| disease | Hydrocele |
Hydrocele refers to the accumulation of excessive fluid between the two layers of the tunica vaginalis of the testis. Most hydroceles have no obvious disease cause and are referred to as primary hydroceles. Their onset and progression are relatively slow, and patients may be asymptomatic. Hydroceles caused by scrotal trauma, inflammation or tumors of the testis and epididymis, as well as filariasis, are called secondary hydroceles. They often present with symptoms of the primary condition.
bubble_chart Pathogen
The testis descends from the abdominal membrane to be decocted later into the scrotum, and the abdominal membrane follows it downward, becoming the tunica vaginalis of the testis. The layer of the tunica vaginalis surrounding the testis and epididymis is the visceral layer, while there is another outer layer called the parietal layer. There is only a small amount of fluid between these two layers. The processus vaginalis, which descends with the testis, completely closes after birth and becomes a cord-like structure. If the processus vaginalis fails to close entirely, fluid from the abdominal cavity (ascites) can flow through its unclosed lumen to the area around the testis or remain at a certain segment of the spermatic cord, forming a hydrocele known as congenital or communicating hydrocele. If excessive fluid accumulates between the two layers of the tunica vaginalis propria of the testis, it results in testicular hydrocele (Figure 1).
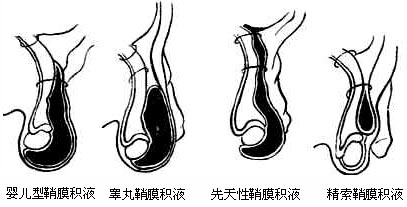
Figure 1 Classification of hydrocele
bubble_chart Clinical Manifestations
Primary hydrocele is initially asymptomatic and develops slowly. The patient only becomes aware of it when it grows to a certain size. An excessively large testicular hydrocele causes a dragging sensation due to its weight. Sometimes, it may bury the penis within the skin and affect urination. Congenital hydrocele is characterized by the rapid disappearance of the mass when lying flat. However, if the communicating channel is very narrow, the mass may only slightly shrink or soften after prolonged bed rest, making it easy to misdiagnose as testicular hydrocele. When taking the medical history, it is crucial to inquire in detail about changes in the size of the mass. A spermatic cord hydrocele often appears as a mass above the testicle, similar in size to the testis, and is sometimes mistaken for a third testicle. Testicular hydrocele is typically pear-shaped, with the testis buried within and untouchable. The hardness of the cyst varies greatly. When the fluid volume is large, it can be very firm, resembling a testicular tumor.
bubble_chart DiagnosisAll types of hydrocele test positive (transillumination) on a transillumination test. One type of testicular hydrocele, due to its prolonged duration, has an exceptionally thick parietal layer. The transillumination test may yield a negative result (no transillumination). If the diagnosis of hydrocele remains uncertain, especially when it has persisted for a long time with an unusually thick parietal layer, and the possibility of a hernia can be ruled out, a diagnostic puncture may be performed. The fluid aspirated from a hydrocele is a clear, pale yellow liquid.
bubble_chart Treatment Measures
(1) Hydrocele in newborn infants often resolves spontaneously before the age of two, so treatment is not urgently needed. If it persists beyond two years, fluid aspiration is performed. In most cases, the condition does not recur after aspiration. This method is not suitable for adults, as the fluid typically reaccumulates shortly after aspiration in adults.
(2) Injection therapy: After fluid aspiration, irritating agents such as quinine or sodium morrhuate are injected into the tunica vaginalis cavity to induce inflammatory adhesions, thereby obliterating the cavity. This method has significant side effects, often results in incomplete adhesions, and may lead to multilocular hydrocele, complicating subsequent surgical treatment. It is now less commonly used.
(3) Surgical treatment: Congenital hydrocele cannot be treated with the above methods and primarily requires surgery. The goal of surgery is to perform high ligation of the hernia neck at the internal ring to block the flow of ascitic fluid. The distal hernia sac may be left untreated.
The effective surgical method for testicular hydrocele is excision and inversion of the tunica vaginalis.
Postoperative recurrence: Hydrocele rarely recurs after surgical treatment. Analysis of recurrent cases of testicular hydrocele suggests that recurrence is mainly due to misdiagnosis of congenital hydrocele as simple testicular hydrocele, leading to tunica vaginalis inversion without high ligation. Continuous leakage of peritoneal fluid promotes epithelial regeneration and recurrence. In a minority of cases, recurrence may result from incomplete excision of multilocular testicular hydrocele.
Hydrocele should be primarily differentiated from indirect inguinal hernia and testicular tumor.
The formation and anatomical relationship of communicating hydrocele and indirect inguinal hernia are the same. The diagnosis differs only due to the varying contents of the hernia sac. If a mass rapidly protrudes along the inguinal canal when the patient stands, sometimes showing signs of intestinal loops or borborygmi, it indicates a hernia. During examination, intestinal loops may be palpated within the mass, and the spermatic cord at the external ring is thickened. In contrast, communicating hydrocele causes gradual enlargement of the scrotum without obvious protrusion in the inguinal canal, and the spermatic cord is not thickened. When performing a transillumination test, it is important to note that infants' intestinal walls are thin; even if it is a hernia, the transillumination may still appear positive. Careful examination is essential, and puncture should not be performed hastily to avoid accidental injury to the intestines. To differentiate whether it is a spermatic cord hydrocele, check if the upper part of the spermatic cord near the mass is thickened. If thickened, the mass is connected to the abdominal cavity, indicating a hernia. If not thickened, it is likely a hydrocele. In cases of testicular hydrocele, the mass occupies the entire side of the scrotum, and the testis cannot be palpated. In contrast, with a hernia, the testis can still be palpated alongside the hernia contents.





