| disease | Meniere's Disease |
| alias | Meniere's Disease, Meniere's Syndrome |
In 1861, the Frenchman Meniere first reported a case of a 12-year-old girl who, after catching a cold, suddenly developed tinnitus, deafness, and persistent nausea, vomiting, and vertigo, and died on the fifth day. An autopsy revealed inner ear hemorrhage. At the time, the medical community attributed this condition to cerebral apoplexy, but only he provided a detailed description of the disease, adopting Flourens' (1842) concept of labyrinth physiology and affirming that it was an inner ear disorder. To commemorate his diagnostic significance, the condition was named after him. Looking back now, the girl he reported likely suffered from leukemia complicated by inner ear hemorrhage. Since then, clinically, cases of unknown origin exhibiting the triad of vertigo, tinnitus, and deafness have often been referred to as Meniere's syndrome or symptom complex. In 1936, Hallpike and others, during autopsies of patients who died from craniotomy, discovered that the histopathological changes involved dilation of the endolymphatic spaces in the inner ear, leading to the terms labyrinthine hydrops or endolymphatic hydrops. It was also called aural vertigo, resulting in considerable confusion in nomenclature. In 1962, an international conference decided to retain only the name Meniere's disease, abolishing all other terms. In fact, endolymphatic hydrops is not unique to Meniere's disease. According to Belal's report, among 47 cases (57 ears) of endolymphatic hydrops, only 9 cases (11 ears) exhibited symptoms of Meniere's disease, accounting for about one-fifth. Thus, the two terms are not synonymous.
bubble_chart Epidemiology
Incidence rates vary significantly due to differing diagnostic criteria among studies. Cawthorne (1954) reported that among 2,000 vertigo cases, 60% were Ménière's disease; Williams (1958) found Ménière's disease accounted for 17.5% of 632 vertigo cases. In a domestic study by 301 Hospital involving 9,000 vertigo cases, the incidence was 11%. In Japan, Nagayasu reported a 17% incidence among 626 vertigo patients. Unilateral cases are more common, with Walsh (1956) noting that 83.5% of 127 cases involved one ear. The disease predominantly affects individuals aged 30–50, with adolescents accounting for only 7–10%. There is no significant gender difference, though some reports suggest a higher prevalence in males. Residents of colder regions show lower incidence rates. According to Matsunaga (1976), the disease is more prevalent in developing countries and urban populations. Recent literature indicates a rising trend, possibly linked to increased air pollution and chemical drug poisoning diseases.
bubble_chart EtiologyThe causes of the disease are multifaceted and generally include the following factors:
1. Circulatory disorders of the inner ear Many pieces of evidence suggest that autonomic nervous system dysfunction leads to spasms in the inner ear blood vessels, reducing blood flow in the vascular stria. This results in decreased secretion of endolymph, accumulation of intermediate metabolites, increased osmotic pressure in the cochlear duct, and fluid infiltration from the perilymphatic space and blood vessels into the endolymph, causing fluid accumulation. Patients with Ménière's disease exhibit reduced blood pressure responsiveness to endogenous or exogenous norepinephrine, possibly due to dysfunction in α-adrenergic receptors. Cervical spondylosis affecting the vertebrobasilar circulation can also trigger the disease, while emotional stress and excessive fatigue often serve as precipitating factors.
2. Congenital developmental abnormalities Congenital anatomical anomalies, such as underdeveloped ears, anterior displacement of the sigmoid sinus, occlusion of the cochlear aqueduct, narrowing or blockage of the endolymphatic duct, underdeveloped or absent endolymphatic sac, or developmental stenosis or atresia of the utricular valve or any membranous labyrinthine passage, can all lead to this condition.
3. Endocrine disorders and metabolic abnormalities Iwata (1958) first proposed that this syndrome is caused by endocrine imbalance between the pituitary and adrenal glands. Disorders in alcohol and lipid metabolism, increased plasma osmotic pressure, and changes in electrolyte and protein components—particularly imbalances in potassium levels in the blood and lymph—can contribute to the disease. Increased blood viscosity, hyperlipidemia, and low fibrinogen levels may also induce the condition. Additionally, adrenal cortex dysfunction and hypothyroidism can cause autonomic nervous system disorders, leading to inner ear circulatory disturbances and resulting in labyrinthine hydrops.
