| disease | Breech Presentation |
| alias | Breech Presentation |
Breech presentation is the most common abnormal fetal position, accounting for approximately 3-4% of full-term pregnancies and deliveries. Because the fetal head is larger than the fetal breech and does not undergo significant molding during delivery when the head is delivered last, breech births are often difficult. Additionally, the incidence of umbilical cord prolapse is higher, leading to an increased perinatal mortality rate, which is 3-8 times higher than that of occiput presentation. In breech presentation, the sacrum serves as the reference point, resulting in six possible fetal positions: left sacrum anterior (LSA), left sacrum transverse (LST), left sacrum posterior (LSP), right sacrum anterior (RSA), right sacrum transverse (RST), and right sacrum posterior (RSP).
bubble_chart Etiology
Before 30 weeks of pregnancy, breech presentation is more common, and after 30 weeks of pregnancy, it usually converts naturally to cephalic presentation. The exact reasons for persistent breech presentation during labor are not entirely clear, but possible factors include:
1. Excessive fetal movement within the uterine cavity—polyhydramnios, lax abdominal walls in multiparous women, and relatively more amniotic fluid in premature labor, allowing the fetus to move freely and assume a breech position.
2. Restricted fetal movement within the uterine cavity—uterine abnormalities (such as unicornuate uterus, bicornuate uterus, etc.), fetal abnormalities (such as hydrocephalus, etc.), twins, and oligohydramnios, which increase the likelihood of breech presentation.
3. Obstruction to fetal head engagement—narrow pelvis, placenta previa, pelvic tumors, etc., which also predispose to breech presentation.
bubble_chart PathogenesisAmong the various parts of the fetus, the fetal head is the largest, the fetal shoulders are smaller than the head, and the fetal buttocks are the smallest. In cephalic presentation, once the fetal head is delivered, the other parts of the body follow. However, in breech presentation, the situation is different: the smaller and softer buttocks are delivered first, while the largest part, the fetal head, is delivered last. To adapt to the conditions of the birth canal, the fetal buttocks, shoulders, and head must follow a specific mechanism to accommodate the birth canal for successful delivery. Therefore, it is essential to understand the childbirth mechanism of these three parts: the fetal buttocks, shoulders, and head. Using the right sacroanterior position as an example, the mechanism is explained below (Figure 4).
|
|
|
(1) The intertrochanteric diameter of the fetal buttocks engages with the right oblique diameter of the pelvic inlet. | (2) After internal rotation, the intertrochanteric diameter aligns with the anteroposterior diameter of the maternal pelvic outlet. |
|
|
|
(3) The anterior hip is delivered under the pubic arch, and the buttocks are delivered with the intertrochanteric diameter aligned with the anteroposterior diameter of the pelvis. | (4) After the delivery of the fetal buttocks, they rotate clockwise, turning the buttocks anteriorly. |
|
|
|
(5) The sagittal suture of the fetal head engages with the left oblique diameter of the pelvic inlet. | (6) After the fetal head enters the pelvis, the sagittal suture descends along the left oblique diameter of the pelvis. |
|
|
|
(7) When the occipital bone undergoes internal rotation and reaches below the pubic symphysis, the sagittal suture aligns with the anteroposterior diameter of the pelvic outlet. | (8) As the occipital bone curves downward under the pubic arch, the fetal head flexes and is delivered, with the sagittal suture still aligned with the anteroposterior diameter of the pelvic outlet. |
Figure 4. Mechanism of childbirth in right sacroanterior position.
1. After the breech is delivered, the fetal buttocks engage with the pelvic inlet along the right oblique diameter via the intertrochanteric diameter [Figure 4 (1)], with the sacrum located at the right anterior position. The fetal buttocks gradually descend, with the anterior hip descending slightly faster and thus positioned lower. Upon encountering resistance at the pelvic floor, the anterior hip internally rotates 45° toward the mother's right side, positioning it behind the pubic symphysis. At this point, the intertrochanteric diameter aligns with the anteroposterior diameter of the mother's pelvic outlet [Figure 4 (2)]. The fetal buttocks continue to descend, and the fetal body flexes laterally to adapt to the curvature of the birth canal. The posterior hip is delivered first from the anterior edge of the perineum, followed by slight extension of the fetal body, allowing the anterior hip to be delivered from beneath the pubic arch [Figure 4 (3)]. Subsequently, both legs and feet are delivered. After the fetal buttocks and lower limbs are delivered, the fetal body undergoes external rotation, turning the fetal back to the anterior or right anterior position [Figure 4 (4)].
