| disease | Adenovirus Pneumonia |
Since 1958, various regions in China have confirmed that adenoviruses not only cause upper respiratory tract infections but can also lead to infantile pneumonia, most commonly affecting children aged 6 months to 2 years. Adenovirus pneumonia is the most severe, particularly prevalent in northern provinces, with more severe cases compared to southern regions. Large-scale outbreaks of extremely severe adenovirus pneumonia occurred in North China, Northeast China, and Northwest China during the winters of 1958 and 1963.
bubble_chart Epidemiology
Adenoviruses are generally transmitted through respiratory epidemics. In collective childcare settings, adenoviral upper respiratory infections and pneumonia often occur simultaneously. Serological studies in populations indicate that specific adenovirus antibodies passed from the mother are commonly retained during the first few months after birth, followed by a lack of antibodies until the age of two, after which they gradually increase. This observation aligns perfectly with the clinical finding that 80% of adenoviral pneumonia cases occur in infants aged 7 to 24 months. Notably, the larger the number of susceptible individuals across different age groups in a region, the higher the incidence of adenoviral respiratory infections, and the greater the likelihood of adenoviral pneumonia in infants and young children. In northern China, adenoviral pneumonia is more prevalent in winter and spring, with only occasional cases in summer and autumn, while in Guangzhou, during high-prevalence years, it is more commonly seen in autumn. In Beijing, this type of pneumonia accounts for approximately 20–30% of viral pneumonia cases.
bubble_chart EtiologyIt is known that there are 41 serotypes of adenovirus, many of which are closely associated with upper and lower respiratory tract infections in humans. Pathological observations from hospitalized children in both northern and southern regions of China have confirmed that adenovirus types 3 and 7 are the primary pathogens causing adenoviral pneumonia. The virus can be isolated from throat swabs, feces, or postmortem lung tissue, with serum antibody titers during the convalescent stage increasing fourfold or more compared to the early stage (5–10 days after onset or earlier). Similar pathological findings have been observed in severe cases of measles complicated by pneumonia. In Beijing and other areas, adenovirus type 11 has also been identified as a common pathogen for pneumonia and upper respiratory tract infections (Pediatric Research Institute, 1964–1966). Additionally, types 21, 14, as well as 1, 2, 5, and 6 have gradually emerged in mainland China, while types 1, 2, 5, and 6 are predominant in Taiwan. Recently, Bethune Medical University conducted genomic analysis of adenovirus types 3 and 7 isolated between 1976 and 1988, confirming that type 7b often leads to severe pneumonia.
Adenovirus is a DNA virus that primarily replicates within the cell nucleus. It exhibits strong resistance to heat, acid, and lipid solvents. Besides the throat, conjunctiva, and lymphoid tissues, it also replicates in the intestines. Based on their ability to agglutinate specific animal red blood cells, adenoviruses can be divided into three groups. The group that frequently causes pneumonia in infants and young children—types 3, 7, 11, 14, and 21—can all agglutinate monkey red blood cells.
bubble_chart Pathological ChangesFocal or confluent necrotic pulmonary infiltration and bronchitis are the main pathological changes of this disease. The consolidated pneumonia can occupy an entire lobe, most commonly the lower lobe of the left lung. On the cut surface of the lung, tubular structures composed of yellowish-white necrotic material can be squeezed out from the consolidated areas, and the lung tissue outside the consolidation often shows significant emphysema. Microscopically, the lesions are centered around bronchitis and peribronchitis, with inflammation often progressing to necrosis. The exudate fills the entire lumen, and the alveolar spaces around the bronchi also frequently contain exudate, mostly consisting of lymphocytes, monocytes, serous fluid, and fibrin, sometimes accompanied by hemorrhage, with very few neutrophils. Necrosis of the alveolar walls is also common. At the edges of the inflammatory areas, hyperplasia of bronchial or alveolar epithelium can be seen. Within the nuclei of the hyperplastic and enlarged epithelial cells, intranuclear inclusion bodies are often visible, approximately the size of normal red blood cells, with clear boundaries and staining that is eosinophilic or amphophilic, surrounded by a clear halo. The nuclear membrane is distinct, with a small amount of chromatin accumulation on the inner surface of the nuclear membrane. However, there are no cytoplasmic inclusion bodies or multinucleated giant cells, allowing morphological differentiation from measles virus pneumonia and pulmonary cytomegalic inclusion disease. Additionally, systemic organs such as the central nervous system and heart exhibit interstitial inflammation and hyperplasia of small vascular wall cells.
bubble_chart Clinical ManifestationsAccording to the analysis of 245 cases of adenovirus pneumonia in infants and young children caused by types 3 and 7, confirmed virologically in Beijing from 1959 to 1963, the clinical characteristics can be summarized as follows.