4. Craniocerebral trauma Trauma causing temporal bone fractures or inner ear hemorrhage can obstruct the cochlear or vestibular ducts, disrupting endolymph circulation and leading to fluid accumulation.5. Inner ear immune reactions Quinke (1893) suggested that the disease is related to angioneurotic edema. Duke (1923) proposed a direct link to Type I hypersensitivity reactions, with common food allergens such as wheat, beef, milk, and eggs, and less common inhalant allergens like Mongolian snakegourd root and dust. Symptoms can be triggered by ingesting allergenic foods or intradermal injections of allergenic extracts and may subside upon eliminating the offending allergen. According to Pulec, Type I hypersensitivity accounts for 14% of 162 Ménière's disease cases. Animal experiments by Jiro Ozawa, using chicken serum and subcutaneous tuberculin injections into the stylomastoid foramen, demonstrated that Type III hypersensitivity (antibody-antigen reactions) mediated by humoral immunity can increase vestibular membrane permeability and enhance vascular stria secretion, leading to endolymphatic hydrops. The clinical community has accepted the fact that local antibody production occurs in the inner ear. Research suggests that autoantigens may include inner ear membrane tissue vessels, ear matrix structures, the endolymphatic sac, and type II collagen in avascular areas of the inner ear. Hughes (1983) reported that autoimmune-induced Ménière's disease accounts for about 10% of cases, while Shea (1982) estimated it at 50%.
6. Other factors Chronic tonsillitis, sinusitis, appendicitis, cholecystitis, and other bacterial toxins, viral infections, or syphilis may increase duct wall permeability through toxicity, injury, or immune reactions, leading to labyrinthine hydrops.
In summary, neurovascular dysfunction of the labyrinth is the underlying basis of this disease, with multiple contributing factors. The exact pathogenesis remains unclear and requires further research.bubble_chart Pathological Changes
The production and absorption cycle of endolymph is related to the balance between longitudinal and radial flow of lymph in the inner ear, with longitudinal flow playing a dominant role. Endolymph is produced by the stria vascularis of the cochlea and the dark cells of the utricle in the vestibular system, and is phagocytized and absorbed by the endolymphatic sac. Radial flow refers to the perilymph, which can transform into endolymph by permeating through the vestibular membrane into the cochlear duct, and is selectively absorbed by the stria vascularis of each cochlear turn. The endolymphatic sac is now widely recognized as an important phagocytic and absorptive tissue, playing a significant role in labyrinthine hydrops. This sac absorbs endolymph, participates in the metabolism of mucopolysaccharides and proteins, and can produce phagocytes while regulating endolymphatic pressure. If neurovascular dysfunction occurs in the inner ear, it may lead to excessive production or insufficient absorption of endolymph, resulting in endolymphatic hydrops. When endolymphatic pressure rises to a certain level, the vestibular membrane may rupture, causing a mixture of endolymph and perilymph. The potassium-rich endolymph entering the perilymphatic space can lead to potassium intoxication in the vestibular receptors, inhibiting the excitation of sensory cells and clinically manifesting as tinnitus, deafness, and episodic vertigo. After 2–3 hours, as potassium ion concentration decreases, vertigo also subsides, gradually returning to normal. The repeated rupture and repair of the membranous labyrinth constitute the entire course of Ménière's disease. Since the basilar membrane at the cochlear apex is wider than that at the base, increased endolymphatic pressure first affects the apical basilar membrane. Alternatively, endolymph may initially enter the scala vestibuli of the cochlear apex through the helicotrema, causing potassium intoxication in hair cells, which explains why low-frequency hearing loss often occurs in the early stages. The key pathological changes in Ménière's disease include: ① Membranous labyrinth hydrops with cochlear duct dilation, most pronounced at the apex; ② In grade III dilation, the vestibular membrane bulges into the scala vestibuli, sometimes occupying the entire scala vestibuli, or even herniating through the helicotrema into the scala tympani; ③ Vestibular dilation primarily affects the saccule, which may expand 4–5 times in volume, adhering beneath the stapes footplate. Rupture of the vestibular membrane can form fistulas, folds, or collapse, while the utricle is pushed inward and upward, potentially protruding into the ampullated end of a semicircular canal, distorting or rupturing the crista ampullaris. ④ Scattered loss of outer hair cells in the middle turn of the cochlea, patchy atrophy of the stria vascularis in the middle and apical turns, frequent injury to vestibular hair cells, and absence of dilation in the endolymphatic sac, with epithelial folds disappearing, cellular deformation, and fibrosis of the sac wall.