2. Delivery of the Shoulders As the fetus undergoes external rotation, the biparietal diameter of the fetal shoulders engages with the right oblique or transverse diameter of the pelvic inlet and gradually descends along this axis. When the shoulders reach the pelvic floor, the anterior shoulder rotates 45° to the right, moving under the pubic arch, aligning the biparietal diameter with the anteroposterior diameter of the pelvic outlet. Simultaneously, lateral flexion of the fetal body allows the posterior shoulder and posterior upper limb to be delivered past the anterior perineal margin, followed by the anterior shoulder and anterior upper limb emerging from beneath the pubic arch.
3. Delivery of the Head When the shoulders pass through the perineum, the sagittal suture of the fetal head engages with the left oblique or transverse diameter of the pelvic inlet [Figure 4 (5)] and gradually descends along this axis [Figure 4 (6)], while the head undergoes flexion. When the occipital bone reaches the pelvic floor, the fetal head rotates 45° toward the mother's left anterior, positioning the occipital bone toward the pubic symphysis [Figure 4 (7)]. As the head continues to descend, the occipital bone's lower concavity reaches the inferior margin of the pubic arch, serving as a pivot point. The head further flexes, allowing the chin, face, and forehead to emerge sequentially past the anterior perineal margin, followed by the occiput being delivered from beneath the pubic arch [Figure 4 (8)].bubble_chart Clinical Manifestations
According to the posture of the lower limbs, it is divided into:
1. Single breech presentation or frank breech presentation: The fetus has both hip joints flexed and both knee joints extended, with the buttocks as the presenting part. This is the most common type.
2. Complete breech presentation or mixed breech presentation: The fetus has both hip and knee joints flexed, resembling a cross-legged sitting position, with the buttocks and both feet as the presenting parts. This is relatively common.
3. Incomplete breech presentation: One or both feet, one or both knees, or one foot and one knee serve as the presenting parts. Knee presentation is temporary and usually converts to foot presentation after labor begins. This is less common.
Pregnant women often feel a round, hard fetal head below the ribs. Because the fetal buttocks cannot fit snugly against the lower uterine segment and cervix, uterine contractions are often weak, cervical dilation is slow, and labor is prolonged.
Impact on the mother: The irregular shape of the fetal buttocks prevents them from fitting snugly against the lower uterine segment and cervix, increasing the risk of premature rupture of membranes or secondary uterine inertia, which raises the chances of puerperal infection and postpartum hemorrhage. If forceful traction is applied before full cervical dilation, it may cause cervical lacerations or even extend to the lower uterine segment.
Impact on the fetus: The uneven surface of the fetal buttocks exerts uneven pressure on the forebag of membranes, often leading to premature rupture of membranes and increased risk of umbilical cord prolapse. Compression of the umbilical cord can cause fetal distress or even death. Difficulty in delivering the aftercoming head may result in neonatal asphyxia, brachial plexus injury, and intracranial hemorrhage.
1. Clinical manifestations Pregnant women often feel a round and hard fetal head under the ribs. Because the fetal breech cannot closely adhere to the lower segment of the uterus and the cervix, it often leads to uterine contractions lacking strength, slow cervical dilation, resulting in prolonged labor.
2. Abdominal examination The uterus is longitudinally oval, and the longitudinal axis of the fetus aligns with the maternal longitudinal axis. A round, hard fetal head, sometimes with a floating sensation when pressed, can be palpated at the fundus; above the pubic symphysis, an irregular, soft, and wide fetal breech can be felt, and the fetal heart sounds are most clearly heard on the left (or right) upper side.
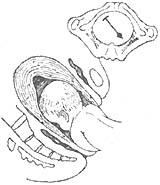
3. Rectal and vaginal examination During a rectal exam, the soft and irregular fetal breech or fetal feet/knees may be palpated. If the fetal breech is positioned high and cannot be confirmed by rectal exam, a vaginal examination is required. During a vaginal exam, assess the degree of cervical dilation and check for umbilical cord prolapse. If the fetal membranes have ruptured, the fetal breech, external genitalia, and anus can be directly touched. At this time, it should be differentiated from the fetal face. For the breech, the anus and the two ischial tuberosities lie in a straight line, and inserting a finger into the anus may feel the annular sphincter contraction; upon withdrawal, meconium may be seen. For the face, the mouth and the two zygomatic prominences form a triangle, and inserting a finger into the mouth may touch the gums and the arched mandible. If fetal feet are felt, they should be distinguished from fetal hands (Figure 1).

