| disease | Spinal Tuberculosis |
Vertebral subcutaneous nodes account for approximately 50-75% of all bone and joint subcutaneous node cases. They were previously more common in children but have become increasingly prevalent among young adults in recent years, with a slightly higher incidence in females than males. Multiple lesions predominantly occur in weight-bearing vertebrae, including the thoracic spine (40.3%), lumbar spine (35.97%), followed by the thoracolumbar junction (12.77%) and lumbosacral region (7.36%). About 3-7% of cases involve two vertebral lesions separated by unaffected vertebrae, known as skip vertebral subcutaneous nodes.
bubble_chart Pathogenesis
Spinal subcutaneous node lesions mostly occur in the vertebral body, with a few cases in the lamina, vertebral arch, spinous process, and transverse process.
(1) Central or juvenile type: Children have more cartilage components around the vertebral body. After the lesion develops in the central ossified part, collapse may occur, while the intervertebral space remains intact in the early stage.
(2) Marginal type: Also known as the epiphyseal or adult type, it occurs in older children or adults, originating from the epiphysis at the upper or lower edge of the vertebral body. The lesion often rapidly destroys the intervertebral soft tissues, narrowing or eliminating the intervertebral space, causing adjacent vertebral bodies to fuse.
(3) Anterior or subperiosteal type: Also occurring in adults, it is located in front of the vertebral ligament leukorrheal disease and often spreads to involve adjacent vertebrae above and below.
(4) Subcutaneous node in the appendages: Such as in the transverse process, lamina, pedicle, or spinous process, which is relatively rare.
Vertebral body lesions, due to circulatory disorders and subcutaneous node infection, lead to bone destruction and necrosis, caseous changes, and abscess formation. The vertebral body collapses due to the lesion and weight-bearing, causing spinal curvature, protrusion of the spinous process, and a hunchback deformity, particularly evident in thoracic subcutaneous nodes. Due to vertebral collapse, sequestrum, granulation tissue, and abscess formation, spinal cord compression can occur, leading to paraplegia, more commonly in the cervical and thoracic regions. Bone destruction and cold abscesses form along the anterior longitudinal ligament leukorrheal disease of the spine and may penetrate the ligament into the anterior spinal fascial space, spreading to distant areas due to gravity. Cervical subcutaneous node abscesses may appear anterior to the cervical spine, causing bulging of the posterior pharyngeal wall, leading to difficulty swallowing or breathing; they may also appear subcutaneously along the posterior edge of the sternocleidomastoid muscle. Thoracic subcutaneous nodes often form prevertebral and paravertebral abscesses, which may also appear in the posterior mediastinum or spread along the intercostal space to the chest wall; progression into the spinal canal can cause paraplegia. Lumbar subcutaneous node abscesses often extend into the pelvis, forming psoas abscesses, spreading downward along the iliopsoas muscle to the groin or medial thigh, reaching the greater trochanter from behind the femur, or extending along the tensor fasciae latae and iliotibial band to the lower lateral thigh; or spreading backward to the lumbar triangle. These abscesses, lacking acute inflammatory symptoms, are called cold abscesses. During the recovery process of spinal subcutaneous nodes, destructive products such as abscesses and sequestra may gradually be absorbed, while fibrous tissue fills and repairs the area, eventually leading to fibrous and bony healing, though the course is prolonged. However, with active treatment, the duration can be significantly shortened. bubble_chart Pathological ChangesI. Anatomical Key Points
The spine constitutes the central axis of the human body, supporting body weight, participating in the formation of the thoracic, abdominal, and pelvic cavities, and protecting the internal organs within these cavities, particularly the spinal cord.
To address lesions of the spine and spinal cord, surgical approaches and methods should be employed without compromising or minimizing damage to spinal stability. When necessary, measures such as bone grafting or internal fixation should be taken to reconstruct stability.
It is worth noting that the thoracolumbar region has unique biomechanical characteristics: ① It serves as a transition point between the relatively fixed thoracic vertebrae and the highly mobile lumbar vertebrae, making it prone to concentrated stress from the torso. ② It is the junction between the thoracic kyphosis and lumbar lordosis, where stress from weight-bearing is also concentrated. ③ The orientation of the articular facets changes in the thoracolumbar transition zone. Due to these biomechanical features, cases have been observed in practice where, within a short period (4–6 weeks), debridement or anterior-lateral decompression of the spinal canal was performed sequentially on the left and right sides of the vertebral body at the same level without internal fixation, leading to spinal instability, severe vertebral displacement, and exacerbation of spinal cord injury.
The Denis-Armstrong three-column theory was originally used for the classification and analysis of thoracolumbar fractures or/and spinal cord injuries. It also holds practical significance when applied to guide surgery for spinal subcutaneous nodules. In cases of spinal subcutaneous nodules, especially those involving multiple vertebrae, the anterior and middle columns of the vertebral body are already damaged to varying degrees. Therefore, during surgery, care should be taken to avoid damaging the remaining healthy bone of the affected vertebrae, particularly the posterior column. If laminectomy is performed to treat spinal subcutaneous nodules complicated by paraplegia, especially in the cervicothoracic or thoracolumbar regions, failure to apply internal fixation may lead to vertebral displacement and further spinal cord injury. After thorough lesion debridement, intervertebral (anterior and middle column) bone grafting should be performed, particularly in the thoracic and thoracolumbar regions, to restore height as much as possible and reconstruct spinal stability. This is crucial for preventing delayed-onset paraplegia caused by kyphotic deformity.
For the debridement of spinal subcutaneous nodules and other spinal surgeries, reviewing the anatomical relationships of the posterior mediastinum and retroperitoneal structures adjacent to the spine and its sides is highly beneficial.1. Posterior Mediastinum: Located below the sternal angle plane and above the diaphragm, bounded anteriorly by the pericardium and posteriorly by the lower thoracic vertebrae. Within the posterior mediastinum, the vertically arranged structures from top to bottom include: the trachea and bronchi (most anterior), the esophagus (central), the thoracic aorta and vagus nerve (posterolateral to the esophagus), and the thoracic duct, azygos vein, hemiazygos vein, and thoracic sympathetic trunk (immediately adjacent to the anterior and lateral aspects of the spine).
2. Lumbosacral Plexus: Runs posterolateral to the psoas major muscle, extending from superomedial to inferolateral. From top to bottom, the nerves include the iliohypogastric nerve, ilioinguinal nerve, lateral femoral cutaneous nerve, femoral nerve, and obturator nerve. During debridement of psoas abscesses, the lumbar plexus may be injured. Accidental injury to the genitofemoral nerve on the anterior surface of the psoas major can result in persistent postoperative neuralgia. Therefore, any cord-like structures encountered during surgery should be carefully preserved to avoid injuring these nerves (Figure 11).
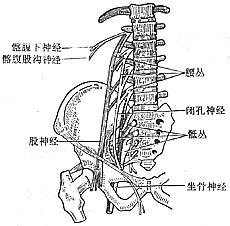
Figure 11: Lumbosacral Plexus
II. Pathological Types
Based on the initial location of the lesion, spinal subcutaneous nodules are classified into four types.
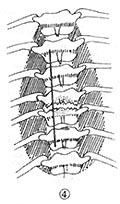
1. Central Type: The lesion originates in the cancellous bone at the center of the vertebral body. After destruction, the vertebral body collapses into a wedge shape. This type should be differentiated from vertebral tumors, especially metastatic carcinoma (Figure 12③).
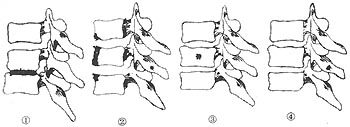
Figure 12: Schematic Diagram of Pathological Types of Spinal Subcutaneous Nodules
2. Epiphyseal type The most common, often involving the epiphyses of adjacent vertebrae simultaneously. Early X-ray films show disc space narrowing, accounting for about 75% of spinal subcutaneous nodule cases (Figure 12①).