1. Symptoms
(1) Onset: The incubation period is 3 to 8 days. Generally, there is a sudden fever, often reaching a high temperature above 39°C from the first or second day, and by the third or fourth day, it mostly presents as a sustained or irregular high fever; in more than 3/5 of the cases, the highest body temperature exceeds 40°C.
(2) Respiratory symptoms: Most children develop a cough from the onset, often manifesting as frequent coughing or grade I paroxysmal coughing, accompanied by pharyngeal congestion, but nasal catarrhal symptoms are less noticeable. Dyspnea and cyanosis mostly begin between the third and sixth days, gradually worsening; severe cases exhibit nasal flaring, three depressions sign, wheezing and breathlessness (obstructive dyspnea with wheezing and breath-holding), and cyanosis of the lips and nails. Dullness is easily detected on percussion; areas of dullness are accompanied by diminished breath sounds, and sometimes tubular breath sounds can be heard. In the initial stage, auscultation mostly reveals coarse breath sounds or dry rales, with moist rales appearing after the third or fourth day of illness, increasing gradually, and often accompanied by signs of lung qi swelling. Severe cases may show pleural reaction or pleural effusion (mostly seen in the second week). In the absence of secondary infection, the effusion is straw-yellow and clear; with secondary infection, it becomes turbid, with white blood cell counts often exceeding 10×109/L.
(3) Neurological symptoms: Generally, drowsiness and lethargy appear after the third or fourth day of illness, sometimes alternating with dysphoria. In severe cases, semi-unconsciousness and convulsions may occur in the advanced stage. Some children exhibit head tilting backward and neck stiffness. Apart from toxic encephalopathy, some cases involve encephalitis caused by adenovirus, necessitating lumbar puncture for differentiation.
(4) Circulatory symptoms: Pale complexion is relatively common, with a grayish complexion in severe cases. Heart rate increases, generally not exceeding 160 beats per minute in mild cases, while severe cases often range between 160 and 180 beats, sometimes exceeding 200 beats. Electrocardiograms typically show sinus tachycardia, with severe cases exhibiting right heart load increase, changes in T waves and ST segments, and low voltage. Occasionally, first- or second-degree atrioventricular block or pulmonary P waves may appear. In 35.8% of severe cases, heart failure occurs between the sixth and fourteenth days of illness. The liver gradually enlarges, reaching 3–6 cm below the costal margin, with a firm texture; a few cases also show splenomegaly.
(5) Digestive symptoms: More than half of the cases experience grade I diarrhea and vomiting, with severe cases often showing abdominal distension and fullness. Diarrhea may be related to adenovirus replication in the intestines, but in some cases, it may also result from severe illness and high fever affecting digestive function.
(6) Other symptoms: Catarrhal conjunctivitis, red papules, maculopapular rashes, and scarlatiniform rashes may occur. Although the appearance of small chalky white spots on the tonsils is not common, it is a relatively specific early sign of this disease.
2. X-ray findings
X-ray morphology is closely related to the severity and stage of the disease. Thickened and blurred lung markings are early manifestations of adenovirus pneumonia. Pulmonary consolidation usually begins to appear between the third and fifth days of illness, with patchy lesions of varying sizes or confluent sexually transmitted disease lesions, most commonly seen in the lower lobes of both lungs and the upper right lung. Between the sixth and eleventh days of illness, the density of the lesions increases with disease progression, and the lesions become more numerous, widely distributed, and confluent. Unlike lobar pneumonia, the lesions in this disease are not confined to a single lobe. Most lesions begin to resolve after the eighth to fourteenth days. If the lesions continue to increase and the condition worsens, mixed infection should be suspected. Lung qi swelling is quite common, with no significant difference between the early and peak stages, presenting as bilateral diffuse lung qi swelling or perilesional lung qi swelling (Figure 1). Pleural changes occur in 1/6 of cases, mostly presenting as pleural reaction or effusion during the peak stage.
