| disease | Poisonous Snake Bite |
There are approximately 2,500 species of snakes worldwide, with over 650 of them being venomous, posing a threat to vast regions inhabited by about a billion people. It is estimated that more than 300,000 people are bitten by poisonous snakes each year, with a mortality rate of around 10%. In the Guangdong and Guangxi regions of China, snake-related incidents are severe, with an annual incidence rate of snakebites at about 25 per 10,000 people. China is home to over 160 snake species, about 50 of which are venomous, including 10 highly toxic and dangerous ones such as the king cobra, banded krait, cobra, hundred-pace viper, banded krait, viper, pit viper, bamboo leaf viper, sharp-nosed viper, and sea snake, whose bites can be fatal. These venomous snakes are commonly found in southern forests, mountainous areas, and grasslands during summer and autumn. People are at risk of being bitten by poisonous snakes while cutting grass, gathering firewood, picking wild fruits, harvesting vegetables, walking, or during military training. Venomous snakes typically have triangular heads, slender necks, short and thick tails, and brightly colored patterns. When biting, they open their mouths wide, revealing long fangs. Poisonous snake bites often leave two rows of deep and thick tooth marks. If it is uncertain whether the bite is from a venomous snake, treat it as a poisonous snake bite and administer first aid accordingly.
bubble_chart Pathogenesis
(1) Classification of Venomous Snakes: Venomous snakes can be roughly divided into three major categories
1. Neurotoxic snakes: Including the Banded Krait (金環蛇) and sea snakes, their venom primarily affects the nervous system, causing muscle paralysis and respiratory paralysis.
2. Hemotoxic snakes: Such as the Bamboo Leaf (竹葉青), viper (蝰蛇), and turtle-shelled snake (龜殼花蛇), their venom mainly impacts the blood and circulatory system, leading to hemolysis, hemorrhage, coagulation disorders, and heart failure.3. Snakes with both neurotoxic and hemotoxic venom: Such as the pit viper (蝮蛇), king cobra (大眼鏡蛇), and cobra (眼鏡蛇), their venom exhibits characteristics of both neurotoxins and hemotoxins.
(2) Active Components of Snake Venom:
1. Neurotoxins: Primarily act on the nervous system.
2. Cardiotoxins: Mainly affect the heart, causing heart failure.
3. Cytotoxins: Can destroy blood cells and cause necrosis of vascular endothelial cells.
4. Coagulants: Can lead to thrombus formation.
5. Various enzymes: Can cause hemolysis and tissue damage.
(3) Toxicity Levels of Snake Venom: The toxicity of venom varies among different species of venomous snakes. Some snakes have a high mortality rate after envenomation, while others only cause symptoms. The table below compares the single venom yield and lethal dry venom dose of several venomous snakes. (Table 1-21)
Table 1-21 Comparison of Venom Yield and Lethal Dose (mg)
Snake Name | Single Dry Venom Yield | Lethal Dry Venom Dose |
Banded Krait (銀環蛇) | 5.4 | 1.0 |
Sea Snake (海蛇) | 6.0 | 3.5 |
Bamboo Leaf (竹葉青) | 14.1 | 100.0 |
Golden Krait (金環蛇) | 43.0 | 10.0 |
Pit Viper (蝮蛇) | 45.0 | 25.0 |
Viper (蝰蛇) | 72.0 | 42.0 |
King Cobra (大眼鏡蛇) | 100.0 | 12.0 |
Cobra (眼鏡蛇) | 211.0 | 15.0 |
bubble_chart Clinical Manifestations
After being bitten by a poisonous snake, the speed and severity of symptoms in the patient are significantly related to the type of snake, the dose and nature of the venom. Of course, the location of the bite, the depth of the wound, and the patient's resistance also have some influence. When a poisonous snake actively attacks a person in a hungry state, the amount of venom discharged is large, and the consequences are severe.