3. Subperiosteal type Commonly seen at the anterior edge of thoracic vertebral bodies, the abscess spreads extensively beneath the anterior longitudinal ligament and subperiosteum, often causing destruction across multiple vertebral anterior edges. This type should be differentiated from vertebral erosion caused by thoracic aortic aneurysm (Figure 12②).
4. Appendicular type Refers to lesions primarily originating in the dense bone of spinous processes, transverse processes, laminae, or superior/inferior articular processes. Before the advent of CT, conventional X-ray imaging showed this type accounted for only 0.2–2% of spinal tuberculosis cases. It should be distinguished from tumors of vertebral appendages, particularly spinal metastases (Figure 12④).
bubble_chart Clinical Manifestations
(1) Systemic Symptoms The onset of the disease is insidious, with no clear date of occurrence. Patients experience fatigue, loss of appetite, low-grade fever in the afternoon, night sweating, and weight loss—all systemic toxic symptoms. Occasionally, a few cases may deteriorate acutely with a fever of around 39°C, often misdiagnosed as severe common cold or other acute infections. In some cases, there may be no systemic symptoms like low-grade fever, and the patient may only feel dull or radiating pain in the affected area, which can also be easily misdiagnosed as other diseases.
(2) Local Symptoms
1. Pain Dull pain in the affected area often appears simultaneously with systemic symptoms like low-grade fever. It worsens during activity, riding on bumpy roads, coughing, or sneezing, and improves with bed rest. Nighttime pain is more severe and can radiate along spinal nerves: upper cervical pain may radiate to the occipital region, lower cervical pain to the shoulder or arm, and thoracic pain along intercostal nerves to the upper or lower abdomen, often misdiagnosed as cholecystitis, pancreatitis, or appendicitis. Lower thoracic vertebrae 11–12 may radiate along the inferior gluteal nerves to the lower back or buttocks, leading to X-rays often focusing only on the lumbar spine, thus frequently misdiagnosing lower thoracic lesions as fistula disease. Lumbar vertebral disease often radiates along the lumbar plexus to the front of the thigh, occasionally involving the back of the leg, and is easily misdiagnosed as disc herniation.
2. Abnormal Posture This is caused by paravertebral muscle rigidity and spasm due to pain. Patients with cervical subcutaneous node often exhibit torticollis, forward head tilt, shortened neck, and hands supporting the jaw. A posture with a protruding chest and abdomen is common in thoracolumbar or lumbosacral structural issues.
Normally, one can bend to pick up objects, but patients cannot bend and instead flex their hips and knees, supporting one knee with a hand while picking up objects—this is called a positive picking-up test (Figure 13).
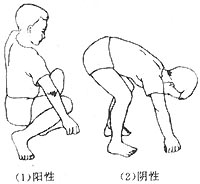
Figure 13 Picking-up Test
Young children may not extend their back. To test, have them lie prone, and the examiner lifts their feet. Normally, the spine curves naturally backward (Figure 14), but in affected children, the diseased vertebrae remain fixed or paravertebral muscles spasm, preventing back extension.
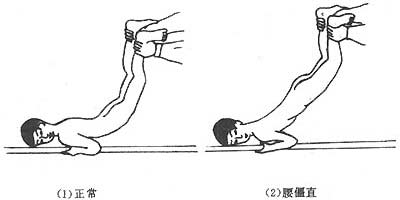
Figure 14 Juvenile Spinal Mobility Test
3. Spinal Deformity For the cervical and lumbar spine, check for loss of physiological lordosis; for the thoracic spine, check for increased physiological kyphosis. Palpate each spinous process from top to bottom for abnormal protrusions, especially localized angular kyphosis, which is common in spinal subcutaneous node and differs from the rounded kyphosis seen in adolescent vertebral epiphyseal chondropathy, ankylosing spondylitis, or poor posture.
4. Cold Abscess At the time of consultation, 70–80% of spinal subcutaneous node cases are complicated by cold abscesses. Deep paravertebral abscesses can be visualized via X-ray, CT, or MRI. Abscesses may spread along muscle fascial planes or neurovascular bundles to form multiple abscesses on the body surface. Atlantoaxial lesions may cause retropharyngeal abscesses, leading to dysphagia or respiratory obstruction; mid-to-lower cervical abscesses appear in the anterior or posterior cervical triangles; thoracic subcutaneous node may present as tense fusiform or columnar abscesses along the vertebral body (Figure 15), spreading along intercostal neurovascular bundles to the chest or back, rarely penetrating the lungs, pleural cavity, or even the esophagus and thoracic aorta; thoracolumbar or lumbar abscesses may spread along one or both iliopsoas muscles or their substance to the retroperitoneum, occasionally penetrating fixed organs like the colon, and extending downward to the iliac fossa, groin, buttocks, or legs; sacral abscesses often collect anterior to the sacrum or spread along the piriformis through the greater sciatic foramen to the vicinity of the greater trochanter (Figure 16). Understanding the pathways and locations of cold abscess spread aids in diagnosis.
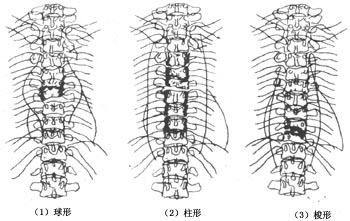
Figure 15 Types of Paravertebral Abscesses in Thoracic Subcutaneous Node

Figure 16 Spine subcutaneous node Cold abscess Multiple abscess Pathway
5. Sinus Cold abscesses can extend to the body surface and may resolve spontaneously with treatment or rupture on their own to form a sinus. If the sinus becomes secondarily infected, the condition will worsen, making treatment difficult and the prognosis poor. This should be avoided as much as possible.
6. Spinal cord compression Signs of spinal cord compression should be monitored in patients with vertebral subcutaneous nodules, especially those in the cervical or thoracic spine above the conus medullaris. Attention should be paid to any neurological dysfunction in the limbs to facilitate early detection of spinal cord compression complications.
bubble_chart Auxiliary Examination
Imaging Examination
(1) X-ray Radiography In the early stages of the disease, X-ray findings are mostly negative. According to Lifeso et al. (1985), conventional X-ray radiography can only reveal abnormalities approximately 6 months after onset, when 50% of the vertebral bone is affected.
Early X-ray signs in most cases initially show an enlarged paravertebral shadow, followed by involvement of the anterior inferior edge of the vertebra, narrowing of the intervertebral space, osteopenia of the vertebral body, an enlarged paravertebral shadow, and sequestra. For vertebral bone destruction areas with a diameter <15 mm, lateral radiographs often fail to reveal them, whereas tomographic radiographs can detect destruction areas with a diameter as small as 8 mm. Sequestra of varying sizes may be visible in the cancellous bone of the vertebra or within abscesses.
In central vertebral subcutaneous node vertebrae, the intervertebral space often shows no significant changes, making it difficult to distinguish from vertebral tumors. However, some slow-growing tumors such as thyroid metastatic carcinoma, chordoma, and cervical malignancy with cachexia may exhibit varying degrees of intervertebral narrowing, making differentiation from epiphyseal vertebral subcutaneous nodes extremely challenging.
Typically, in vertebral subcutaneous node cases, except for old or nearly cured patients, the enlarged paravertebral shadow is mostly bilateral. However, spinal tumors such as vertebral giant cell tumor of bone, chordoma, cervical malignancy with cachexia, and kidney cancer spinal metastases may show unilateral or bilateral enlarged paravertebral shadows on anteroposterior X-ray radiographs, particularly when limited to one side, necessitating careful differentiation.