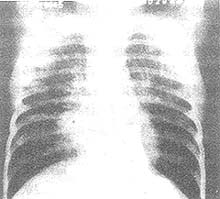
Figure 1 Adenovirus pneumonia, lung qi swelling
3 years old, female. Persistent high fever, cough, and wheezing for 8 days, with type VII adenovirus isolated from throat swab. Chest X-ray shows increased density of the right hilum, thickened and coarse lung markings in the inner zones of both lungs, patchy shadows in the inner zone of the right lung, significantly increased translucency in the lower zones of both lungs, diaphragms located at the level of the 10th posterior rib with flattened diaphragmatic curvature, consistent with grade III lung qi swelling.
3. Disease Course
This condition is classified into mild and severe cases based on respiratory and toxic symptoms. The fever pattern varies, with most cases showing a persistent high fever of 39–40°C or above, followed by irregular fever, while remittent fever is less common. In mild cases, the temperature usually drops abruptly within 7–11 days, and other symptoms disappear relatively quickly, but lung shadows take 2–6 weeks to fully resolve. Severe cases often exhibit marked drowsiness, a pale or grayish complexion, significant hepatomegaly, obvious dyspnea, and large areas of lung consolidation after the 5th–6th day of illness. Some cases may develop heart failure, convulsions, or semi-unconsciousness. In recovering patients, fever subsides between the 10th–15th day, with abrupt and gradual defervescence each accounting for half of the cases. Occasionally, a fever rebound may occur after abrupt defervescence, returning to normal after 1–2 days. The convalescence stage of lung lesions is even longer, lasting 1–4 months. Cases where shadows persist beyond 3–4 months often develop atelectasis, which may later progress to bronchiectasis. We followed up cases of type 3 and 7 adenovirus pneumonia for 1–5 years, finding 30.1% with chronic pneumonia, atelectasis, or occasional bronchiectasis. Later, a 10-year follow-up of 109 cases of type 3, 7, and 11 adenovirus pneumonia revealed that 45.3% showed interstitial thickening, fibrosis, or chronic bronchitis on X-ray; 3.8% had chronic pneumonia with bronchiectasis; and 4.7% each had bronchiectasis or chronic pneumonia alone.
Adenovirus pneumonia in preschool and school-aged children is generally mild, often presenting with persistent high fever but without severe respiratory or neurological symptoms. When measles is complicated or followed by adenovirus pneumonia, all symptoms become more severe, and the condition is prone to sudden deterioration.
We observed 34 cases (1964–1980) of type 11 adenovirus pneumonia and found no significant difference in clinical manifestations compared to types 3 and 7. However, the incidence of severe cases and deaths was similar to type 3 and significantly lower than type 7.
Clinical features of adenovirus pneumonia in infants aged 1–5 months: We observed 38 cases (20 type 3, 12 type 7, 6 type 11, 1981–1983), including 8 cases of bronchiolitis and 30 cases of pneumonia. Most presented with low-grade or grade II fever, a short febrile course, and no signs of lung consolidation. Chest X-rays mainly showed small shadows. Lethargy, drowsiness, and other neurological symptoms were less frequent and milder compared to infants over 6 months old. Clinically, these cases were indistinguishable from respiratory syncytial virus or parainfluenza virus pneumonia, resulting in none being diagnosed as adenovirus pneumonia before etiological confirmation.
bubble_chart Auxiliary Examination
The total white blood cell count is mostly decreased or normal in the early stage (days 1-5), with approximately 62% of cases below 10×109/L (10,000/mm3), and 36% between (10-15)×109/L (10,000-15,000/mm3). No significant changes are observed in the differential count. In the advanced stage, the white blood cell count is similar to that in the early stages, and only increases when secondary bacterial infection occurs. Blood smear examination reveals that the alkaline phosphatase and nitroblue tetrazolium staining of neutrophils are generally lower than in normal children or those with bacterial pneumonia. Even when the total white blood cell count reaches 15,000, the leukocyte alkaline phosphatase index remains significantly reduced. Some children may test positive for serum cold agglutinins. During the fever period, a small amount of protein may be detected in the urine of some cases. Among children exhibiting meningeal irritation symptoms, cerebrospinal fluid examination is generally normal.