(1) Manifestations of neurotoxic injury: The wound area becomes numb, loses sensation, or only has mild itching. The wound shows little redness or swelling, with minimal bleeding. About half an hour after the injury, the patient may experience dizziness, drowsiness, nausea, vomiting, and lack of strength. In severe cases, difficulty swallowing, hoarseness, aphasia, eyelid drooping, and double vision may occur. Eventually, respiratory distress, decreased blood pressure, and shock may lead to hypoxia, cyanosis, and systemic paralysis. If rescue is deficient, respiratory and circulatory failure may ultimately occur, leading to rapid death. Neurotoxins are absorbed quickly, posing high risks, and because local symptoms are mild, they are often overlooked. The first to second days after the injury are the critical period. Once this period is passed, symptoms can improve rapidly, and no sequelae remain after recovery.(2) Manifestations of hematotoxic injury: The bite site swells rapidly and continuously spreads proximally. The wound causes severe pain and continuous bleeding. The surrounding skin often develops blisters or blood blisters, subcutaneous bruising, and tissue necrosis. In severe cases, widespread systemic bleeding may occur, such as subconjunctival static blood, epistaxis, hematemesis, expectoration of blood, and hematuria. Some patients may also experience thoracic or abdominal bleeding and intracranial hemorrhage, ultimately leading to hemorrhagic shock. Patients may also experience dizziness, nausea, vomiting, and diarrhea, joint pain, and high fever. Since symptoms appear earlier, treatment is generally more timely, resulting in a lower mortality rate compared to neurotoxic injuries. However, due to the acute onset and prolonged course, the critical period is longer, and delayed treatment can lead to severe consequences. Local and visceral sequelae often remain after recovery.
(3) Manifestations of mixed toxic injury: Symptoms include both neurotoxic and hematotoxic effects. Locally, the wound resembles hematotoxic injury, with redness, swelling, bruising, blood blisters, tissue necrosis, and lymphadenitis. Systemically, it resembles neurotoxic injury. The primary cause of death in such cases remains neurotoxicity.When diagnosing a snakebite, the following issues must be considered and addressed:
(1) Whether it is a snakebite: First, the possibility of a snakebite must be clearly excluded. Other animals can also cause injuries, such as centipede bites or wasp stings. However, the latter injuries do not exhibit the typical fang marks of a snakebite and have their own distinct characteristics. For example, a centipede bite leaves two horizontally aligned dot-like marks, while a wasp or scorpion sting results in a single scattered wound. Generally, injuries caused by centipedes, etc., are minor and do not present significant systemic symptoms.
(2) Whether it is a poisonous snake bite: This is primarily distinguished by unique fang marks, local wound conditions, and systemic manifestations. A poisonous snake bite often leaves one pair or three to four fang marks, with significant swelling, pain, or numbness around the wound, as well as bruising, blisters, or blood blisters. Systemic symptoms are also more pronounced. In contrast, a non-poisonous snake bite leaves two rows of serrated fang marks. (Figure 1)

Figure 1: Typical fang marks of poisonous and non-poisonous snakes
(3) Which type of poisonous snake bite: Accurately identifying the specific poisonous snake responsible is challenging. Based on the characteristics of the local wound, neurotoxic snakebites can be preliminarily distinguished from hemotoxic snakebites. Further identification of the snake species can be made by considering unique clinical manifestations, fang spacing, and fang mark morphology. (Table 1) For example, cobra bites often cause pupil constriction, viper bites may lead to hematuria within half an hour, and pit viper bites can result in double vision.