bubble_chart Clinical Manifestations
Unilateral tinnitus and deafness accompanied by sudden vertigo attacks are characteristic of this disease. In the early stages, a major attack may be followed by a long period of normalcy, while some cases may experience recurrent attacks over days or weeks, with varying lengths of intervals. During the intervals, aside from tinnitus and deafness, the patient is generally normal. After early attacks, tinnitus and deafness may also completely resolve, but repeated episodes can gradually lead to irreversible tinnitus and sensorineural deafness. Before an attack, tinnitus often worsens, accompanied by a feeling of ear fullness, or even precursors such as fever-like sensations and dull pain behind the ear. Emotional agitation can trigger an attack, and the premenstrual period or late-stage pregnancy [third trimester] may increase susceptibility. The main symptoms are as follows:
1. Tinnitus Early-stage tinnitus is typically low-pitched, later becoming high-pitched and continuous, resembling the hum of a generator. Before a vertigo attack, tinnitus often worsens or changes in character as a precursor. Bilateral tinnitus is rare in the early stages, accounting for only 10–15%. In advanced stages, both ears are often affected. The severity of tinnitus and deafness correlates with the duration of the condition.
2. Deafness In the initial stage [first stage], 85% of cases present with unilateral low-frequency sensorineural hearing loss. In the intermediate [second stage] or advanced stages, the hearing loss becomes flat or sloping. After early attacks, hearing may partially or fully recover, but prolonged illness leads to irreversible hearing loss. In rare cases, a single attack may result in complete hearing loss. Patients often exhibit hyperacusis and recruitment, and some may perceive pure tones as two different pitches or timbres, known as diplacusis. Speech discrimination is poor, and if both ears are affected, hearing aids may be difficult to use.
3. Vertigo Vertigo often follows tinnitus as a precursor, manifesting as sudden rotational dizziness, spinning or swaying toward the affected side, and difficulty standing. Patients may tightly grip objects, close their eyes, and lie in a specific position. Severe cases may experience nausea, vomiting, pallor, and cold sweats. In rare instances, patients may suddenly collapse but remain conscious—a hallmark feature. Headache and impaired consciousness are rare during attacks. The duration of an attack ranges from minutes to days, rarely exceeding 1–2 weeks, with symptoms gradually subsiding until complete resolution. Some patients experience minor episodes after major attacks, such as positional vertigo or sudden collapse upon changing posture. Intervals between attacks vary from hours, days, months, or even years. Frequent recurrences lead to irreversible tinnitus and deafness. The three main symptoms vary depending on the affected site: cochlear damage primarily causes tinnitus and deafness with mild vertigo, whereas vestibular damage predominantly causes vertigo. According to Mawson (1963), 50% of cases involve simultaneous vestibular and cochlear symptoms, 25% present with tinnitus and deafness as the first symptoms, and 25% begin with vertigo. Generally, tinnitus, deafness, and vertigo occur together but with varying severity—this triad is a diagnostic hallmark. When the saccule expands and adheres to the stapes footplate, sometimes forming fibrous adhesions, pressure on the external auditory canal may induce vertigo or a sensation of falling (Hennebert’s sign). Loud sounds may also trigger vertigo (Tullio phenomenon).
4. Ear Fullness About 40% of patients experience ear fullness and pressure before an attack, with the severity correlating with the degree of endolymphatic hydrops. Some foreign scholars report that 7–20% of patients also suffer from migraines, though this is rare domestically.
