| disease | Traumatic Nasal Septal Perforation |
Traumatic nasal septal perforation is mostly caused by trauma or sequelae of nasal septum correction surgery, and its clinical manifestations are related to the size and location, often presenting with symptoms such as minor nosebleeds or blood in nasal discharge.
bubble_chart Etiology
1. Trauma: such as shrapnel or gunshot wounds, stab wounds, cuts, etc.
2. Postoperative complications: such as accidental perforation during nasal septum correction; improper use of cryotherapy, laser, or electrocautery leading to cartilage necrosis; excessive chemical cauterization can also cause perforation.
3. Hematoma infection: Nasal impact or contusion often leads to nasal septum hematoma. If secondary infection occurs, it may form an abscess, causing extensive cartilage necrosis and perforation.
bubble_chart Clinical Manifestations
The symptoms are related to the size and location of the perforation. Larger perforations can cause dryness of the nasal mucosa, even leading to atrophy, with crusts or purulent scabs often adhering to the edges. Minor nosebleeds or blood-streaked nasal discharge are common, along with other symptoms such as nasal obstruction, reduced sense of smell, and headache. Small perforations in the anterior part of the septum usually cause milder symptoms, producing a whistling sound during breathing, which becomes more noticeable during vigorous activity. Perforations located in the posterior part of the nasal septum often present no obvious symptoms.
bubble_chart Treatment Measures
Traumatic nasal septal perforation, if it is a small to medium perforation with minimal mucosal tissue defect and the general and local conditions permit, can be immediately treated with debridement and tension-reducing sutures, or repaired by shifting adjacent mucoperiosteal flaps for suturing. If the perforation is large with significant mucosal defects, although early suturing and repair may be attempted, it often ultimately fails to heal, making delayed intervention more appropriate. Repair surgery for nasal septal perforation is challenging due to the narrow surgical field, inconvenient operation, and lack of a standardized procedure. The surgery should be flexibly and carefully designed and selected based on the size of the perforation, its anterior or posterior location, and the condition of the mucosa. It is generally accepted that combining several methods yields the best healing results for perforations. Some regions domestically have pioneered the nasal columella flip approach for mucoperiosteal inlay grafting repair of nasal septal perforation, with the steps as follows:
1. **Position and Anesthesia**: For general anesthesia, the patient is placed in a supine position; for local anesthesia, a semi-sitting position is adopted. A 1% lidocaine solution with diluted adrenaline is used for bilateral infraorbital nerve blocks and infiltration injections of the nasal columella and anterior nostril margin. Surface nasal anesthesia is achieved with 1% dyclonine cotton pads.2. **Incision**: A transverse incision is made at the root of the nasal columella down to the subcutaneous layer, extending bilaterally along the inner edge of the anterior nostril like a seagull’s wings to the outer edge of the anterior nostril, ensuring the incision is largely concealed within the anterior nostril.
3. **Nasal Columella Flip**: The subcutaneous tissue is sharply dissected within the incision, and the nasal columella is flipped upward along the anterior edge of the medial crus of the greater alar cartilage. The skin of the nasal tip and anterior nostril margin is also lifted, partially exposing the domes of the bilateral greater alar cartilages.
4. **Nasal Septum Dissection**: The nasal septal cartilage and bone are dissected between the medial crura of the bilateral greater alar cartilages. Care must be taken to minimize injury to the bilateral mucoperichondrium, and injections in the nostril area should avoid enlarging the perforation. The dissection area should be sufficiently large, extending superiorly to the junction of the septal cartilage and perpendicular plate of the ethmoid bone and inferiorly to include the nasal floor mucoperiosteum.
5. **Tension-Reducing Staggered Suture of Mucoperiosteum**: Tension-reducing incisions are made on the lateral aspects of the bilateral nasal floors and one side of the nasal roof. The perforation edges on both sides of the nostril are sutured laterally. Due to differing degrees of tension reduction, the suture lines naturally stagger and are not at the same level.
6. **Autologous Mucoperiosteal Graft Inlay**: A mucoperiosteal graft is harvested from the anteromedial surface of the tibia. Since its diameter shrinks by more than 50%, the harvested graft’s diameter should be half that of the nostril. It is then inlaid at the perforation level (Figure 1) and sutured with a single stitch to the mucoperichondrium on one side to prevent displacement.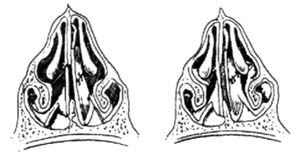
**Figure 1**: Bilateral mucoperiosteal tension-reducing staggered sutures and autologous mucoperiosteal graft inlay.
7. **Nasal Packing**: Both nasal cavities are packed with multi-layered finger-cot gauze, ensuring appropriate tightness.
8. **Incision Closure**: The nasal columella skin flap must be accurately repositioned.
9. **Postoperative Care**: The packing is removed 48 hours postoperatively. The incision sutures are removed on the 6th day, and the repair sutures are removed between the 6th and 8th days (or on the 6th day if tension is minimal).
The features of this technique for nasal septal perforation repair include: relatively spacious access, adequate tension reduction, secure suturing, reduced failure rates, and a relatively novel approach.