(2) CT Examination CT can detect subtle bone changes and the extent of abscesses early, and is particularly valuable for areas where conventional X-ray radiography is less effective, such as the atlantoaxial joint, cervicothoracic spine, and irregularly shaped sacrum. Some scholars classify spinal subcutaneous node CT images into four types: ① Fragmented type: Small fragments remain after vertebral destruction, with low-density soft tissue shadows adjacent to the vertebra, often containing scattered small fragments; ② Osteolytic type: Osteolytic destruction areas are present at the anterior edge or center of the vertebra; ③ Subperiosteal type: Irregular bony destruction is seen at the anterior edge of the vertebra, with annular or semi-annular calcifications often visible in the paravertebral soft tissues; ④ Localized bone destruction type: The destruction area is sometimes surrounded by a sclerotic band (Jainr et al., 1993).
Among spinal subcutaneous node CT examinations, the fragmented type is the most common, and spinal tumors often exhibit similar features, necessitating comprehensive analysis with clinical data. For example, the presence of calcifications or small bone fragments within an enlarged paravertebral shadow aids in the diagnosis of spinal subcutaneous nodes. Despite this classification, CT sometimes still cannot differentiate between spinal subcutaneous nodes and spinal tumors.
(3) MRI Examination MRI offers high soft tissue resolution and is superior to CT for examining the brain and spinal cord. It can perform imaging scans in sagittal, axial, and coronal planes of the spine. In spinal subcutaneous node MRI, the affected vertebrae, discs, and appendages exhibit signals compared to their normal counterparts: higher signals indicate hyperintensity, while lower signals indicate hypointensity.
1. Vertebral Lesions T1-weighted images show hypointensity at the lesion site, sometimes mixed with short T1 signals. T2-weighted images of vertebral lesions show enhanced signals. The images reveal not only signal changes in the affected vertebrae but also the outline of vertebral destruction, altered alignment due to vertebral collapse, and enlarged paravertebral shadows.
2. Paravertebral Abscesses Paravertebral abscesses in spinal subcutaneous nodes appear as hypointense signals on T1-weighted images and as hyperintense signals on T2-weighted images. Coronal images can delineate the outline and extent of paravertebral abscesses or bilateral psoas abscesses.
3. Disc Changes Narrowing of the intervertebral disc on X-ray radiographs is one of the early signs of spinal subcutaneous nodes. On MRI, T1-weighted images show hypointense and narrowed discs. Normally, the nucleus pulposus exhibits fine transverse fissures on T2-weighted images, which disappear in the presence of inflammation, allowing early detection of disc inflammatory changes.
MRI is more sensitive than any other imaging examination, including ECT, in the diagnosis of early spinal subcutaneous nodes. In patients with suspected spinal subcutaneous nodes who present with clinical symptoms for 3 to 6 months but show no abnormalities on X-ray films, MRI can reveal the affected vertebral bodies and paravertebral soft tissues (abscesses), with T1-weighted images showing low signal intensity and T2-weighted images showing high signal intensity. Early spinal subcutaneous node MRI findings can be divided into three types: ① vertebral inflammation; ② vertebral inflammation with abscess; ③ vertebral inflammation, abscess, and discitis. It is worth noting that when the affected vertebral body is in the inflammatory phase without changes in soft tissue or disc signal, it cannot be distinguished from vertebral tumors, and a biopsy should be performed if necessary for confirmation.
The diagnosis of typical cases is usually not difficult based on medical history, symptoms, signs, and imaging examinations. However, diagnosing early-stage cases without obvious abnormalities on X-rays is very challenging. It is essential to be familiar with the clinical symptomatology and signs of the disease, make a preliminary assessment of the affected spinal region, and conduct imaging and laboratory tests. If necessary, a puncture or even an open pathological biopsy should be performed.
bubble_chart Treatment Measures
(1) Non-surgical Treatment For patients with spinal subcutaneous nodules who do not meet the surgical criteria, appropriate chemotherapy regimens (refer to the general principles) and local immobilization should be applied. Patients with low-grade fever, back pain, or biomechanical instability should rest on a hard bed. Glisson belt traction or a Halo-vest is suitable for patients with cervical spine instability. For patients with large retropharyngeal abscesses in the atlantoaxial subcutaneous nodules that affect breathing or swallowing, puncture and aspiration of pus may be performed.
Application of the Halo-Vest: The Halo-Vest was initially used in the 1950s as a traction device for cervical spine diseases causing cervical instability. Compared to other traction devices such as traction clamps or the Minerve gypsum vest, it offers significant advantages over traditional external fixation methods. After fixation, patients achieve three-dimensional stability. They can sit up, stand, and walk, thereby reducing bed rest time and avoiding other complications.
1. Indications Caution should be exercised for patients over 60 years old or those with poor cardiopulmonary function.
(1) Cervical spine reduction: fractures, fracture dislocations, and subluxations.
(2) External fixation for cervical spine instability: fracture dislocations, rheumatoid arthritis, primary or metastatic tumors, and unstable atlantoaxial subcutaneous nodules.
2. Structure of the Halo-Vest The Halo-Vest consists of three main components: the halo ring and skull pins, a plastic vest, and adjustable metal struts connecting the halo ring to the vest. Different sizes of Halo-Vests can be selected based on the patient's head and torso dimensions. During installation, the halo ring should be positioned approximately 1–1.5 cm from the scalp. The plastic vest can be chosen according to the patient's chest circumference. Additional accessories include skull pins, hex nuts, turnbuckles, shoulder straps, and vest straps.
3. Installation and Fixation of the Halo-Vest The halo ring should be sterilized under high pressure before use. The hair at the installation site on the patient's skull should be shaved, and the skin should be scrubbed and disinfected.
The patient should be given a small dose of sedative before the procedure and placed supine on a bed with the head positioned beyond the edge, supported by a thin board. The halo should be placed below the maximum cranial circumference, approximately 1 cm above the eyebrow and 1 cm above the auricle. The anterior skull pins should be fixed 1 cm above the lateral third of the forehead, while the posterior pins should be diagonally opposite the anterior pins, approximately 1.5 cm below the ear. Mark the fixation points for the skull pins. After local disinfection and procaine injection, the skull pins should be inserted at a 90-degree angle into the outer table of the skull, but not too deeply, to ensure the halo ring remains securely fixed and prevents slippage during traction.
First, place the back panel of the plastic vest on the patient's back, then position the front panel and secure the front and back panels with nylon straps. Connect the halo ring to the vest by adjusting the turnbuckles, shoulder straps, chest straps, and back straps.
After the Halo-Vest is installed, anteroposterior and lateral cervical spine X-rays should be taken. If necessary, adjust the traction direction and force of the halo ring to achieve the desired fixation.
(II) Surgical Treatment According to surgical indications, elective debridement of the lesion is performed after the systemic symptoms of subcutaneous node poisoning have subsided. The surgical approach is selected based on the patient's condition, objective circumstances, and the surgeon's familiarity with the approach. For thoracic subcutaneous nodes, the extrapleural approach is generally used. For patients under 60 years of age with acceptable cardiopulmonary function, long paravertebral abscesses, destruction of 4–6 vertebral bodies, extensive sequestra, or cases requiring anterior spinal bone grafting, or when paravertebral abscesses penetrate the thoracic cavity or lungs, transthoracic debridement may be considered. For lumbar subcutaneous nodes, the extraperitoneal approach is employed. Principles for debridement of multi-segmental (skip-type) subcutaneous node lesions in the spine: ① Priority is given to lesions that may cause paralysis; ② If the severity of lesions in two segments is similar, the upper segment is addressed first, while the lower segment is treated later; ③ The more severe lesion is treated first, while milder lesions may heal with non-surgical treatment; ④ Cervical subcutaneous nodes have good blood supply and can heal without surgery. For spinal subcutaneous nodes complicated by sinus tracts that do not heal after 3–6 months of non-surgical treatment, surgery may be considered. Postoperative care for spinal subcutaneous nodes typically involves bed rest for 6–8 weeks. Patients may begin mobilization exercises when spinal pain subsides, existing abscesses disappear, body temperature normalizes, erythrocyte sedimentation rate (ESR) decreases, and spinal stability is confirmed. Initially, patients should focus on managing daily activities independently, then gradually increase physical activity while adhering to the full course of chemotherapy.