5. Vagal Nucleus Irritation Symptoms Vestibular excitation during menstruation or pregnancy stimulates the vestibular nucleus and spreads to the vagal nucleus, leading to nausea, vomiting, pallor, cold sweats, bradycardia, or even syncope during attacks. Some cases present with abdominal pain and diarrhea, leading to misdiagnosis as acute abdominal conditions. Others may exhibit ipsilateral nasal congestion or rhinorrhea, resembling vasomotor rhinitis.
bubble_chart Auxiliary Examination
During the attack stage, there may be spontaneous horizontal nystagmus or horizontal-rotatory nystagmus, with the fast phase directed toward the affected side, which becomes more pronounced when the eyes are closed. In the late stage of the attack [third stage], the direction of nystagmus shifts to the healthy side, presenting as paralytic nystagmus, which gradually disappears thereafter. It is difficult to conduct detailed examinations during an attack, so the following tests are often performed during the intermittent phase:
I. Auditory Function Shows typical cochlear sexually transmitted disease changes.
1. Pure-tone audiometry In the early stage, low-frequency sensorineural deafness is observed. In the intermediate stage [second stage], a flat-type hearing loss is common. During the attack stage, hearing worsens, but partial or complete recovery may occur afterward, resulting in fluctuating hearing curves. In the advanced stage, the hearing curve stabilizes into a declining pattern. Hearing loss typically ranges between 50–70 dB within 5–10 years after onset.
2. Speech audiometry Speech reception thresholds (SRT) correlate well with pure-tone thresholds. Due to sound distortion, speech discrimination scores may drop to 40–70%. According to Stahle (1976), who followed 356 patients for years, the average speech reception threshold was 62 dB, with a discrimination score of 52%, and the average pure-tone loss was 55 dB.
3. Suprathreshold function tests The alternate binaural loudness balance (ABLB) test is positive. The difference limen for intensity (DLI) is below 0.6 dB, and the short increment sensitivity index (SISI) is elevated to over 80%, indicating the presence of auditory recruitment.
4. Impedance audiometry Type A tympanogram is observed, with no tone decay or acoustic reflex decay. If the difference between the stapedius reflex threshold and hearing threshold is below 60 dB, it is called Metz positive, also suggesting recruitment.
5. Bekesy audiometry Shows a Type II curve.
6. Electrocochleography (ECochG) The SP/AP amplitude ratio exceeds 37%. Gibson reported that an increased SP-AP wave width ratio is more significant than an increased amplitude ratio.
II. Vestibular Function Tests Vestibular function may be normal in the early stage but gradually declines with frequent attacks. In the advanced stage, it may be completely lost.
1. Hallpike caloric test This is the most commonly used method. Approximately one-third of patients show normal responses, one-third show weakened responses, and the remaining one-third show no response. Cawthorne et al. conducted caloric tests on 900 patients, finding canal paresis in 640 cases, directional preponderance in 75 cases, a combination of both in 108 cases, and inconclusive records in 26 cases. Canal paresis and directional preponderance were the most common findings. Vestibular dysfunction is most severe within the first five years of the disease and correlates with cochlear dysfunction. For simplified outpatient testing, irrigating the posterosuperior quadrant of the tympanic membrane with 2 ml of ice water can yield qualitative results.
2. Electronystagmography (ENG) Nystagmus is mostly horizontal, with severe cases showing horizontal-rotatory nystagmus. In the acute phase, nystagmus beats toward the opposite side, later shifting to the ipsilateral side, termed recovery nystagmus. Myerhoff (1981) performed ENG on 211 patients, finding normal responses in 21%, canal paresis in 65%, and directional preponderance in 14%. Normal responses do not rule out the condition. Saccadic, smooth pursuit, and optokinetic tests are normal, while rotational and galvanic stimulation tests may show reduced or normal function. Recently, sinusoidal harmonic acceleration (SHA) vestibular testing has been used, providing reproducible and controllable stimulation to assess phase gain, phase lag, and directional preponderance. Phase lag is the most sensitive parameter, and its combination with phase gain is ideal.
3. Other tests Neurological examinations are normal. The tympanic membrane is normal. Temporal bone tomography, as reported by Cole (1972) in 250 cases, showed bilateral labyrinthine otosclerotic lesions in 25 cases (10%). It also helps exclude internal auditory canal enlargement due to acoustic neuroma.
