| disease | Tetracycline-stained Teeth |
| alias | Tetracycline Stained Teeth |
Tetracycline is an antibiotic biosynthesized by the catalytic dehalogenation of chlortetracycline, with low toxicity, and has been used clinically since 1948. In 1950, foreign reports emerged about tetracycline drugs causing tooth discoloration; subsequently, there were further reports of tetracycline depositing in teeth, bones, and even nails, as well as causing enamel hypoplasia. In this regard, it was not until the 1970s that domestic attention was drawn to the issue during the intermediate stage [second stage].
bubble_chart Etiology
During the development and mineralization of teeth, tetracycline antibiotics can be incorporated into the tooth structure, causing tooth discoloration.
Since enamel and dentin form simultaneously on opposite sides of a basal membrane, a single dose can create yellow layers in both tissues; however, the deposition in dentin is four times higher than in enamel, and in enamel, it appears only as diffuse, non-banded pigmentation (Figure 1). This is because dentin apatite crystals are smaller, resulting in a larger total surface area compared to enamel apatite crystals, allowing dentin to absorb significantly more tetracycline than enamel. Additionally, because the yellow layer is wavy and cap-shaped, roughly resembling the tooth's outline, a single dose-induced discoloration can be observed across most of the tooth's surface, whereas repeated doses at long intervals do not produce horizontal banding. Alongside tooth discoloration, bone tissue may also become stained, but the latter can gradually fade due to the physiological metabolic activity of bone tissue. In contrast, tooth discoloration is permanent. Furthermore, tetracycline can cross the placenta in pregnant women, causing discoloration of deciduous teeth.
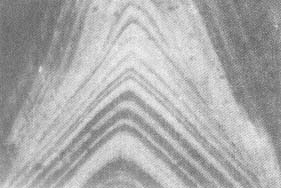
Figure 1 Tetracycline-stained tooth section under fluorescence microscopy
The primary effect of tetracycline on teeth is discoloration, sometimes accompanied by enamel hypoplasia. Due to the chelating properties of tetracycline molecules, they can form stable tetracycline-calcium orthophosphate complexes with dental tissues, which inhibit two phases of mineralization: nucleation and crystal growth.
The extent of tetracycline-induced tooth discoloration and enamel hypoplasia depends on the following factors:
① The inherent color of the tetracycline drug itself, e.g., demeclocycline appears cadmium yellow, while oxytetracycline is lemon yellow.
② The color derived from degraded tetracycline, as tetracycline is light-sensitive and can change color under UV or sunlight.
③ The depth of tetracycline binding in dentin affects the degree of discoloration; the closer the stained band is to the enamel-dentin junction, the more pronounced the discoloration. Thus, medication during early infancy, when outer dentin forms, has the greatest impact.
④ The structure of enamel itself plays a role. In severe enamel hypoplasia, where enamel is entirely lost, the stained dentin becomes visibly exposed. In contrast, with grade I enamel hypoplasia, where enamel loses translucency and appears chalky, it can mask the stained dentin, making the tooth color appear closer to normal.
bubble_chart Clinical Manifestations
1. It appears yellow and exhibits bright yellow fluorescence under sunlight, gradually changing from yellow to brown or dark gray. This transformation is slow and can be accelerated by sunlight, which is why the labial surface of the incisors discolors first.
2. The discoloration is more noticeable in anterior teeth than in posterior teeth, and more pronounced in deciduous teeth than in permanent teeth. This is because the enamel of deciduous teeth is thinner and more translucent, making it harder to mask the color of tetracycline-bound compounds in the dentin.3. The degree of tooth discoloration is related to the type, dose, and frequency of tetracycline administration. Generally, it is believed that oxytetracycline, demeclocycline, and tetracycline hydrochloride cause more noticeable discoloration than oxytetracycline and chlortetracycline. In permanent teeth, the number of tetracycline treatment courses is proportional to the degree of discoloration. However, a large dose administered over a short period has a greater effect than an equivalent total dose administered over a longer period.
4. Tetracycline-induced tooth discoloration and enamel hypoplasia only occur if the drug is administered during tooth development. Generally, if the drug is administered after the age of 6–7, it will not cause significant tooth discoloration. {|103|}
1. Medical History Received multiple short-term high-dose treatments (tetracycline-class drugs) before the age of 6-7.
2. Clinical Presentation Teeth appear yellow, light gray, or dark gray, with more pronounced discoloration in anterior teeth compared to posterior teeth, and in deciduous teeth compared to permanent teeth. Severe cases may present with enamel hypoplasia.
3. Differential Diagnosis Under ultraviolet light, tetracycline-stained teeth exhibit fluorescent excitation, which can help distinguish them from hereditary opalescent dentin. {|102|}
bubble_chart Treatment Measures1. Visible Light Composite Resin Restoration This method can refer to the treatment of dental fluorosis, but only 0.1mm of labial enamel should be ground or no grinding at all, as tetracycline staining primarily occurs in the dentin. Excessive grinding of the enamel layer or even exposure of the dentin not only intensifies the underlying color but also severely affects the bonding strength. For teeth with severe tetracycline staining, due to poor masking effects, this method may still yield unsatisfactory results.
2. Bleaching Method This can be attempted for cases without enamel defects. It can be divided into external bleaching and internal bleaching.
(1) External Bleaching: Clean the tooth surface and apply petroleum jelly to the gingival margin. Place absorbent paper soaked in 30% hydrogen peroxide solution on the labial surface of the anterior teeth, leaving a small distance from the gingival margin. Expose to infrared or incandescent light for 10 minutes. A course of treatment consists of 5–8 sessions. Experiments show that external bleaching does not reduce the fluorescent bands already present in the dentin, but the tooth color appears improved to the naked eye. However, the original tooth color typically returns within 0.5–1 year. High-concentration hydrogen peroxide can etch and demineralize the enamel, giving it a chalky appearance and reducing its original transparency, thereby diminishing the reflectivity of the stained dentin. Over time, the enamel remineralizes, transparency increases, and the color returns—this is a key reason for the so-called "color rebound."
(2) Internal Bleaching: This involves performing a pulpectomy for the purpose of bleaching. After a routine pulpectomy, the root canal filling material is reduced to 2–3mm below the cervical line. For bleaching, 30% hydrogen peroxide solution or a paste made from 30% hydrogen peroxide and sodium borate is sealed into the pulp chamber. The medication is changed every 3 days for a total of 4–6 sessions. Once the desired color is achieved, the cavity is filled with composite resin. This method effectively removes or alters the tetracycline bound to the dentin, significantly reducing fluorescence levels and yielding highly satisfactory clinical results. For individuals with occupational demands for aesthetics and no enamel defects, this method can be attempted. Its drawback is converting a vital tooth into a non-vital one. Although short-term efficacy is reliable, long-term outcomes require further observation.
To prevent the occurrence of tetracycline-stained teeth, tetracycline drugs should not be used by pregnant and lactating women, as well as children under 8 years of age.