1. Cervical spine1-2subcutaneous node lesion debridement. Cervical spine1-2subcutaneous nodes are relatively rare, accounting for 0.27% of spinal subcutaneous nodes. Their abscesses can cause difficulty in swallowing and breathing in patients, while leading to limb paralysis is uncommon.
(1) Preoperative preparation: Pay attention to oral hygiene, treat infections in the nose and throat, and perform nebulized inhalation and gargling with gentamicin sulfate solution 2-3 days before surgery. For patients with cervical spine instability, cervical spine1-2subluxation or dislocation, occipitomandibular traction or skull traction should be performed preoperatively.
(2) Position: Supine position, with soft pillows placed under both shoulders and the root of the neck to extend the neck, but not hyperextend. Small sandbags are used to fix both sides of the head.
(3) Anesthesia: First, perform a tracheostomy under local anesthesia, then insert a tube through the tracheostomy site for general anesthesia.
(4) Procedure: Use a mouth gag to open the mouth, and disinfect the oral and posterior pharyngeal wall mucosa with 0.1% benzalkonium bromide solution.
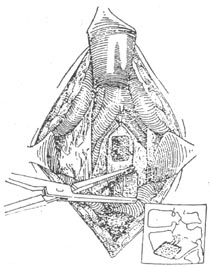
Incision: Suture the uvula to the soft palate with silk thread, depress the tongue root with a tongue depressor, and block the entrance of the esophagus and trachea with fine gauze to prevent blood or pus from flowing in. At the midline of the bulging abscess on the posterior pharyngeal wall, make a 1 cm longitudinal incision with a sharp knife, aspirate all the pus, then extend the incision to 3-4 cm (Figure 1①). This midline area has no special blood vessels.
After incising the abscess, aspirate all the pus, insert a curette to thoroughly remove sequestra, granulation tissue, and caseous necrotic tissue. Then, under the periosteum, dissect bilaterally, being careful not to exceed the lateral masses of the atlas to avoid injuring the vertebral artery. When curetting the posterior part of the lesion, take care not to injure the spinal cord. After complete debridement, thoroughly irrigate and close the wound in two layers (Figure 1②③).
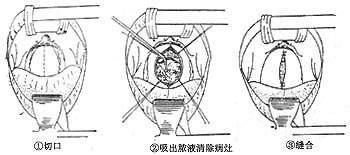
Figure 1: Cervical spine1-2subcutaneous node lesion debridement
Due to anatomical constraints, the surgical field is limited, making thorough debridement difficult. Additionally, the anterior arch of the atlas has little cancellous bone, leading to a high infection rate, which can affect bone graft survival. Note that excessively large bone grafts may make wound closure difficult. Fang (1983) reported 4 cases of bone grafting, with 2 cases of slippage. Severe infections can lead to encephalitis or meningitis, which may be fatal. Therefore, posterior occipital-cervical bone graft fusion may be necessary during seasonal epidemics.
(5) Postoperative management: Intravenous fluids should be administered for 2-3 days postoperatively. Once the local condition improves, a residue-free liquid diet can be started. Due to the high risk of throat infection, additional anti-infective medications should be used postoperatively. The tracheostomy tube can be removed 3-5 days after surgery, once respiratory inflammation subsides, secretions decrease, and the airway is clear. First, attempt to block the tracheal tube; if respiratory, expectoration, and vocal functions remain good after 24-48 hours, the tube can be removed. After removal, the wound does not need suturing; simply disinfect the area and cover it with sterile gauze. Continue occipitomandibular traction for 6-8 weeks. If the atlantoaxial joint is stable and the condition improves, the patient can gradually begin ambulation with a cervical collar for protection.
2. Cervical spine3-7Thoracic spine1subcutaneous node lesion debridement
(1) To debride lesions in these cervical spines, including thoracic spine1subcutaneous nodes, the commonly used surgical approaches are an oblique incision along the anterior border of the sternocleidomastoid muscle or a transverse incision on one side of the neck. The latter aligns with the natural skin lines of the neck, avoiding postoperative scar contracture and aesthetic issues. Patients with slender necks and drooping shoulders can more easily access thoracic spine1, but for robust patients with short, thick necks, debriding thoracic spine1lesions, especially for anterior vertebral bone grafting, a transverse neck incision may be unsatisfactory.
(2) Anesthesia: Local anesthesia can be used for cooperative patients, while general anesthesia is preferred for children and uncooperative patients.
(3) Position: Supine position, with soft pillows placed under both shoulders, allowing the head and neck to naturally extend backward but not excessively. A slightly firm pillow is placed under the neck to maintain its position, and a small sandbag is placed on each side of the head for fixation. The upper body is elevated by approximately 15° to reduce venous congestion in the head and neck.
4) Operative Steps
1) Incision The oblique incision is located along the anterior border of the right sternocleidomastoid muscle, extending from the mastoid process of the temporal bone down to the suprasternal notch, centered on the lesion, approximately 10 cm in adults. The right side is often chosen for ease of operation and to avoid accidental injury to the recurrent laryngeal nerve. If the lesion or cold abscess is predominantly on the left side, the left side is naturally selected.
The transverse incision starts from the midpoint of the sternocleidomastoid muscle on the operative side, crosses the midline of the neck by about 2 cm, with a total length of 5–7 cm. The height of the incision is determined by the location of the lesion (Figure 2①).
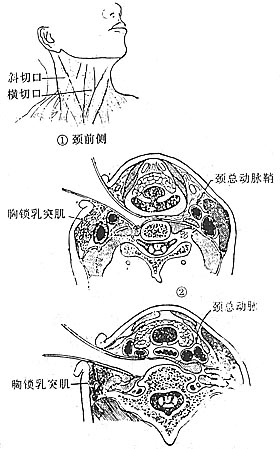
Figure 2 Cervical Vertebrae 3–7
Subcutaneous Node Lesion Debridement (Anterolateral Approach) 2) Surgical Method Incise the skin, subcutaneous tissue, and platysma muscle. Superficial venous branches or the external jugular vein that obstruct the operation may be ligated and divided. Sharply and bluntly dissect the deep cervical fascia, especially when using a transverse incision. The longitudinal dissection should be wider than the transverse to ensure adequate exposure of the anterior vertebral body. Expose the anterior and middle cervical fascia at the lower part of the incision. Incise the anterior cervical fascia, retract the sternocleidomastoid muscle laterally, and dissect the omohyoid muscle, dividing it at its tendinous portion. Separate the sternocleidomastoid muscle from the carotid sheath. To expose lesions at cervical vertebrae 3–4
, retract the carotid sheath, thyroid gland, constrictor muscles of the pharynx, and larynx toward the midline, and retract the sternocleidomastoid muscle laterally. Care must be taken to avoid injuring the accessory nerve, which enters the upper third of this muscle. The anterior scalene muscle, longus colli muscle, and bulging retropharyngeal abscess can then be exposed. If no abscess is present, especially in pediatric patients, do not mistake the anterior tubercle of the transverse process for the vertebral body. If necessary, perform an X-ray to confirm the lesion’s location. To expose cervical vertebrae 5–6–7 or thoracic vertebra 1 , retract the carotid sheath and sternocleidomastoid muscle laterally, and the visceral sheath (thyroid, trachea, and esophagus) medially to reveal the prevertebral fascia (Figure 2②③).