Taking a thorough medical history is crucial. Diagnosis is straightforward for those with the classic triad of symptoms, but it becomes more challenging for patients presenting only with tinnitus and deafness without vertigo, or vertigo without tinnitus and deafness. In such cases, a detailed examination is necessary to rule out other conditions, and sometimes long-term follow-up is required for a definitive diagnosis. According to Pulec (1977), in a study of 120 cases followed for five years, 46% had specific predisposing factors: allergies (14%), adrenal insufficiency (7%), hypothyroidism (2%), insufficient sex hormones (2%), vascular insufficiency (3%), congenital or acquired syphilis (6%), and mixed sexually transmitted diseases (12%). When possible, systematic endocrine function tests, glucose tolerance tests, syphilis antibody tests, and skin allergen tests should be conducted. For suspected patients during the intermittent phase, a glycerol test should be routinely performed: After fasting for two hours, the patient orally ingests a 50% glycerol solution at a dose of 3 mL (1.5 g)/kg, administered in one dose. Pure-tone and speech audiometry are performed before administration and repeated hourly for three hours afterward. An improvement of 12% or more in air conduction hearing at 250, 500, and 1000 Hz is considered positive. Early-stage patients whose hearing has already recovered during the intermittent phase or advanced-stage (grade III) patients with irreversible hearing damage may test negative, though false positives are rare. High doses of glycerol may cause nausea and headaches, so a half-dose is now recommended without reducing efficacy. Some clinicians use furosemide (Frusemide) instead of glycerol for testing, as it offers a higher positive rate and fewer side effects. If early-stage patients have normal hearing, a loading test may precede the glycerol test: the patient takes 2 g of salt orally daily for 14 days to induce hearing deterioration before proceeding with the glycerol test as described. According to Dobie (1982), among 196 glycerol tests, 64.8% were positive, 26.5% negative, and 8.7% inconclusive. Patients with a disease duration exceeding 15 years had twice the positive rate of those with shorter durations. Advanced-stage patients had a positive rate deficiency of 26%, so a negative test does not rule out Ménière's disease. Although mannitol has strong dehydrating effects, its large molecular size prevents it from crossing the lymphatic membrane, making it unsuitable for this test.
bubble_chart Treatment Measures
1. General Treatment A low-salt, low-fat diet should be adopted, with daily salt intake not exceeding 1g. Pay attention to physical exercise to enhance constitution, maintain a balance between work and rest, and ensure living spaces are well-ventilated and painted in dark gray. Avoid mental stimulation and abstain from smoking and alcohol.
2. Drug Treatment Medications can be used in the early stages, and the following drugs may be considered as appropriate.
1. Sedatives - Dimenhydrinate 50mg, three times daily, can alleviate vertigo, nausea, and vomiting. - Chlorpromazine Hydrochloride 25mg, three times daily, has drowsiness and sedative effects. - Diazepam 2.5–5mg, three times daily, provides good sedation and sleep-inducing effects.
2. Vasodilators
(1) Nicotinic Acid 50–100mg, three times daily, taken orally half an hour before meals. Can be used long-term, with the dose adjusted to the point of facial flushing and fever after administration.
(2) Tangut Anisodus Alkali (654-2) Relaxes smooth muscles and relieves spasms in small blood vessels. Oral administration is less effective; intramuscular injection of 5–10mg or intravenous drip of 30–40mg is preferred.
(3) Tolazoline An α-blocker with vasodilatory and antispasmodic effects. Take 25mg orally three times daily or administer intramuscularly. Contraindicated in patients with gastric ulcers or heart disease.
(4) Padutin A vasodilatory hormone. Administer 10U dissolved in 1.5ml of sterile water via intramuscular injection. Contraindicated in patients with hypertension or heart disease.
(5) 5% Sodium Bicarbonate 40–50ml via intravenous injection or 250ml via intravenous drip. Neutralizes acidic metabolic products in tissues, releases CO2, dilates microvessels in the inner ear, and improves microcirculation.
(6) Papaverine Has significant smooth muscle relaxant effects and benefits cerebral and coronary arteries. Administer 30mg via intravenous drip.
(7) Cinnarizine 25–50mg orally three times daily or 20–40mg via intravenous drip. Dilates capillaries and reduces vascular fragility.
(8) Inhalation of 7% CO2 and 95% O2 Mixture Dilates microvessels, increases oxygen partial pressure in endolymph, and lowers pH. Alternatively, inhale 7% CO2 alone for 5 minutes per session.
