| disease | Horseshoe Kidney |
Horseshoe kidney is also a relatively common congenital anomaly, found in approximately one out of every 500 to 1000 autopsies, with males being more affected than females at a ratio of about 4:1. It can be detected at any age, with about half of the cases occurring between 30 and 40 years old.
bubble_chart Pathogen
Horseshoe kidney is formed by the fusion of the two kidneys at the root of the nose (more than 90% at the root of the nose) along the midline of the body. Generally, scholars believe that this abnormal kidney morphology results from the compression and fusion of nephrogenic tissue cells from both kidneys between the two umbilical stirred pulses during early embryonic development. The fusion mostly occurs at the root of the nose, forming the isthmus. The isthmus is composed of kidney excess substance (to varying degrees) and connective tissue, located anterior to the abdominal aorta and inferior vena cava, slightly above their bifurcation. Due to the restriction of fusion at the root of the nose, the two kidneys cannot rotate normally, causing the renal spinal angle to be opposite to the normal antagonism. The renal stirred pulse may originate from the iliac stirred pulse, the bifurcation of the abdominal aorta, or the inferior mesenteric stirred pulse. The ureters are shorter than normal and descend anterior to the isthmus to the bladder (Figure 1).
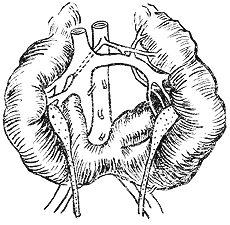
Figure 1 Horseshoe kidney
bubble_chart Clinical Manifestations
Horseshoe kidney can present clinically with three types of symptoms. The first type is pain and a mass in the umbilical region. The second type involves gastrointestinal disturbances, such as abdominal pain and constipation. The third type includes urinary system complications, such as infections, hydronephrosis, and stones. In reality, most cases are discovered during surgical exploration or are misdiagnosed as other abdominal conditions, such as appendicitis, pancreatitis, or duodenal ulcers.
bubble_chart DiagnosisThe diagnosis of this disease primarily relies on pyelography. On the pyelogram, it can be observed that the angle formed by the longitudinal axis of both kidneys and the spine (the renal-spinal angle) points downward, unlike the normal upward orientation. Occasionally, in intravenous pyelograms, if one kidney shows poor function or fails to develop due to technical conditions, the visualized kidney may be mistakenly identified as incomplete renal rotation. This point should be carefully considered during diagnosis.
bubble_chart Treatment Measures
Renal function is usually not significantly impaired in this disease, so no special treatment is required in the absence of complications. If there are infections, hydronephrosis, stones, or severe compression symptoms, appropriate treatment measures should be taken based on the specific situation.
infection; effusion; calculus





