| disease | Congenital Odontoid Process Deformity of the Cervical Spine |
Congenital odontoid dysplasia can lead to atlantoaxial instability and result in spinal cord injury, or even death.
bubble_chart Pathological Changes
Congenital odontoid anomalies include odontoid separation (Figure 1), odontoid hypoplasia, and odontoid aplasia. As shown in (Figure 2)

Figure 1 Odontoid Separation
A. Frontal view B. Posterior view C. Lateral view
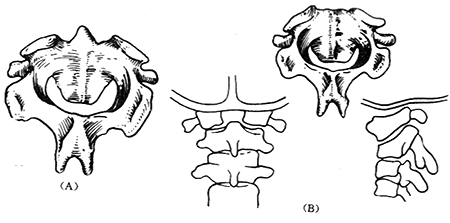
Figure 2
(A) Odontoid hypoplasia (B) Odontoid aplasia
The cause of congenital odontoid anomalies remains unclear. The odontoid is composed of two cartilaginous parts, and if chondrification fails to complete, odontoid anomalies occur. This type of anomaly leads to atlantoaxial joint instability, making it prone to dislocation and resulting in spinal cord compression symptoms.
bubble_chart Clinical Manifestations
The clinical manifestations of odontoid process separation, dysplasia, or absence are essentially the same. Clinically, there may be no symptoms, but when subjected to minor trauma, symptoms of medulla oblongata or upper cervical spinal cord compression may occur. The main symptoms include neck pain, torticollis, neck muscle tension, and restricted head and neck movement. In severe cases, quadriplegia may occur, leading to death. Lateral neck and open-mouth anteroposterior X-rays may show a short or absent odontoid process. In cases of odontoid process separation, the free bone is connected to the anterior arch of the atlas and has a large gap with the odontoid body. CT scans can clearly show the type of odontoid process deformity.
The diagnosis can be easily made based on clinical manifestations, lateral and open-mouth anteroposterior X-rays of the atlantoaxial joint. CT scans can accurately determine the type of deformity.
bubble_chart Treatment MeasuresMost scholars advocate for active surgery. For those incidentally discovered during physical examinations, close observation is necessary to avoid trauma, and a cervical collar can be used for immobilization. For patients with clinical symptoms, cervical immobilization with a collar can be attempted first. If symptoms do not improve, atlantoaxial fusion should be considered. For patients with cervical instability leading to neurological symptoms, occipitocervical posterior fusion can be performed. In recent years, some scholars have adopted posterior atlantoaxial lateral joint screw fixation, which also achieves atlantoaxial joint stabilization.
Key points of occipitocervical posterior fusion:
1. Incision: A longitudinal incision from the external occipital protuberance to the spinous process of cervical 5.
2. Exposure: The occipital bone and cervical laminae are exposed. The muscles and soft tissues attached to the spinous processes are stripped subperiosteally. The laminae of cervical 1-2 and the external occipital protuberance are exposed.
3. Bone grafting and fusion: Autologous iliac bone is harvested, with a length equal to the distance from the external occipital protuberance to the cervical spinous process and a width equal to the width of the cervical laminae. The harvested iliac bone is shaped into an "H" form, with the upper end curved and two small holes drilled at each end of the curve. The lower end of the bone block is notched to straddle the cervical spinous process. Two holes are drilled into the external occipital protuberance, penetrating only the outer table of the skull. The bone block is fixed to the occipital bone using 1.0mm diameter stainless steel wires, with the two "limbs" of the bone block embedded on the spinous process of cervical 2
. Small bone strips are then packed on both sides of the bone block.4. Postoperatively, the patient is placed on a gypsum bed that includes the head and neck until the bone graft has fused.
Children under the age of 2 should be distinguished due to the absence of the apical epiphyseal nucleus of the odontoid process; after the age of 12, the fusion of the apical epiphyseal nucleus of the odontoid process with the odontoid body can be easily misdiagnosed as odontoid deformity and should be differentiated.