3. Microvascular Dilators and Blood Viscosity Reducers (Chinese Medicinals)
(1) Salvia Dilates blood vessels, reduces plasma viscosity, and decreases fibrinogen levels. Administer orally or via intravenous drip.
(2) Ligustrazine Dilates small blood vessels and reduces platelet aggregation. Administer 40–80mg via intravenous drip.
(3) Ilex Pubescens Alkali Reduces platelet aggregation and counteracts thrombosis.
4. Calcium Channel Blockers Intracellular calcium overload can cause vasoconstriction, reduced red blood cell deformability, and microcirculatory disorders, leading to vertigo. Sibelium (Flunarizine) is a selective calcium ion blocker that prevents intracellular calcium overload, improves cochlear microcirculation, reduces vestibular excitability, and enhances neuronal hypoxia tolerance. It lacks the myocardial suppression and hypotensive side effects of typical blockers. Take 10mg orally once or twice daily.
5. Diuretics Primarily used during the attack stage.
(1) Acetazolamide (Diamox) Inhibits intracellular carbonic anhydrase, reduces sodium-hydrogen ion exchange, facilitates sodium and potassium excretion, and decreases endolymph volume. Take 250mg orally every 6 hours or administer 500mg via intravenous drip. For long-term use, supplement with 1g of potassium chloride orally three times daily.
(2) Hydrochlorothiazide 25mg, three times daily. Prolonged use may reduce blood potassium levels. Triamterene also has diuretic effects, and prolonged use may increase blood potassium levels. The usual dosage is 50-100mg, three times daily. Both medications can be taken together at reduced doses. Regular monitoring of blood potassium and sodium levels is recommended.
(3) Isosorbide Dinitrate - Has the effects of mannitol and urea, is easily absorbed by the intestines, and can be prepared as an 85% solution for intravenous drip at 1.6 ml/kg, or as a 70% solution for oral administration, 30 ml each time, three times a day. It can be taken for one month without any side effects.
6. Vestibular Function Disruptors - Suitable for patients with bilateral conditions or those in poor physical condition who cannot undergo surgery. Use streptomycin sulfate 1 g intramuscularly, three times a day. After 3–4 weeks, the patient may experience unsteady walking. During medication, perform caloric testing daily or pure-tone audiometry every other day. If hearing declines or there is no response to 30°C cold water stimulation, discontinue use. Contraindicated in patients with renal dysfunction. Alternatively, inject 0.6 ml of a 25% solution into the tympanic cavity, or use gentamicin tympanic injection five times a day, 12 mg (0.3 ml) each time. A Politzer balloon can also be used to pressurize the external auditory canal to facilitate drug entry into the tympanic cavity. On average, after 3–4 days of medication, caloric function tests will turn negative.
7. Hormone Therapy - Suitable for patients with adrenal cortical insufficiency. Arenbery (1977) treated 75 cases with dexamethasone, with 90% experiencing symptom relief. Ariyasu (1990) treated 10 cases with prednisone, while another 10 received a placebo as a control. In the treatment group, nine out of ten cases showed significant symptom relief within 24 hours, compared to only three in the control group. The prednisone dose was 32 mg on the first day, 16 mg on days 2–4, then reduced by 4 mg daily until discontinuation. Some reports indicate this drug is ineffective, and it is now rarely used.
8. Acute Stage of Attack Management - Focuses on treating vertigo, nausea, and vomiting. Emergency measures, in addition to the aforementioned medications, include the following methods:
(1) Cold Water Irrigation of the External Auditory Canal - Based on the principle of caloric vestibular stimulation, irrigate the external auditory canal (the ear canal toward which the nystagmus fast phase points during an attack) with 5–10 ml of 30°C cold water or ice water. This induces nystagmus in the opposite direction, counteracting vestibular stimulation and rapidly improving vertigo. This method is simple, practical, and yields quick results.
(2) Block Therapy - Use 0.1% procaine or lidocaine, calculated at 1–1.5 mg/kg, dissolved in a 5–10% glucose solution for slow intravenous drip. This relieves vascular spasms and stops vertigo attacks. During the attack stage, 0.5–0.8 ml of lidocaine can also be injected into the tympanic cavity for the same effect.
