craniomaxillofacial fixation, and other methods such as circumferential jaw fixation and compression plate fixation.
1. Single-jaw arch splinting: A 2-mm diameter aluminum wire or prefabricated arch bar with hooks is shaped to match the dental arch. Thin ligature wires are then passed through the interdental spaces to secure the arch bar to some or all teeth on either side of the fracture line (Figure 3), stabilizing the fractured segments. This method is suitable for fractures with minimal displacement, such as linear fractures of the mandibular symphysis or localized alveolar process fractures.
2. Intermaxillary fixation: The commonly used method involves placing arch bars with hooks on the upper and lower teeth, followed by intermaxillary fixation using small rubber bands to maintain the jaw in the correct occlusal position (Figure 4). This method is stable and reliable, suitable for various mandibular fractures. Its advantage is that it allows the jaw to heal in an optimal position, facilitating functional recovery. However, the disadvantage is that the patient cannot open the mouth to eat, and maintaining oral hygiene becomes difficult, necessitating enhanced care.
|
|
Figure 3 Single-jaw dental arch splintage | Figure 4 Intermaxillary traction fixation method |
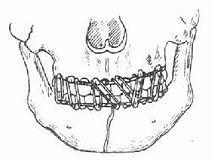
3. Interosseous wiring fixation: For cases requiring open reduction, holes can be drilled at both ends of the fracture, and stainless steel wires can be passed through for ligation and fixation (Figure 5). This is also a reliable fixation method. Pediatric jaw fractures and edentulous jaw fractures can also be fixed using this method.
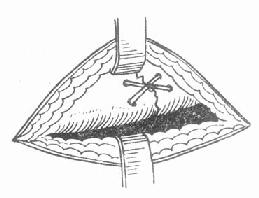
Figure 5 Interosseous wiring fixation method
4. Mini-plate or microplate fixation: Based on open reduction, appropriately sized and shaped mini-plates or microplates are placed across the bone surfaces at both ends of the fracture. Special screws are used to penetrate the cortical bone to secure the plates, achieving the goal of fracture fixation (Figure 6). Mini-plates are generally used for the mandible, while microplates are suitable for the maxilla.
5. Craniomaxillary fixation method: For transverse fractures of the maxilla, fixation cannot rely solely on the mandible. The skull can be utilized for fixation to prevent elongation and deformation of the midface. The fixation method involves first placing a dental arch splint on the maxillary teeth. One end of a stainless steel wire is ligated to the posterior dental arch splint, and the other end is passed through the oral cavity and the zygomatic soft tissues, then suspended on the frame of a plaster cap (Figure 7). Intermaxillary fixation is also applied simultaneously.
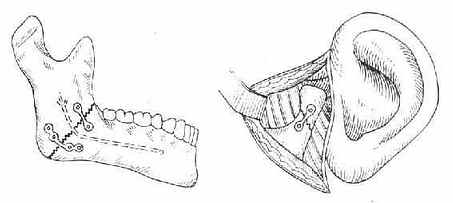
Figure 6 Mini-plate or microplate fixation method
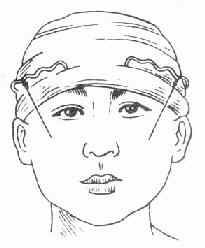
Figure 7 Craniomaxillary fixation method
The duration of jaw fracture fixation can be determined based on the patient's injury, age, and overall condition. Generally, it is 3–4 weeks for the maxilla and 4–8 weeks for the mandible. A combination of dynamic and static methods can be used to shorten the intermaxillary fixation time. The method involves removing the rubber bands during meals after 2–3 weeks of fixation to allow appropriate movement. After rigid internal fixation with mini-plates or microplates, functional training can be initiated earlier to promote fracture healing.