| disease | Varicocele |
Varicocele refers to the dilation and tortuosity of the veins within the spermatic cord due to obstructed blood flow. It occurs in 95% of cases on the left side and is less common bilaterally.
bubble_chart Etiology
Varicose veins in the left spermatic cord have their anatomical causes, which are the internal factors of this condition, while prolonged standing and frequently sustained increases in abdominal pressure are the external factors that promote its formation and development.
In a few young individuals, higher sexual desire and more severe local congestion can also lead to varicose veins, and all cases present symptoms.
bubble_chart Pathological Changes
The veins of the testis and epididymis form a plexus within the spermatic cord, ascending through the inguinal canal and converging into several internal spermatic veins and external spermatic veins. In about 60% of individuals, the internal spermatic veins merge into a single branch at the internal ring, while a minority remain as two or three branches. They ascend through the retroperitoneal space. On the right side, they enter the inferior vena cava at an oblique angle, while on the left, they enter the left renal vein at a right angle. Due to the longer course of the left internal spermatic vein and the right-angle entry into the renal vein, the resistance is greater. The vein Maijing passes behind the sigmoid colon, where it is compressed by this segment of the intestine. Additionally, the vein lacks valves and is not supported by surrounding muscle compression, leading to impaired venous return on the left side. When standing, a significant column of blood pressure acts downward on the plexus, causing it to dilate, thicken, and become varicose, resulting in varicocele. This phenomenon can also occur when retroperitoneal tumors or renal tumors compress the veins, obstructing venous return and manifesting as varicose veins. To distinguish between the two, the latter is termed secondary varicocele, while the former is called primary varicocele. The key diagnostic criterion is that primary varicocele typically resolves quickly when lying flat, whereas secondary varicocele often persists or resolves very slowly.
bubble_chart Clinical ManifestationsPatients may be completely asymptomatic. If symptoms are present, they typically include a dragging pain in the scrotum after prolonged standing, which may radiate to the ipsilateral lower abdomen or inner thigh. These symptoms disappear when lying down. In recent years, reports have indicated that varicocele patients may experience reduced sperm count, affecting fertility. Fertility can be restored after surgical treatment. Additionally, some patients may exhibit symptoms such as restlessness, anxiety, insomnia, general weakness, and impotence. Severe varicocele can lead to testicular atrophy on the affected side, prompting patients to seek medical attention due to smaller testicles.
95% of cases occur on the left side. During examination, have the patient stand. A noticeable drooping of the affected scrotum can be observed, with sometimes tortuous veins visible on the skin surface. The veins within the scrotum are coiled into a mass resembling a bag of roundworms. Upon palpation, a soft, compressible mass of varicose veins can be felt within the spermatic cord above the testis. Occasionally, small nodules formed by thrombosis may be palpable. Similar masses can also be felt posterior and inferior to the testis. The mass quickly disappears when the patient lies down. If the mass does not disappear upon lying down, secondary causes should be considered, and appropriate examinations should be conducted. The mass quickly disappears when the patient lies down. If the mass does not disappear upon lying down, secondary causes should be considered, and appropriate examinations should be conducted.
bubble_chart Treatment Measures
Not all cases of this disease require surgical treatment. For younger, unmarried individuals with symptoms, elevating the scrotum with a suspensory band can alleviate the symptoms, which may also disappear after marriage. For those with more severe symptoms, high ligation of the internal spermatic vein can be performed. This involves ligating all branches of the internal spermatic vein at the internal ring (Figure 1). If a fistula disease is left behind, it often leads to recurrence. After ligation of the internal spermatic vein, venous blood from the testis and epididymis can return via the external spermatic vein to the inferior vena cava or through subcutaneous venous branches below the external ring to the femoral vein (Figure 2). Some suggest ligating the internal spermatic vein in the retroperitoneal wall above the internal ring, reasoning that the vein is already a single branch there, preventing fistula disease. The drawback is that the location is deeper, exposure is poor, and tissue injury is greater. Once infection occurs, the retroperitoneal space has low resistance and is prone to spreading. Therefore, this method is not routinely used now and is reserved only for recurrent cases, particularly when there is significant adhesion from the original incision.

Figure 1: High ligation of the internal spermatic vein
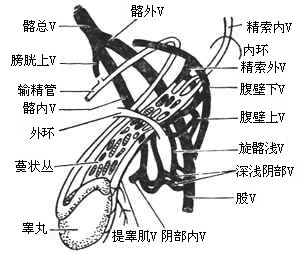
Figure 2: Venous return after ligation of the internal spermatic vein





