| disease | Acute Renal Failure in Children |
| alias | Acute Renal Failure, Acute Kidney Failure |
Acute renal failure, abbreviated as acute kidney failure, is a syndrome of a specific nature caused by various factors leading to a sharp decline or even loss of kidney function. This means the kidneys cannot regulate urine output and composition according to the body's needs. Its characteristics include disruption of the stability of water and electrolytes in the internal environment, acid-base imbalance, and retention of metabolic waste products. Although oliguria (daily urine output less than 400mg/m2) is common, some cases, such as acute renal failure caused by aminoglycoside nephrotoxicity or antibiotics like gentamicin and kanamycin, may exhibit near-normal urine output. Therefore, monitoring renal function through blood tests (e.g., urea nitrogen) and urine output measurements is crucial.
bubble_chart Etiology
Acute kidney failure can be caused by many factors. Based on the relationship between the disease cause and the kidneys, it can be classified into prerenal, renal, and postrenal.
1. Prerenal Prerenal kidney failure is due to a rapid decrease in effective systemic blood circulation volume and a reduction in cardiac output, leading to decreased renal cortical blood flow and glomerular filtration rate. If low perfusion is restored within a certain period, kidney function can return to normal; however, if it persists beyond a certain time, kidney parenchymal damage occurs.
⑴ Reduced blood volume: Blood loss, gastrointestinal loss, decreased plasma protein, burns, or kidney/adrenal diseases accompanied by salt loss.
⑵ Hypotension: Sepsis, disseminated intravascular coagulation, hypothermia, hemorrhage, heart failure.
⑶ Hypoxia: Pneumonia, constriction of the main artery, respiratory distress syndrome.2. Renal Acute kidney failure caused by kidney diseases includes acute kidney failure due to rapidly progressive glomerulonephritis, such as secondary to streptococcal infection, lupus erythematosus, membranoproliferative nephritis, idiopathic rapidly progressive nephritis, or allergic purpura.
Activation of the intrarenal coagulation system leading to small vessel thrombosis can cause acute kidney failure, such as renal vein thrombosis, cortical necrosis, and hemolytic uremic syndrome. Hemolytic uremic syndrome is the most common cause of acute kidney failure in infants.
The term "acute tubular necrosis" originally described necrosis of the renal tubules, primarily the proximal tubular epithelial cells, in the absence of arterial constriction or glomerular lesions. The mechanisms include changes in intrarenal hemodynamics, tubular obstruction, and passive reflux of glomerular filtrate through injured tubules into periglomerular capillaries. It results from direct toxic effects on the kidneys, caused by factors such as heavy metals (e.g., mercury, arsenic), chemicals (e.g., carbon tetrachloride), drugs (e.g., sulfonamides, rifampin), antibiotics (e.g., kanamycin, neomycin, gentamicin, polymyxin), hemoglobin, myoglobin, shock, and ischemia.
Acute kidney failure caused by acute interstitial nephritis due to infections or drugs is often an allergic reaction to treatment.
Tumor infiltration of the kidneys or uric acid crystal obstruction of the tubules can also lead to renal failure. Developmental abnormalities such as polycystic kidney disease, hypoplasia, or hereditary nephritis may complicate acute kidney failure. Children with these disorders often cannot conserve sodium and water, but sodium and water loss may be compensated by increased oral intake. If accompanied by vomiting, diarrhea, or urinary salt and water loss, intravascular volume depletion and renal failure may occur.
3. Postrenal Any cause of urinary tract obstruction can lead to secondary renal failure. These patients often have concurrent urinary tract infections. For ureteral obstruction to cause renal failure, it must be bilateral.bubble_chart Clinical Manifestations
Symptoms and signs may be prominent or altered by underlying diseases. Clinical findings related to renal failure include pallor (anemia), decreased urine output, edema (sodium and water retention), hypertension, vomiting, and drowsiness (uremic encephalopathy). Complications of acute kidney failure include volume overload leading to congestive heart failure and pulmonary edema, arrhythmias, gastrointestinal bleeding due to gastritis or stress ulcers, seizures, unconsciousness, and behavioral changes.