For better surgical access, the transverse cervical artery and vein may be ligated and divided. Near the sternoclavicular joint and the medial border of the anterior scalene muscle, the subclavian vein and internal jugular vein converge to form the brachiocephalic vein. This convergence angle is called the venous angle, with the thoracic duct on the left and lymphatic ducts on the right draining into the vein. Extreme care must be taken to avoid injury during surgery. If a prevertebral abscess is present, the area will appear swollen, with edema and petechiae on the fascial surface. Perform a trial aspiration to confirm the lesion’s location. If vertebral destruction is not severe, the esophagus can be seen moving up and down during swallowing (under local anesthesia) at the level of cervical vertebra 6 and below. Note this carefully. At the midline of the vertebral body, symmetrically grasp the fascia with forceps, lift it, and make a longitudinal incision between the forceps. Suture and ligate the edges for traction, thereby accessing the prevertebral space. If pus is present, aspirate it completely. Dissect beneath the periosteum to the longus colli muscles on both sides of the vertebral body, reaching the anterior longitudinal ligament.
Further extend the fascial incision longitudinally to expose the vertebral body, avoiding injury to the sympathetic chain, vertebral artery, and vessels of the longus colli muscle. To expose cervical vertebra 7 and thoracic vertebra 1 , the sternal head of the sternocleidomastoid muscle attached to the sternum may be divided to facilitate access to the affected vertebra, taking care not to injure the dome of the pleura. During vertebral exposure, minor bleeding points should be ligated or cauterized. The superior thyroid artery, superior laryngeal nerve, hypoglossal artery, external carotid artery and its branches, middle thyroid vein or inferior thyroid artery, and recurrent laryngeal nerve need not be specifically exposed or addressed unless they interfere with the operation.
When removing the lesion, after aspirating the pus, scrape off the subcutaneous nodular granulation tissue, caseous material, and dead bone on the abscess wall. Further clarify the location of the lesion and its anatomical relationship, then enlarge the bone lesion entrance with rongeurs to thoroughly remove the lesion and excise the remaining intervertebral disc. When curetting the posterior aspect of the lesion, take care to avoid injuring the spinal cord. After lesion removal, thoroughly rinse with saline solution.
In patients with large bone defects, a rectangular or square bone trough is made on the anterior or anterolateral side of the lesion (vertebral body) using a trephine, rongeur, or sharp curette. This process avoids the use of osteotomes to prevent vibration or accidental injury to the spinal cord. A suitable bone graft is harvested from the iliac crest. The anesthesiologist should apply appropriate cervical traction but avoid over-traction to prevent spinal cord injury, and the bone graft is then implanted. The graft should not protrude anteriorly beyond the vertebral body or compress the spinal cord posteriorly. For patients with seasonal external contraction disease, the head should be gently rocked side to side to ensure the graft remains stable and does not dislodge. The area is then irrigated again. Hemostasis is thoroughly achieved, local antibiotics are applied, and the prevertebral soft tissues are tightly sutured to maintain the correct position of the graft. For large abscess cavities, a silicone or rubber drainage tube may be placed.
(5) Postoperative management: A liquid diet is started 48 hours postoperatively, and the drainage tube is removed. The occipitomandibular brace is worn continuously for 2–3 months until the bone graft fuses, after which a cervical collar is worn for ambulation.
3. Thoracic Spine 2–12 Subcutaneous node debridement via thoracic approach: The thoracic approach for debridement of thoracic subcutaneous node lesions offers the following advantages over the traditional extrapleural route: a wider surgical field for thorough lesion removal, anterior vertebral bone grafting to maintain spinal stability, and the ability to address lung or pleural lesions simultaneously. Caution is advised for patients with poor pulmonary function (maximum ventilation capacity below 40% of predicted), cardiovascular diseases, or the very young or elderly. Long-term practice has shown no risk of thoracic infection with this approach.
Anesthesia: General anesthesia with endotracheal intubation. For lesions at thoracic 2–4 or thoracic 11–12 , bronchial intubation is used to collapse the lung on the operative side for better exposure.
Position: Lateral decubitus position with the operative side up. Both arms are extended forward at 90° and placed on a double-layer armrest. The lower leg is kept straight, while the operative-side leg is flexed at the hip (45°) and knee (90°). A soft pillow is placed between the legs, secured with a knee strap, and the pelvis is stabilized with a restraint belt to maintain position.
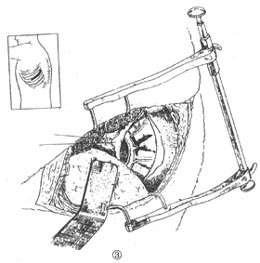
Operative steps:
(1) Incision: A posterolateral thoracic incision is made on the side with larger paravertebral abscesses, severe vertebral destruction, abscess penetration into the lung or pleural cavity, or poorer lung ventilation as estimated from chest X-rays. However, for thoracic 2–5 subcutaneous nodes, a right-sided thoracic approach is more convenient; for mid-thoracic 6–10 subcutaneous nodes, either side is suitable; for thoracic 11–12 subcutaneous nodes, the side depends on the height of the diaphragmatic attachment (refer to lateral thoracic X-rays), with the left side generally offering better exposure.
Three types of surgical incisions: For thoracic 2–5 subcutaneous nodes, the posterior end starts anterior to the lateral border of the sacrospinalis muscle and the medial border of the scapula, curves downward around the inferior angle of the scapula, and ascends to terminate at the anterior axillary line, forming a U-shaped incision.
For thoracic 6–10 subcutaneous nodes, the posterolateral thoracic incision starts at the lateral border of the sacrospinalis muscle on the operative side, follows the direction of the rib to be resected, and ends at the anterior axillary line.
For thoracic 10–12 subcutaneous nodes, the incision follows the direction of the 9th rib.
Schematic diagrams of the three surgical incisions are shown in Figure 3①②③④.
|
|
|
|
|
|
Figure 3 Transthoracic thoracic spine2~12subcutaneous node lesion debridement
①Incision site ②Axial schematic ③Condition after thoracotomy ④Location of paravertebral abscess incision
Depending on the level of vertebral lesions, in general, the resected rib should be 1-2 ribs higher than the lesion level; otherwise, it will be difficult to manage the lesion and paravertebral abscess. A corresponding segment of the rib is resected, with the anterior end not exceeding the costal cartilage and the posterior end excluding the rib head.
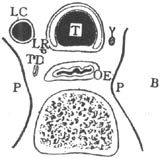
Taking the thoracic spine7~9subcutaneous node as an example, the skin and subcutaneous tissue are incised, hemostasis is ensured, and at the muscular weak point under the scapular angle, i.e., the auscultatory triangle, the muscle is incised down to the rib. The left middle and index fingers are placed under the chest wall muscles and lifted upward, the latissimus dorsi and the underlying serratus anterior are incised forward to the anterior axillary line, and the trapezius and water calptrop base peel muscles are incised backward to the edge of the sacrospinalis.The loose tissue between the subscapularis and intercostal muscles is separated, and a retractor is used to lift the scapula. The right hand is inserted under the scapula, counting the ribs from the second rib downward to identify the rib sequence. Typically, the fourth rib is resected, and the rib is removed subperiosteally, preserving the rib for potential bone grafting. During rib resection, the intercostal vascular pedicle can also be preserved to facilitate vascularized rib grafting between the vertebrae, making the bone graft more likely to survive. In pediatric patients, the rib may not need to be resected, and the thoracic cavity can be accessed through the intercostal space. When dealing with mid- and lower-thoracic subcutaneous nodes, the rib to be resected can also be identified by counting upward from the 12th rib. After entering the thoracic cavity, an automatic retractor is used to spread the thorax. If there are adhesions in the thoracic cavity, the visceral and parietal pleura are separated bluntly and sharply, ensuring thorough hemostasis. A wide hook is used to retract the lung toward the midline. In cases with bronchial intubation, the lung on the operative side can collapse at this point, allowing direct visualization of the prevertebral abscess. In the right thoracic spine3~4, the azygos vein can be seen in the posterior mediastinum. The azygos vein, at the height of T4, wraps around the posterior esophagus, crosses the dorsal side of the right bronchus, and forms the azygos arch before draining into the superior vena cava. Branches of the azygos vein can be ligated, but the azygos arch generally does not interfere with the surgery and does not require intervention. When accessing through the left thoracic cavity, the descending thoracic aorta can be seen below the T4 plane. After entering the thoracic cavity, the descending thoracic aorta shifts toward the contralateral side with the mediastinum and does not hinder the procedure. The hemiazygos vein is often covered by the thoracic aorta. The T1~4vertebral bodies are separated from the esophagus only by the anterior longitudinal ligament and the terminal end of the longus colli muscle, so care must be taken to avoid injuring the esophagus. At other levels, the esophagus has little relation to the spine (Figure 4). Figure 4 Anterior anatomical relationship of T1~4vertebrae A. Thoracic Vertebra 1 Cross Section B. Thoracic Vertebra 2 Cross Section C. Thoracic Vertebra 3 Cross Section Th.G. Thyroid Gland C. Common Carotid Artery LC. Left Subclavian Artery LR. Left Recurrent Laryngeal Nerve OE. Esophagus P. Pleura T. Trachea TD. Thoracic Duct VA. Azygos Vein V. Right Vagus Nerve A. Aorta (2) Debridement of the Lesion
Through the thoracic cavity, along the anterior side of the abscess of the affected vertebral body and偏向 the surgical side, the paravertebral abscess is longitudinally incised. The incision should not be too close to the intervertebral foramen to avoid injury to the segmental stirred pulse supplying blood to the spinal cord through the intervertebral foramen. In the upper thoracic spine, the rib heads, especially T2–4, should also be avoided to prevent injury to the sympathetic chain.