The diagnosis should be based on the epidemic situation and clinical manifestations. The early-stage differences between typical adenovirus pneumonia in infants and young children and general bacterial pneumonia are as follows: ① Most cases present with persistent high fever at the onset or shortly after, which is ineffective with antibiotic treatment; ② From the 3rd to 6th day of illness, neurological symptoms such as drowsiness and lethargy appear, with drowsiness sometimes alternating with dysphoria. The complexion appears pale or grayish, hepatomegaly is significant, and complications such as heart failure and convulsions are prone to occur later. These symptoms suggest that adenovirus pneumonia not only affects the respiratory tract but also involves other systems; ③ Pulmonary signs appear relatively late, generally after the 3rd to 5th day of illness, with moist rales appearing gradually. The affected area expands progressively, often accompanied by dullness on percussion and diminished breath sounds. Dyspnea worsens during the second week of illness; ④ The total white blood cell count is relatively low, with the majority of cases not exceeding 12×109/L (12,000/mm3), and neutrophils not exceeding 70%. The alkaline phosphatase and nitroblue tetrazolium staining values of neutrophils are significantly lower than those in purulent bacterial infections, but they rise again if a concurrent purulent bacterial infection occurs; ⑤ Chest X-rays may show large patchy shadows, most commonly in the left lower lobe. In summary, during the epidemic season, a preliminary diagnosis can be made if infants and young children develop severe pneumonia with clinical, X-ray, and blood test findings consistent with the above. Facilities with the necessary resources may perform rapid viral diagnostics. Currently, immunofluorescence techniques (indirect methods are more suitable than direct methods), enzyme-linked immunosorbent assays (ELISA), and specific IgM testing can be performed. However, these three methods cannot differentiate adenovirus serotypes, which is a limitation. Conventional throat swab virus isolation and paired serum antibody tests are only suitable for retrospective diagnosis in laboratory settings.
bubble_chart Treatment Measures
General treatment refers to the section on bronchopneumonia treatment. Below, we focus on insights gained from recent clinical practice. 1. **Antiviral drugs** still require extensive research. Ribavirin used to treat adenovirus pneumonia showed no significant effect when administered via nasal drops. However, intravenous and/or intramuscular injection in early-stage cases yielded better results compared to the control group, while advanced-stage cases showed no significant improvement (Beijing Children's Hospital and Institute of Materia Medica, Chinese Academy of Medical Sciences, 1978–1980). Further studies on aerosol inhalation therapy are needed. 2. **Prevention and treatment of secondary bacterial infections** should be emphasized. If a secondary infection is suspected, prompt treatment is necessary. For example, Staphylococcus aureus infections may be treated with new-generation penicillins or cephalosporins, while Escherichia coli infections may require ampicillin. 3. **Sedation, antispasmodics, and asthma relief** can be achieved with drugs like chlorpromazine and promethazine. 4. **Digitalis preparations** may be used to control heart failure. 5. **Blood transfusion, plasma infusion, or gamma globulin administration** may provide supportive effects. 6. **Proper oxygen therapy and fluid infusion**, if managed appropriately, can help critically ill children through the peak phase. 7. **Adrenocorticosteroids** were tested in early-stage patients without significant efficacy. However, in cases of severe respiratory obstruction or critical toxic symptoms (convulsions, unconsciousness, shock, persistent high fever above 40.6°C, etc.), short-term intravenous corticosteroid therapy may be warranted. 8. **Specific horse serum therapy**. From 1961 to 1964, the clinical efficacy of horse serum against adenovirus types 3 and 7 was observed, with mixed conclusions. After 1973, the serum production process was improved, increasing its potency. Applied in provinces like Jilin and Heilongjiang, it reportedly reduced fever rapidly, alleviated symptoms early, and minimized sequelae, achieving favorable results (Department of Pediatrics, Bethune Medical University, and Changchun Institute of Biological Products, among others). However, post-1976 batches were more likely to cause serum sickness. 9. **During the convalescent stage**, if lung signs persist, physiotherapy is recommended.