A detailed medical history can help identify the cause of renal failure. Vomiting, diarrhea, and fever suggest dehydration and prerenal azotemia. However, these symptoms can also precede hemolytic uremic syndrome and renal vein thrombosis. If skin lesions or throat infections occur first, they may indicate post-streptococcal glomerulonephritis. Rashes can be seen in systemic lupus erythematosus or allergic purpura. Attention should be paid to exposure to or use of chemical agents and medications. A flank mass may indicate renal vein thrombosis, tumor, polycystic kidney disease, or urinary tract obstruction.
Laboratory tests may reveal anemia (rarely due to blood loss; anemia may result from hemodilution or hemolysis, as seen in lupus, renal vein thrombosis, and hemolytic uremic syndrome); leukopenia (lupus nephritis); thrombocytopenia (lupus, renal vein thrombosis, hemolytic uremic syndrome); hyponatremia; hyperkalemia; acidosis; elevated serum urea nitrogen, creatinine, uric acid, and phosphorus (indicating decreased renal function); and hypocalcemia (due to hyperphosphatemia). Serum C3
levels may be decreased (in post-streptococcal infection, lupus, or membranoproliferative glomerulonephritis), or antibodies against streptococci may be detected in the serum (post-streptococcal glomerulonephritis). Chest radiography may reveal cardiomegaly and pulmonary congestion due to fluid overload. In children with acute kidney failure, urinary tract obstruction should be considered, and investigations such as abdominal plain films, ultrasonography, renal scintigraphy, or, if necessary, retrograde pyelography should be performed. If obstruction is identified, urgent percutaneous nephrostomy may be required. Finally, a renal biopsy may be necessary to determine the cause of renal failure.bubble_chart Treatment Measures
In addition to treating the disease cause, the primary treatment is to help the child survive the renal failure period, minimize the internal environmental disturbances caused by oliguria, and promote the recovery of renal lesions.
1. Maintaining water and electrolyte balance: During the physical examination, the child's fluid status must be assessed. Sometimes, it is difficult to distinguish between oliguria caused by hypovolemia and acute tubular necrosis. In cases of hypovolemia, the urine is concentrated (urine osmolality >500 mmol/L, urine sodium usually <20 mmol/L), and the fractional excretion of sodium (FENa) is often less than 1%. 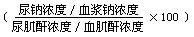 In contrast, with tubular necrosis, the urine is dilute (urine osmolality <350 mmol/L, urine sodium usually >40 mmol/L), and FENa is often greater than 1%.
In contrast, with tubular necrosis, the urine is dilute (urine osmolality <350 mmol/L, urine sodium usually >40 mmol/L), and FENa is often greater than 1%.
If hypovolemia is present without blood loss or hypoalbuminemia, colloidal expansion is unnecessary. Instead, isotonic saline (20 mL/kg) can be administered intravenously over 30 minutes, and the patient usually urinates within 2 hours. If the child still does not urinate, a urinary catheter should be inserted to measure bladder urine volume and central venous pressure. If clinical and laboratory tests confirm adequate fluid replacement, diuretics should be considered. Although diuretics are ineffective for children who have already developed anuria, do not alter renal function, and do not affect the natural course of renal failure, drugs like furosemide or mannitol act on changes in tubular function, accelerating urine flow. For some oliguric patients, promoting urine output is valuable for managing hyperkalemia and water retention. A single intravenous dose of furosemide (2 mg/kg) can be administered at a rate of 4 mg/min. If there is no response, a second dose (10 mg/kg) may be given. If urine output does not increase, furosemide should be discontinued, and a single dose of mannitol (0.5 g/kg) can be administered intravenously. Regardless of the response, mannitol should not be repeated to avoid toxic reactions. If the patient does not have hypertension, dopamine (5 μg/kg/min) can be combined with diuretics to increase renal cortical blood flow.