Two hemostatic forceps are symmetrically clamped along the longitudinal axis of the paravertebral abscess, and an incision is made between the forceps. The paravertebral abscess wall is penetrated with No. 7 silk thread to suture and ligate the blood vessels.
After incising the abscess wall, subperiosteal剥离 is performed within the abscess cavity to the left and right sides, exposing the affected vertebra. The剥离 should extend as far as possible to the contralateral paravertebral groove to fully expose the lesion. The surrounding abscess, caseous material, sequestra within the vertebral body, and necrotic intervertebral discs are then cleared.
(3) Intervertebral Bone Grafting
Severe destruction of the vertebral body that compromises spinal stability, particularly to prevent kyphotic deformity in pediatric patients, can be effectively addressed with solid intervertebral bone grafting. A bone trough is created in the vertebral body using a trephine at the site of the bone defect, and a large autologous iliac bone graft is embedded. Alternatively, two segments of rib bone may be implanted into the trough. Implanting a single rib often leads to subsequent fracture, slippage, or sinking into the vertebral cancellous bone, failing to achieve the desired outcome.
When creating the bone trough for intervertebral bone grafting in children, healthy vertebral bone should be preserved as much as possible to avoid affecting future vertebral growth and development.
Upon completion of the procedure, the lesion is irrigated with生理盐水. Locally, 200 mg of INH adsorbed onto gelatin sponge is applied, maintaining an effective concentration for one month (this will not be repeated in subsequent chapters). The incised anterior vertebral abscess wall is tightly and间断缝合 with No. 7 silk thread in full thickness. The thoracic cavity is irrigated, and a drainage tube is placed at the 7th–8th or 8th–9th intercostal space along the posterior axillary line. The thoracic cavity is closed, and the胸膜, intercostal muscles, and layers of the chest wall muscles and skin are缝合 in layers.
Postoperative Management:
The patient is placed on a hard bed and assisted with expectoration to maintain respiratory tract patency, preventing pulmonary infection and atelectasis. The通畅 of the thoracic drainage tube and changes in负压 should be monitored to prevent blockage by blood clots or纤维蛋白 leucorrhea. If the drainage tube becomes blocked, gentle finger compression or冲洗 with sterile生理盐水 can be used to maintain通畅. The volume, color, and characteristics of the drainage fluid should be recorded daily. The drainage tube is removed 48–72 hours postoperatively. Patients with intervertebral bone grafting should remain卧床 for 3–6 months. Those with large bone defects and spinal instability should wear a brace for protection during rehabilitation exercises.
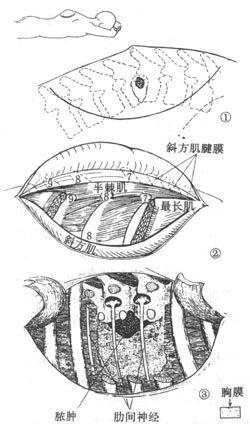
4. Thoracic Subcutaneous Node Debridement via Extrapleural Approach
The advantage of this procedure is its suitability for children and elderly or frail patients, especially those with poor cardiopulmonary function. Postoperative management is simple, and pulmonary complications are fewer. However, debridement of contralateral lesions is less thorough compared to the transthoracic approach. Here, the thoracic7–8subcutaneous node is used as an example for illustration.
Positioning: The patient is placed in the lateral decubitus position, with the side of greater vertebral destruction and larger paravertebral abscess as the surgical side. The torso is stabilized with soft pillows and约束带.
Anesthesia: General anesthesia with endotracheal intubation.
Operative Steps:
(1) Incision
A curved incision is made centered on the affected vertebra, 5–6 cm from the midline of the spinous process (Figure 5①). The浅筋膜 is incised along the direction of the incision.
Figure 5: Thoracic Subcutaneous Node Debridement via Extrapleural Approach (adapted from Roof)
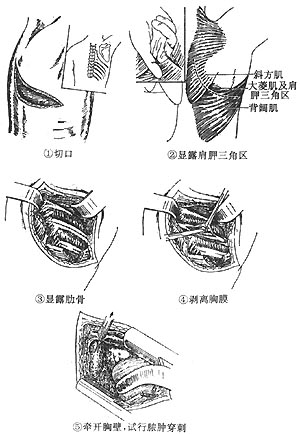
① Incision ②, ③ Process of exposing the lesion (2) Exposing the Lesion Peel the medial flap, longitudinally incise the trapezius muscle and the attachment of the water calptrop base peel-shaped muscle along the spinal border, and retract them laterally. Make a longitudinal incision in the thinner part of the sacrospinalis muscle 5cm from the spinous process, retract the muscle medially and laterally to expose the ribs. Along the direction of the rib to be removed, incise the rib membrane for 7-8cm and peel it. Cut the rib 6-7cm from the rib neck, use Koch's forceps to grasp the proximal end of the rib and pull it outward. At this point, sever the costovertebral joint, use an eyebrow chisel to pry open the rib head and neck, taking care not to injury the chest membrane, and remove the entire rib head and neck. Then bite off the corresponding transverse process. At this point, paravertebral pus can be seen overflowing. After aspirating all the pus, locate and ligate the intercostal arteries and veins, preserving the intercostal nerves as much as possible. Using the same method, remove a segment of the ribs above and below the lesion center, including the rib heads, necks, and their corresponding transverse processes, to expand the surgical field for lesion clearance. However, to maintain spinal stability, preserve the transverse processes as much as possible without compromising the exposure of the lesion. (3) Debridement of the lesion The paravertebral soft tissues and mediastinal pleura are bluntly dissected along the lateral side of the spine toward the anterior aspect of the vertebral body using a periosteal elevator or fingers to expose the lesion (Fig. 5②③). After aspirating the pus, caseous material, sequestra, and granulation tissue are curetted under direct vision. The extent of the lesion above, below, and the abscess cavity anterior to the vertebra is carefully examined. When removing the necrotic intervertebral disc between the two affected vertebrae with a nucleus pulposus forceps, sequestra of varying sizes are often extracted from the adjacent affected vertebrae. At the site of the vertebral bone defect, all subcutaneous node material is aspirated and curetted by accessing the contralateral paravertebral space. Alternatively, the anterior longitudinal ligament and periosteum are longitudinally incised at the anterolateral aspect of the affected vertebra, followed by subperiosteal dissection to reach as far as the contralateral side of the vertebra. During this process, gauze packing is used to expand the paravertebral abscess cavity while debriding the lesion. At the posterior aspect of the affected vertebra, near the bone defect anterior to the spinal canal, caution must be taken during curettage to avoid injuring the spinal cord and mistaking the intervertebral foramen for the lesion. During the debridement, adequate lighting is essential. Bone wax or gelatin sponge is used to control active bleeding points to maintain a clear surgical field and prevent accidental injury to the spinal cord. After thorough debridement, the area is irrigated. If the paravertebral abscess cavity is large or there is significant intraoperative bleeding, a silicone drainage tube may be placed in the abscess cavity upon completion of the procedure. (4) Suture The wound is closed in layers with No. 7 silk sutures. Postoperative management: The patient is placed supine on a hard bed and turned regularly to prevent bedsore. If debridement on the contralateral side of the vertebra is incomplete, a second debridement is performed 4–6 weeks after the first surgery. When the debridement is thorough, intervertebral bone grafting using rib or iliac bone can be performed to prevent kyphotic deformity and promote bony fusion of the vertebrae. 