Figure 1 Differences between fetal hands and feet
4. B-ultrasound examination Can accurately determine the type of breech presentation, fetal size, fetal head posture, etc.
bubble_chart Treatment Measures
1. During pregnancy: Before 30 weeks of pregnancy, breech presentations often spontaneously convert to cephalic presentations. If a breech presentation persists after 30 weeks of pregnancy, correction should be attempted. Common correction methods include:
(1) Knee-chest position: Have the pregnant woman empty her bladder and loosen her waistband. The knee-chest position is shown in Figure 2. Perform this twice daily for 15 minutes each time, and recheck after one week. This posture helps the fetal buttocks exit the pelvis, allowing the fetal head and back to slide along the uterine curvature due to changes in the fetus's center of gravity.
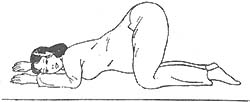
Figure 2 Knee-chest position
(2) Laser irradiation or moxibustion at the Zhiyin point: In recent years, laser irradiation of the bilateral Zhiyin points (located on the outer side of the little toe, approximately 1 fen from the toenail corner) has been commonly used. Alternatively, moxibustion with moxa sticks can be applied once daily for 15–20 minutes, with five sessions constituting one course of treatment.
(3) External cephalic version (ECV): If the above correction methods are ineffective, ECV may be performed between 32–34 weeks of pregnancy. Due to the risk of severe complications such as placental abruption or cord entanglement, caution is required. Administer 4.8 mg of salbutamol orally half an hour before the procedure. ECV is best performed under B-ultrasound monitoring. The pregnant woman lies flat with her abdomen exposed. Confirm the fetal position and monitor the fetal heart rate. Steps include loosening the presenting part (lifting it gently upward with both hands to free it) and rotating the fetus (holding the fetus at both ends, gently pushing the head toward the pelvic inlet along the fetal abdomen while lifting the buttocks upward until cephalic presentation is achieved). Movements should be gentle and intermittent. If frequent or intense fetal movements or abnormal fetal heart rate are observed during or after the procedure, stop rotating, return to the original position, and monitor for half an hour.
2. During childbirth: Based on factors such as maternal age, parity, pelvic size, fetal size, fetal viability, type of breech presentation, and complications, the appropriate mode of delivery should be determined during the initial stage of labor.
(1) Indications for elective cesarean section: Narrow pelvis, abnormal soft birth canal, fetal weight >3500 g, fetal distress, elderly primipara, history of difficult delivery, incomplete breech presentation, etc., all warrant cesarean delivery.
(2) Management of vaginal delivery:
1) First stage of labor: The woman should lie on her side and avoid standing or walking. Minimize rectal exams and avoid enemas to prevent premature rupture of membranes. If membranes rupture, immediately check the fetal heart rate. If the heart rate slows or accelerates, perform a rectal exam or, if necessary, a vaginal exam to check for cord prolapse. If cord prolapse occurs with a stable fetal heart rate but incomplete cervical dilation, an emergency cesarean section is required to save the fetus. If no cord prolapse is present, closely monitor the fetal heart rate and labor progress. If coordinated uterine contractions are weak, efforts should be made to strengthen them. When the cervix is dilated to 4–5 cm, the fetal foot may protrude into the vagina. To ensure full dilation of the cervix and vagina, after disinfecting the perineum, use the "blocking" method: during contractions, cover the vaginal opening with a sterile towel using the palm to prevent the fetal foot from descending first, allowing the buttocks to descend only after full dilation. This facilitates smooth delivery of the aftercoming head (Figure 3). During "blocking," monitor the fetal heart rate every 10–15 minutes and check for full cervical dilation. Prolonged blocking after full dilation may cause fetal distress or uterine rupture. As full dilation approaches, prepare for delivery and neonatal resuscitation.

Figure 3 Blocking the perineum with the palm to promote fetal squatting
2) Second stage of labor: Before delivery, the bladder should be emptied by catheterization. Primiparas should undergo an episiotomy. There are three methods of childbirth: ① Spontaneous childbirth: The fetus is delivered naturally without any traction. This is very rare and only occurs in multiparous women with a small fetus, strong uterine contractions, and a normal birth canal. ② Assisted breech delivery: After the fetal breech is delivered naturally up to the umbilical region, the shoulders and aftercoming head are assisted by the birth attendant. After the umbilical region is delivered, the head should generally be delivered within 2-3 minutes, with a maximum of no more than 8 minutes. For the delivery of the aftercoming head, some advocate the use of single-blade forceps for better results. ③ Breech extraction: The entire fetus is delivered by traction from the birth attendant. This procedure carries a high risk of fetal injury and should not be used.
3) The third stage of labor: Prolonged labor is prone to complications such as uterine atony and bleeding. After the placenta is delivered, oxytocin should be injected intramuscularly to prevent postpartum hemorrhage. For surgical procedures and soft birth canal injuries, timely suturing should be performed, and antibiotics should be administered to prevent infection.