If adequate urine output is not achieved after fluid replacement or diuretic administration, fluid intake must be strictly restricted. The restriction should be based on the patient's fluid status. For patients with oliguria or anuria but normal blood volume, fluid intake should be limited to insensible water loss [400 mL/(m2·24h) or 1 mL/(kg·h)] plus the urine output for that day. If water retention is present, fluid intake should be completely restricted to reduce the already expanded blood volume. Generally, electrolyte-free 10–30% glucose solution is administered at the slowest possible rate via an infusion pump to maintain intravascular volume. The infusion content can also be adjusted based on electrolyte balance. Except in cases of excessive water retention, extrarenal fluid losses such as blood loss or abnormal gastrointestinal losses (vomiting, diarrhea) should be replenished.
2. Management of Hyperkalemia Acute kidney failure can rapidly lead to hyperkalemia (serum potassium >6 mmol/L), which may cause arrhythmia and death. The earliest electrocardiogram (ECG) changes in patients with hyperkalemia include peaked T waves, followed by ST-segment depression, prolonged P-R interval, widened QRS complex, ventricular fibrillation, and cardiac arrest. When serum potassium rises to 5.5 mmol/L, the patient's fluids should contain a high concentration of glucose, and potassium-lowering resin (1 g/kg) should be administered orally or via retention enema. Potassium-lowering resin is a medicinal sodium-based cation exchange resin. When taken orally or administered as an enema, it undergoes ion exchange in the intestines, absorbing potassium and excreting it through feces, thereby reducing serum potassium levels. The advantage of sodium-based resin is that it does not exacerbate toxicity and can also absorb ammonium ions in the intestines of uremic patients, reducing urea synthesis. The best method is to suspend the potassium-lowering resin in 2 mL/kg of 70% sorbitol for oral administration. Sorbitol induces osmotic diarrhea, promoting the loss of water and electrolytes (renal failure patients often have fluid retention and elevated sodium and potassium levels), thereby facilitating the excretion of water and electrolytes through the gastrointestinal tract. If 70% sorbitol is used for enemas, it may irritate the rectal mucosa, so a 20% concentration is preferable, and the dose can be increased to 10 mg/kg. Resin therapy can be repeated every 2 hours, but the frequency should be carefully monitored to avoid the risk of sodium overload.
If serum potassium rises above 7 mmol/L, in addition to the use of potassium-lowering resins, the following treatments should be applied.
⑴ Intravenous injection of 10% calcium gluconate at 0.5 mg/kg, administered slowly, with close monitoring of heart rate. If the heart rate drops by 20 beats per minute, the infusion should be stopped until the heart rate returns to its pre-infusion rate.
⑵ Intravenous injection of 5% sodium bicarbonate at 3 mmol/kg, avoiding volume expansion, hypertension, and spasms.
⑶ Administer a mixture of 50% glucose at 1 mg/kg and insulin (1 unit of insulin requires 5 g of glucose) intravenously over at least 1 hour, with close monitoring to prevent hypoglycemia.
Calcium gluconate does not lower serum potassium levels but can counteract myocardial irritability caused by potassium. The mechanism by which sodium bicarbonate lowers blood potassium is unclear. The intravenous mixture of glucose and insulin facilitates the transfer of extracellular potassium into cells. Beta-adrenergic agonist nebulization can also rapidly reduce blood potassium levels. These emergency measures only take a few hours. If hyperkalemia persists, dialysis therapy is required.
3. Correcting acidosis—In renal failure, due to insufficient excretion of hydrogen and ammonium ions, grade II acidosis is common but rarely requires treatment. Severe acidosis (stirred pulse pH < 7.15, serum bicarbonate < 8 mmol/L) can increase myocardial irritability and thus requires intervention. Due to the risks of rapid alkaline infusion, only partial correction of acidosis is needed intravenously, with bicarbonate administered to raise the stirred pulse pH to 7.2 (approximately equivalent to serum bicarbonate of 12 mmol/L). The correction formula is as follows:
NaHCO2 required (mmol) = 0.3 × body weight (kg) × [12 - serum bicarbonate (mmol/L)].
Once serum calcium and phosphorus reach normal levels, further correction of acidosis can be achieved orally with sodium bicarbonate or sodium citrate solution.
In renal failure, impaired phosphorus excretion leads to hyperphosphatemia and corresponding hypocalcemia. However, due to concurrent acidosis, free calcium levels often remain normal, preventing spasms. Rapid correction of acidosis may lower free calcium levels and trigger spasms.