Table 1: Fang spacing and fang mark morphology of several major poisonous snakes
Snake Name | Fang Spacing (cm) | Fang Mark Morphology |
Bamboo Leaf Green | 0.5–1.2 | ("八"-shaped) |
Pit Viper | 0.6–1.2 | ( ) Small fang spacing |
Golden Krait | 0.8–1.6 | ( ) "品"-shaped. The skin around the wound often resembles lychee peel. |
Banded Krait | 0.8–1.4 | ( ) "品"-shaped, with frequent skin tearing around the wound. |
Viper | 1.0–1.5 | ( ) The tissue around the wound appears darkened. |
Cobra | 1.1–1.9 | ( ) Significant bruising and swelling around the wound. |
King Cobra | 1.5–3.0 | ( ) Pronounced swelling around the wound. |
Five-step snake | 1.5~3.5 | ( ) The tooth spacing is large, bleeding is profuse, and local blisters and blood blisters are common. |
The head of a venomous snake is slightly triangular, with brightly colored patterns on its body, and paired fangs on the upper jaw, which can distinguish it from non-venomous snakes. The fangs are grooved or tubular and connected to the venom gland. When the muscles surrounding the gland contract, the venom is discharged through the duct into the fangs and injected into the bitten person or animal. (Figure 2)
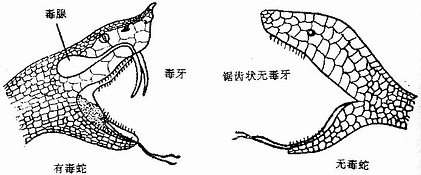
Figure 2 Differences between venomous and non-venomous snakes
bubble_chart Treatment Measures
First aid on the scene after a poisonous snake bite is crucial. Various measures should be taken to quickly remove the venom and prevent its absorption and spread. Upon reaching a well-equipped medical station, comprehensive measures should continue, such as thorough debridement, oral and topical application of effective snakebite medicine, administration of antivenom serum, and systemic supportive therapy.
(1) Preventing Venom Absorption: After a bite, snake venom rapidly enters the body within 3–5 minutes. Effective measures should be taken as early as possible to prevent venom absorption.
1. **Tourniquet Method**: This is a simple and effective method, easily performed for self-rescue or mutual aid on the scene. Immediately after a poisonous snake bite, use a cloth strip, towel, or bandage to bind the limb 5–10 cm proximal to the bite or at the base of the bitten finger (toe) to reduce venous and lymphatic flow, thereby temporarily preventing venom absorption. During transport, loosen the tourniquet every 20 minutes for 1–2 minutes each time to prevent limb static blood and tissue necrosis. The bandage should only be removed after thorough wound debridement and 3–4 hours of taking snakebite medicine.
2. **Ice Pack Method**: If possible, apply ice packs to the bitten limb while it is bound to constrict blood and lymphatic vessels, slowing venom absorption. Alternatively, immerse the limb or finger in cold water (4–7°C) for 3–4 hours, then switch to ice packs for 24–36 hours. However, while cooling the local area, ensure the patient remains warm overall.
3. **Immobilization of the Bitten Limb**: After injury, move slowly and avoid running to reduce toxin absorption. Ideally, immobilize the limb temporarily and keep it in a low position while transporting to a medical station. If necessary, administer a mild sedative to keep the patient calm.
(2) Promoting Venom Elimination and Neutralization: Measures should be taken to expel or neutralize any remaining venom at the wound site. The simplest method is oral suction, rinsing the mouth with clean water after each suction. However, the suctioner’s oral mucosa and lips must be free of breaks. Alternatively, use breast pumps or cupping devices to extract venom, which is also effective.
For deep or contaminated wounds, perform thorough debridement. After disinfection, make a "+" or "++" shaped incision centered on the fang marks to allow residual venom to drain. Avoid cutting too deep to prevent vascular injury. For bites on hands or feet, use a triangular needle or knife tip to puncture the Baxie (Eight Evils) or Bafeng (Eight Winds) acupoints subcutaneously (1 cm deep), then gently massage from proximal to distal to accelerate venom expulsion. After enlarging the wound, apply topical medications for wet compresses or irrigation to neutralize the venom. Common topical agents include 30% saline or alum solution, while irrigation solutions include 1:5000 potassium permanganate or 5–10% saline.
Local injection of trypsin can help decompose and neutralize venom, alleviating or inhibiting poisoning symptoms. Dissolve trypsin in 2–4 mL of saline and inject it into the wound base and surrounding area, repeating after 12–24 hours if needed. Administering diuretics like furosemide, ethacrynate sodium, or mannitol can accelerate venom excretion through the urinary system.
(3) **Inhibiting Venom Effects**: Primarily involves oral and topical application of effective Chinese herbal medicine and snakebite tablets to achieve detoxification, anti-inflammatory, hemostatic, cardiotonic, and diuretic effects. Antivenom serum is widely used clinically and is particularly effective against the same species of poisonous snake bite.