5. Thoracic vertebral subcutaneous node debridement via extrapleural approach within the thorax This approach provides satisfactory exposure of the lesion without entering the pleural cavity, avoiding respiratory dysfunction and complications associated with thoracotomy. It is suitable for subcutaneous nodes in the upper, middle, and lower thoracic vertebrae. Only one rib is resected during the procedure, minimizing the impact on spinal stability. Anesthesia: General anesthesia with endotracheal intubation. Position: The patient is placed in the lateral decubitus position, with the surgical side and trunk fixation as described previously. Procedure: (1) Incision Taking thoracic vertebrae 4–5 as an example, the incision starts between the medial border of the scapula and the spinous process at the level of the second rib, curves slightly, passes about 2–3 cm below the inferior angle of the scapula, and ends at the anterior axillary line on the lateral chest wall. The incision can be adjusted upward or downward depending on the level of the thoracic vertebral lesion (Fig. 6①). (2) Exposure of the lesion After incising the deep fascia, the auscultatory triangle is identified, with the latissimus dorsi muscle anteriorly and inferiorly, and the trapezius and rhomboid major muscles posteriorly and superiorly. The fascia of the auscultatory triangle is incised, and the index and middle fingers of the left hand are inserted into the incision to bluntly dissect the loose tissue between the deep surface of the muscles and the chest wall. The trapezius and rhomboid major muscles are divided toward the posterior and superior aspects of the triangular area, and the muscles are retracted laterally to expose the ribs. The right hand is inserted into the subscapular space, and the ribs are counted downward from the second rib to determine the rib to be resected based on the level of the lesion. The periosteum of the rib is incised and subperiosteal dissection is performed. A segment of the rib is resected, extending from the rib angle posteriorly to the midaxillary line anteriorly. After rib resection, a careful incision is made along the rib bed (taking care not to puncture the pleura) (Fig. 6②③④⑤). Fig. 6 Extrapleural debridement within the thorax Blunt dissection is performed in the extrapleural fat layer to separate the parietal pleura from the inner chest wall. The extent of pleural dissection should include at least three ribs above and below the incision and extend medially to the midline of the spine. If the paravertebral abscess is large, the dissection should be expanded further. In children and emaciated patients, the extrapleural fat is scant and the parietal pleura is thin and prone to tearing. If torn, it should be sutured immediately. Conversely, in patients with a history of pleuritis, the thickened pleura is less likely to tear. A retractor is used to spread the chest wall and expose the abscess, which is then punctured for localization. Protect the surrounding area of the abscess with saline gauze, make a longitudinal incision in the abscess wall. The steps and methods for lesion management are the same as those for transthoracic lesion removal and will not be repeated here. Irrigate the lesion, suture the abscess wall, and place a Bülau drainage tube to facilitate lung expansion and prevent pleural effusion and infection in the extrapleural space. Close the chest wall incision in layers.
6. Thoracic Vertebrae
11
~Lumbar Vertebrae
2
Subcutaneous Node Lesion Debridement
Anesthesia: General anesthesia with intubation.
Position: The patient is placed in a lateral position, with the thoracoabdominal plane at a 60° angle to the operating table. Sandbags are used to stabilize both sides of the torso. The upper limb on the operative side is flexed at the elbow and suspended on a horizontal head frame. The lower limb on the non-operative side is extended, while the upper limb and knee joint are semi-flexed. A soft pillow is placed between the two upper limbs. A soft pillow is also placed under the waist on the healthy side to fully separate the hypochondrium on the affected side from the iliac crest, facilitating exposure of the lesion during surgery.
Operative Steps:
⑴ Incision: Starting 3–4 cm lateral to the spinous process of the 10th thoracic vertebra, extend the incision to the transverse process of the 12th rib, then curve laterally along the 12th rib to its free end, ending 3–4 cm medial and superior to the anterior superior iliac spine (Figure 7).
Figure 7: Position and Incision for Thoracic Vertebrae
11
~Lumbar Vertebrae
2
Subcutaneous Node Lesion Debridement
⑵ Exposure of the Lesion: Incise the skin, subcutaneous tissue, and fascia, and appropriately mobilize the skin flaps bilaterally while protecting them. Make a longitudinal incision along the spine through the lower trapezius and upper latissimus dorsi muscles, then incise the latissimus dorsi and serratus posterior inferior muscles along the inferior border of the 12th rib. Retract these muscles bilaterally to expose the lateral portion of the sacrospinalis muscle, dissect it, and transect the serratus posterior inferior muscle to expose the 12th rib. Strip the periosteum from the rib, first transecting the 12th rib at the level of the transverse process, then completely resect it. If necessary, a segment of the 11th rib may also be resected. Take care to avoid injuring the 12th intercostal nerve, iliohypogastric nerve, and ilioinguinal nerve.
After incising the external oblique, internal oblique, and transversus abdominis muscles between the distal end of the 12th rib and the iliac crest, retract the muscle flaps anteriorly and posteriorly to expose the retroperitoneal fat and peritoneum. Use a gauze ball to dissect between the posterior peritoneum and the anterior wall of the abscess, then push the peritoneum, abdominal contents, kidney, and ureter medially until reaching the L1–2 vertebral bodies. Next, partially incise the periosteum along the 12th rib bed and separate the rib bed, chest wall, and diaphragm from the pleura.
Take care to avoid tearing the pleura. If a tear occurs, suture it immediately. Before ligating the tear, instruct the anesthesiologist to inflate the lungs with positive pressure. If repair is impossible, place a closed thoracic drainage tube postoperatively.
Remove the heads and necks of the 11th and 12th ribs using the aforementioned method, then clear the thoracic subcutaneous node lesion extrapleurally, as described in the relevant chapters. Alternatively, after resecting the 10th rib at the upper end of the incision, incise the 10th rib bed to enter the thoracic cavity and expose T10–12 for lesion debridement—i.e., via the extrapleural and extraperitoneal approach.
⑶ Lesion Debridement: The method for lesion debridement is as described earlier. Notably, the first to fourth lumbar arteries arise as a common trunk from the dorsal side of the abdominal aorta, crossing anterior to the vertebral bodies. The first and second lumbar arteries are thicker and lie deep to the diaphragmatic crura. When incising the lateral aspect of the vertebral body to expose the lesion, avoid injuring these arteries; locate and ligate them beforehand.
If the contralateral vertebral body is severely damaged with a large psoas abscess, perform debridement on the contralateral side 4–6 weeks postoperatively, once the patient’s general condition has improved. If the contralateral side has only an abscess with mild bone destruction and the patient’s condition is stable, the patient may be repositioned supine for supplementary abscess debridement during the same session.
⑷ Closure: Irrigate the lesion, place anti-subcutaneous node medication in the lesion, and close the wound in layers.