Chinese medicine therapy for adenovirus pneumonia primarily focuses on ventilating the lung, clearing heat, and removing toxins in the early stage. In the intermediate stage [second stage], clearing up phlegm is added, while in severe cases or the critical phase, supporting healthy qi and rescuing from collapse is emphasized. According to the experience of Dr. Pu Fu-zhou from the Chinese Medicine Research Institute, pneumonia is an externally contracted disease, not limited to the scope of warm diseases, and includes categories such as wind-cold, summerheat, and dampness. The focus of pneumonia always lies in the lung, and severe cases may affect other zang-fu organs. Treatment is divided into routine therapy and rescue methods. The principle is to ventilate the lung and expel pathogens when evil is excessive, while for deficiency of healthy qi and collapse, methods such as nourishing yin, restoring yang, and replenishing both qi and fluids are used. Specifically, routine treatment focuses on ventilating the lung and expelling pathogens through the exterior, while rescue methods emphasize pattern identification. The approaches are summarized into eight methods and post-illness recuperation. (1) **Releasing exterior method**: For wind-heat invading the lung, use Mulberry Leaf and Chrysanthemum Decoction combined with Fistular Onion Stalk and Fermented Soybean Decoction with modifications. If heat is severe, combine with Modified Lonicera and Forsythia Powder. For wind-cold attacking the lung, use Apricot Kernel and Perilla Powder and Scallion and Fermented Soybean Decoction with modifications. For summerheat pathogens, use Chinese Mosla Drink with modifications. (2) **Therapy for releasing both the internal and external**: For exterior cold and interior heat, use Ephedra, Apricot Kernel, Gypsum, and Licorice Decoction with additions. For external cold and internal heat, Minor Green-Blue Dragon Plus Gypsum Decoction was used. If internal fluid retention is not severe, with phlegm in the throat and a croaking sound, a pale or slightly red tongue, and floating rapid pulse, treat with Belamcanda and Ephedra Decoction. For exterior collapse with interior cold, use Cinnamon Twig, Magnolia Bark, and Bitter Apricot Seed Decoction. For exterior collapse with interior heat, use Pueraria, Skullcap, and Coptis Decoction with additions. For exterior collapse with thoracic accumulation, use Minor Chest Bind Decoction combined with Trichosanthis Fruit and Longstamen Onion Bulb Decoction with modifications. (3) **Unblocking yang and draining dampness method**: For dampness pathogens, use Thousand Gold Phragmites Stem Decoction with additions. If dampness-heat blocks the lung, causing unconsciousness and miliaria alba, use Coix Seed and Bamboo Leaf Powder. (4) **Clearing heat and nourishing yin method**: For qi deficiency and heat blockage, use 3g of American ginseng to support healthy qi and administer 5g of Cow-Bezoar Powder divided into five doses. If healthy qi is deficient and pathogens enter the nutrient level, use heat-clearing and toxin-removing formulas with additions to unblock stagnation. For residual heat, use Bamboo Leaf and Gypsum Decoction with modifications. For summerheat damaging lung qi, follow Wang’s method of clearing summerheat and regulating qi with modifications. (5) **Descending qi and resolving phlegm method**: For qi counterflow with panting, use Perilla Fruit Qi-Descending Decoction with modifications. For liver qi ascending counterflow, use Inula and Hematite Decoction with additions. (6) **Supporting healthy qi and unblocking stagnation method**: For prolonged illness with deficient lung qi and severe pathogen blockage, use Polyghace Seche, Milkwort Root, rice, Chinese Date, and Chebula Fruit to tonify the lung and replenish qi. If lung blockage is severe, add a small amount of charred Ephedra and select Bitter Apricot Seed, raw Gypsum, Platycodon Root, and Fistular Onion Stalk to attack and supplement for unblocking. (7) **Consolidating yin and descending counterflow method**: For panting due to improper heat therapy, use Ophiopogon Decoction with modifications. For dual damage to qi and fluids, use Raw Wheat Powder with additions. For exhaustion of yin fluids, use Three-Carapace Pulse-Restoring Decoction with additions. For prolonged illness damaging yin, use Major or Minor Wind-Stabilizing Pearl with modifications. (8) **Restoring yang to rescue from collapse method**: Use Ginseng and Aconite Decoction or Ginger and Aconite Decoction with additions, administered frequently. **Post-illness recuperation**: For spleen-stomach disharmony, use Two Old Ingredients Decoction with additions. For spleen-stomach disharmony with deficiency and fullness, use Magnolia Bark, Fresh Ginger, Pinellia, Licorice, and Ginseng Decoction. For post-illness deficiency vexation, use Gardenia and Fermented Soybean Decoction. For middle deficiency with qi sinking, use Center-Supplementing and Qi-Regulating Decoction with modifications.
Since the 1970s, severe adenovirus pneumonia has been observed to present with DIC manifestations. Hospitals such as Beijing Friendship Hospital have incorporated blood-activating and stasis-resolving medicinal substances, which have shown certain effects in preventing and treating DIC. The medications used include Chinese Angelica, Red Peony Root, Sichuan Lovage Rhizome, suberect spatholobus stem, leech, gadfly, Astragalus Root, and others.