1. Various Snake Antivenom Tablets: Currently, there are more than ten types of snake antivenom tablets used in clinical practice. When using them, it is essential to first clarify which type of venomous snake the tablet is effective against. Secondly, the medication should be administered early, in large doses, and over a long course of treatment. Finally, targeted auxiliary treatments combining traditional Chinese and Western medicine must be applied. The most widely used clinically is the Nantong Snake Antivenom Tablet (also known as Jidesheng Snake Antivenom Tablet). Immediately after the injury, 20 tablets should be taken, followed by 10 tablets every 6 hours until the symptoms of poisoning are significantly alleviated. At the same time, the tablets should be mixed with warm water to form a paste and applied around the wound and 3–4 cm above the swollen area of the limb. The Guangzhou Snake Antivenom Tablet (He Xiaosheng Snake Antivenom Tablet) is also quite effective. Immediately after the injury, 5 tablets should be taken, followed by 5 tablets every 3 hours. For severe cases, the dosage should be doubled. Additionally, the Shanghai Snake Antivenom Tablet is mainly used for bites from Agkistrodon halys (Pallas), while the Sanman Snake Antivenom Tablet is primarily effective against bites from Bungarus fasciatus (Banded Krait).
2. Chinese herbal medicine Single prescription: Fresh Chinese Lobelia Herb (whole plant) 30-60 grams can be crushed to extract its juice for oral administration, which has the effects of removing toxin and diuresis for detoxification. Alternatively, 30 grams of fresh Sapium sebiferum tender buds can be crushed to extract the juice for oral administration, with the residue applied externally to prevent snake venom from attacking the heart.
3. Serum therapy: Antivenom has certain efficacy against poisonous snake bite, with monovalent serum efficacy reaching up to 90%, while polyvalent serum efficacy is only 50%. Currently, successfully tested antivenoms include anti-Agkistrodon halys serum, anti-Naja serum, anti-Deinagkistrodon serum, and anti-Banded Krait serum, some of which have been refined into powder form for easier storage. Before administering antivenom, a skin allergy test should be conducted, and injection can proceed if the result is negative.
4. Systemic supportive therapy: In the days following a poisonous snake bite, the condition is severe, with pronounced toxic symptoms often accompanied by varying degrees of water-electrolyte imbalance and shock. Severe cases may lead to respiratory failure, heart failure, acute renal failure, and hemolytic anemia. Therefore, active systemic treatment and correction of major organ functions are crucial. If blood pressure is low, timely blood transfusion and fluid replacement should be administered for anti-shock treatment. If breathing is weak, respiratory stimulants and oxygen inhalation should be provided, with assisted respiration if necessary. The use of adrenal corticosteroids and antihistamines can help neutralize toxins and alleviate toxic symptoms. Systemic anti-infective drugs are important for preventing and treating local tissue necrosis, and routine TAT injections should be administered to prevent tetanus.
Snakebites pose a serious threat to the health of laborers. In high-risk areas, proactive preventive measures should be taken to minimize the incidence of snakebites and reduce mortality rates. First, a comprehensive snakebite prevention and treatment network must be established, ensuring organizational and manpower support with clear responsibilities and dedicated personnel. Second, efforts should be made to mobilize the public to improve environmental hygiene around residences by thoroughly removing weeds, clearing scattered rocks, sealing burrows, and eliminating potential hiding spots for venomous snakes. Regular snake extermination and capture activities should also be conducted. Additionally, basic knowledge on preventing snakebites should be widely disseminated. For those working in the wild, before entering grassy areas, they should use sticks to drive away venomous snakes. When working or patrolling in dense forests, they must remain vigilant, promptly addressing potential hazards, and wear long-sleeved shirts, long pants, shoes, socks, and, if necessary, straw hats. If encountering a venomous snake, avoid panic—instead, evade by moving in zigzag patterns or stand still, facing the snake, and dodging its strikes while looking for an opportunity to pick up a branch for self-defense. Applying snake repellent to limbs or taking oral snakebite detoxification tablets can also help prevent snakebites.