Postoperative Management: As described previously.
7. Lumbar Vertebrae
3–5
Subcutaneous Node Lesion Debridement Anesthesia: General anesthesia with endotracheal intubation or continuous epidural anesthesia. Position: The patient is placed in a supine position with both legs restrained by straps. The center of the lumbar vertebral disease lesion is aligned with the kidney bridge. Elevate the kidney bridge to facilitate exposure of the lesion during debridement. Choose either the left or right surgical approach, focusing on the side with more severe bone destruction and a larger iliopsoas abscess. If the contralateral side has only a mild cold abscess, a simple abscess debridement can be performed during the same session or at an intermediate stage [second stage].
Operative Steps:
(1) Incision: Draw an oblique or curved line from the free end of the 11th rib downward, ending 5–7 cm above the pubic tubercle. Incise the skin and subcutaneous tissue, and appropriately dissect laterally to both sides.
Lumbar spine
3–4
For cases with bilateral iliopsoas abscesses, a subumbilical transverse abdominal incision along the skin lines can also be used, resulting in minimal scarring and better cosmetic outcomes.
The extent of superior and inferior flap dissection and release should match the transverse dimension; otherwise, exposure of the vertebral lesion may be compromised. The external oblique, internal oblique, and transversus abdominis muscles are incised along their fiber directions, with an incision length similar to that of a standard oblique incision. Separate the transversalis fascia and then dissect posteriorly toward the midline to reach the iliopsoas abscess and vertebral lesion. If the iliopsoas abscess wall is thin, its surface may appear pale or dotted with petechial hemorrhages.
(2) Exposure of the lesion: During this process, identify the ureter (which exhibits peristalsis from top to bottom) and its accompanying gonadal (or ovarian) vein, the abdominal aorta (left) or inferior vena cava (right), and the common iliac or external iliac arteries and veins to avoid injury (Figure 8).
Figure 8: Lumbar spine
3–5
Subcutaneous node lesion debridement, exposure and aspiration of the abscess, with the ureter located medially.
The iliopsoas abscess is confirmed by aspiration. To facilitate lesion exposure, the abscess incision should be made as close as possible to the vertebral lesion. The abscess wall is sharply and bluntly separated along its muscle fiber direction. When dissecting distally, avoid injuring the common iliac arteries and veins, especially thin-walled, non-pulsating veins. During abscess debridement, the posterior wall contains the iliohypogastric nerve, ilioinguinal nerve (not visible in this incision), lateral femoral cutaneous nerve, femoral nerve, and obturator nerve, which run obliquely outward and downward from the spine. Any firm, cord-like structure suspected to be a nerve trunk should be carefully protected.
Typically, first locate the sinus tract leading to the diseased vertebra within the abscess cavity and enlarge it for lesion debridement. Do not mistake the intervertebral foramen for a vertebral bone lesion. The intervertebral foramen contains the lumbar arteries and veins, the ascending lumbar vein, and the dorsal branch of the lumbar artery, which enters the spinal canal through the foramen. Mistakenly incising and enlarging this area as a lesion may lead to uncontrollable bleeding and potential nerve root injury.
If no sinus tract connects the psoas abscess cavity to the vertebral lesion, first determine the level of the diseased vertebra. For lumbar spine
3–4
lesions, measure the distance from the iliac crest upward on an anteroposterior X-ray to locate the vertebral level. The lesion is typically found on the anterolateral aspect of the vertebral body, between the abdominal aorta (or inferior vena cava) and the intervertebral foramen.
For accessing vertebral lesions, especially in cases with well-developed iliopsoas muscles that hinder exposure, the paravertebral soft tissues should be incised layer by layer, including the origin of the iliopsoas muscle and the anterior longitudinal ligament of the vertebra. While incising, identify the lumbar arteries and veins to avoid cutting them. Do not incise directly to the vertebral periosteum in one motion, as retracted vessels may retreat deep into the soft tissue, making it difficult to locate bleeding points. If this occurs, the most effective method is to tightly pack the bleeding site with gauze for 5–10 minutes before locating and ligating the vessel.
Perform subperiosteal dissection at the vertebral bone lesion and use an osteotome to enlarge the lesion’s opening for thorough debridement.
For severe destructive lesions at
L3–4–5
with kyphotic deformity, the narrow space between the hypochondrium and iliac crest makes lesion exposure difficult, increasing the risk of vascular or nerve root injury. Exercise caution. During the entire process of clearing the lumbar vertebral disease lesion, avoid compressing the inferior vena cava, as it may impede the reflux of the vertebral venous system and lead to increased bleeding at the lesion site. Whether to perform bone grafting in the lesion and place a drainage tube in the abscess cavity is not mandatory.
⑶ Suture the transversus abdominis, internal oblique, external oblique, subcutaneous tissue, and skin layer by layer with interrupted silk sutures.
Postoperative management: Same as the relevant chapters.
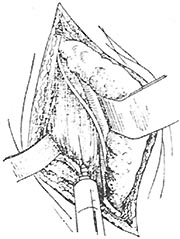
8. Transabdominal debridement for lumbar-sacral subcutaneous node.
⑴ Contraindications: Not suitable for patients with a history of acute abdomen or intestinal adhesions. If L5 is severely destroyed with little remaining structure and accompanied by kyphotic deformity, the bifurcation of the common iliac arteries and veins may be displaced downward, making it difficult to address the lesion via the presacral approach. In such cases, the extraperitoneal debridement route is preferable. This approach is also not recommended for patients with large abscesses in both iliopsoas muscles.
⑵ Preoperative preparation: Perform a cleansing enema one day before surgery and insert a bladder catheter on the day of the procedure.
Anesthesia: General or epidural anesthesia.
Position: The patient is placed supine in a slight Trendelenburg position.
⑶ Procedure:
1) Incision: A left paramedian lower abdominal incision is made, extending from the umbilical plane to the pubic symphysis. The peritoneum is incised along the direction of the incision, taking care to avoid injuring the bladder wall inferiorly.
2) Exposure of the lesion: The greater omentum and small intestine are retracted upward into the abdominal cavity and packed with saline-soaked gauze. The ascending or descending colon is retracted laterally to expose the presacral area, and a self-retaining retractor is used to maintain the position. The bladder (and uterus) is retracted downward. Identify the abdominal aorta and inferior vena cava, then lift the posterior peritoneum anterior to the midsacral region and incise it longitudinally. The two flaps of the posterior peritoneum are suspended and retracted laterally with fine silk sutures to avoid contaminating the abdominal cavity with pus during debridement. The common iliac arteries and veins, as well as the ureters and gonadal (ovarian) veins on both sides, should be clearly visualized and carefully protected. In Chinese individuals, the angle formed by the bifurcation of the left and right common iliac arteries at the L4~5 disc level ranges from 56° to 72°. If this angle is small and the bifurcation is low, presacral debridement becomes more challenging and requires special attention. The anterior lumbar-sacral region is bounded by the right common iliac artery on the right and the left common iliac vein on the left, forming a "safety triangle" where accessing the lesion is relatively safe.
3) Debridement of the lesion: In the midline of the presacral region, slightly偏向 the right common iliac artery, use a fine needle to aspirate and determine the midline incision line. Make a longitudinal, layered incision in an avascular area, taking care to avoid the median sacral vessels, especially the median sacral vein, which drains into the junction of the two common iliac veins and is prone to injury and difficult to control if bleeding occurs. Make a small incision to aspirate the presacral abscess, then enlarge the incision to include the anterior longitudinal ligament. Gently dissect laterally to avoid injuring the sacral nerve branches.
Debridement is primarily performed by suction and curettage, aiming for thorough removal, followed by irrigation. Intervertebral bone grafting is generally not强行 performed (Figure 9).
Figure 9: Intervertebral bone grafting and fusion during transabdominal debridement for lumbar-sacral subcutaneous node