In northern China, adenovirus pneumonia is severe. During the initial major outbreak in 1958, the mortality rate among hospitalized patients was as high as 25%. After treatment integrating Chinese and Western medicine, the mortality rate dropped to 5–10%. In the past decade, there have been no significant outbreaks, and sometimes the incidence in the north has even ranked second (with RSV pneumonia being the first). The severity of the disease has decreased, and the mortality rate is now below 5%. During outbreaks, most deaths occur between the 10th and 15th days of the illness. The main factors affecting prognosis are: ① Young age and lack of specific antibodies—most deaths occur in children aged 6–18 months, with almost no deaths in those over 2 years old; ② Complication or secondary infection during measles, general pneumonia, or other severe illnesses leads to a higher mortality rate. Secondary infections such as Staphylococcus aureus or Escherichia coli also result in a more severe prognosis; ③ Compared to pneumonia caused by adenovirus types 3 and 11, type 7 generally leads to more severe cases and higher mortality.
The oral live attenuated vaccines for adenovirus types 3, 4, and 7 have been proven effective in small-scale applications abroad but have not yet been mass-produced or widely used. During outbreaks, especially in hospital wards, every effort should be made to isolate patients to prevent cross-infection. In community settings, home treatment for upper respiratory infections in infants and young children should be prioritized. In childcare facilities, early isolation is crucial, and caregivers with common colds should be temporarily relieved of their duties to minimize transmission risks.
During the course of adenoviral pneumonia, infections such as Staphylococcus aureus, large intestine bacillus, pneumococcus, Klebsiella pneumoniae, and Pseudomonas aeruginosa may complicate the condition, leading to a more severe tendency of disease. In the late stage [third stage] of adenoviral pneumonia, the following points often indicate the presence of secondary bacterial infection: ① No improvement in the condition around the 10th day of illness, or a relapse after initial grade I relief; ② Sputum turning yellow or resembling rice water; ③ Presence of purulent foci in other parts of the body; ④ Development of empyema; ⑤ New shadows appearing on X-ray examination; ⑥ Increased white blood cell count and elevated proportion of neutrophils or a left shift in the nucleus; ⑦ Elevated values in neutrophil alkaline phosphatase or nitroblue tetrazolium staining.
During the critical phase (days 6–15 of illness) of severe adenoviral pneumonia, a few cases may develop disseminated intravascular coagulation (DIC), especially when secondary bacterial infection is present. Before the onset of DIC, microcirculatory dysfunction is observed, initially manifesting as minor bleeding in the respiratory and gastrointestinal tracts, followed by widespread bleeding in the lungs, gastrointestinal tract, and skin. The diagnosis is confirmed through preliminary screening tests, screening tests, and confirmatory tests. Positive fecal occult blood test and reduced platelet count are key indicators in the preliminary screening. A definitive diagnosis is based on two abnormal findings out of three (thrombocytopenia, decreased fibrinogen, prolonged prothrombin time) or one abnormal finding out of three (positive protamine paracoagulation test [3P test], ethanol gel test, or shortened euglobulin lysis time).
Changchun Bethune Medical University found that severe cases or those complicated by type 7 or 3 adenoviral myocarditis are characterized by acute onset and rapid recovery. This typically occurs in the early second week of the illness, with recovery accelerating as myocardial hypoxia and edema resolve. However, due to concurrent heart failure, myocarditis is often misdiagnosed as fistula disease. Attention should be paid to sudden onset of pallor, profuse sweating, vomiting, abdominal pain, enlarged cardiac borders, increased or decreased heart rate, and hepatomegaly. Electrocardiograms and myocardial enzyme tests should be routinely performed to confirm the diagnosis.
Differential diagnosis should particularly focus on preschool and school-age children. The clinical manifestations of adenovirus and mycoplasma pneumonia are almost identical, with both presenting high fever, while symptoms such as difficulty breathing and drowsiness are relatively mild. However, adenovirus pneumonia generally has signs, whereas mycoplasma pneumonia may only show X-ray shadows without rales or other signs, which may aid in differentiation. In many cases, definitive diagnosis can only rely on specific laboratory tests.
In infants under 5 months, the clinical manifestations of adenovirus pneumonia are significantly milder compared to those in young children, making it indistinguishable from pneumonia caused by respiratory syncytial virus or parainfluenza virus. Differentiation can only be achieved through rapid or pathogen-specific diagnostic methods.