4. Hypocalcemia—Methods to lower serum phosphorus can be used. Except for children with hand-foot convulsions, intravenous calcium supplementation is unnecessary. Generally, oral calcium carbonate antacids that bind phosphates can be used to increase fecal phosphate excretion.
5. Hyponatremia—Hyponatremia is often corrected for oliguria or anuria. If serum sodium falls below 120 mmol/L, the risk of cerebral edema and central nervous system hemorrhage increases. If the patient is not dehydrated, fluid intake should be restricted. If serum sodium drops below 120 mmol/L, hypertonic (3%) sodium chloride should be administered intravenously to raise serum sodium to 125 mmol/L. The required NaCl (mmol) can be calculated as: 0.6 × body weight (kg) × [125 - serum sodium (mmol/L)]. Risks of hypertonic saline include fluid expansion, hypertension, and congestive heart failure. If these occur, dialysis therapy should be considered.
6. Gastrointestinal bleeding—Calcium carbonate antacids can be used for prevention and to lower serum phosphorus. Intravenous cimetidine at 5–10 mg/(kg·12h) may also be administered.
7. Hypertension can be caused by primary disease or extracellular fluid expansion, or both. For patients with renal failure and hypertension, restricting salt and water intake is crucial. In children with severe hypertension, diazoxide can be administered intravenously at 5mg/kg (maximum single dose of 300mg) over 10 seconds Neijing. Blood pressure often decreases within 10 to 20 minutes. If the response is unsatisfactory, the dose can be repeated once after 30 minutes. Alternatively, nifedipine (0.25–0.5mg/kg, sublingual) can be used rapidly for heart pain. For hypertensive crisis, continuous intravenous infusion of sodium nitroprusside or labetalol is recommended. For less severe hypertension, controlling extracellular fluid volume expansion (by restricting salt and water intake and using furosemide) along with β-blockers like propranolol and vasodilators is often effective.
8. Others Spasms may be related to the primary disease, such as systemic lupus erythematosus, hyponatremia (water intoxication), hypocalcemia, hypertension, or uremia itself. Treatment should target the underlying condition. Generally, anticonvulsant drugs like chloral hydrate, phenobarbital, and phenytoin sodium are less effective in uremic patients. Diazepam is effective in controlling spasms.
Unless there is hemolysis (e.g., hemolytic uremic syndrome, lupus) or bleeding, anemia in acute kidney failure is usually mild (hemoglobin 90–100 g/L) due to fluid expansion and does not require transfusion. If there is acute bleeding, hemolytic anemia, or persistent renal failure, and hemoglobin drops to 70 g/L, transfusion is necessary. In patients with fluid overload, transfusion can lead to fluid expansion, causing hypertension, congestive heart failure, and pulmonary edema. Slow transfusion (4–6 hours) of fresh blood (to reduce potassium intake) at 10 ml/kg can minimize fluid expansion. If severe fluid retention is present, anemia should be corrected during dialysis.
In most previously healthy or well-nourished children who suddenly develop acute kidney failure, the initial diet should consist only of fats and carbohydrates, with restrictions on sodium, potassium, and fluid intake. If renal failure persists for about 7 days, oral or parenteral supplementation of essential amino acids should be considered.
Indications for dialysis in acute kidney failure include a combination of the following factors: acidosis, electrolyte imbalances (especially hyperkalemia), central nervous system disturbances, hypertension, fluid retention, and congestive heart failure. Early initiation of dialysis in children with acute kidney failure can significantly improve survival rates.
Some patients with acute kidney failure may reduce complications and delay dialysis with careful conservative treatment, while others still require dialysis. Fatal complications of uremia include bleeding, pericarditis, and central nervous system dysfunction.
The prognosis for renal function recovery is related to the primary cause of acute kidney failure. For instance, in prerenal factors such as hemolytic uremic syndrome, acute tubular necrosis, acute interstitial nephritis, or uric acid nephropathy, renal function is generally easier to recover. However, in most cases of rapidly progressive glomerulonephritis, bilateral renal vein thrombosis, or bilateral renal cortical necrosis, renal function is less likely to recover.