III. Chinese Medicine Treatment - Traditional Chinese medicine offers unique approaches to treating Ménière's disease, typically involving pattern identification and tailored treatment.
1. Chinese Herbal Medicine - Commonly used herbs include Pinellia 9g, Gastrodia Tuber 9g, raw White Atractylodes Rhizome 9g, Chinese Angelica 9g, Sichuan Lovage Rhizome 6g, Poria 12g, fried Immature Orange Fruit 6g, fresh Bamboo Shavings 12g, Acorus 3g, and Tangshen 9g, decocted in water and taken daily. Alternatively, Schisandra Fruit 9g, Chinese Yam 9g, Sour Jujube 9g, Chinese Angelica 9g, dried longan pulp 15g, and Liquorice Root 6g can be decocted and taken.
2. Acupuncture Therapy - Main points: Fengchi (GB20), Baihui (GV20), Yintang (EX-HN3), Hegu (LI4), and Taichong (LR3). Secondary points: Neiguan (PC6), Zusanli (ST36), Sanyinjiao (SP6), Weizhong (BL40), and Qiangjian (GV18). Fengchi, the convergence point of the Foot Shaoyang, Yangwei, and Yangqiao meridians, dispels wind and awakens the spleen, making it a universal point for vertigo. Yintang calms the mind. Retain needles for half an hour with intermittent manipulation. Zusanli can also be treated with moxibustion to invigorate the spleen and resolve phlegm.
IV. Surgical Therapy - For cases unresponsive to long-term conservative treatment, surgery may be considered. According to Pulec (1977), a follow-up of 120 cases showed that 46% were cured with medication after identifying the cause within five years, while only 54% required surgery. Since most current surgeries are destructive, strict criteria should be applied. Rubin recently reported that only 10% of cases require surgery, while Clemis reported 5%. In recent years, Shea has proposed the following treatment plan for reference:
Initial stage [first stage]: Cochlear hydrops, ear fullness, tinnitus, fluctuating deafness, treated with a low-salt diet and medication.
The intermediate stage [second stage]: Cochleovestibular hydrops, fullness sensation, vertigo, tinnitus, fluctuating hearing loss, treated with medication or endolymphatic sac decompression.
The late stage [third stage]: Severe vertigo, tinnitus, non-fluctuating hearing loss, treated with medication, streptomycin perfusion, or vestibular nerve section.
Fourth stage: Severe endolymphatic hydrops, tinnitus, non-fluctuating deafness, unsteadiness, rare vertigo attacks, no treatment required, hearing aids may be used.
Fifth stage: Complete hearing loss, unsteadiness, no vertigo attacks, no treatment required, cochlear implantation may be performed.
Our surgical indications are: ① Recurrent tinnitus, deafness, and vertigo severely affecting life and work, with no improvement after aggressive conservative drug treatment for over six months. ② Pure-tone hearing loss of 30dB or more in speech frequencies, with speech discrimination below 50%. For bilateral cases, conservative surgical treatment should be performed earlier. ③ Unilateral cases with pure-tone hearing loss of 40–50dB, recurrent vertigo, and frequent attacks are suitable for vestibular nerve section.
There are many types of surgery for this condition. Representative surgical methods are introduced below:
1. Labyrinthine destructive surgery: Mollison (1931) first applied labyrinthine fenestration (or resection) for treatment. Suitable for advanced-stage patients with poor hearing, such as those with pure-tone hearing loss exceeding 50dB. Under local or general anesthesia, a postauricular incision is made, the mastoid is fenestrated, the antrum is located, and a small cutting burr is used to enlarge the antrum, exposing the short process of the incus. The lateral semicircular canal is identified superior and medial to it, and the bony labyrinth of the superior and posterior semicircular canals is sequentially drilled open. A hook or dental root canal needle is then inserted into the three ampullae to completely remove the membranous labyrinth. Alternatively, a 2mm×4mm fenestration may be made in the horizontal semicircular canal to expose the membranous labyrinth, followed by injection of absolute alcohol into the membranous duct to fill it. Avoid overfilling to prevent spillage and injury to the facial nerve canal anteriorly. This procedure can also be performed via an endaural approach, lifting the tympanic membrane to remove the stapes and extracting the membranous labyrinth with a hook. Sometimes, the bony wall between the two windows may be removed with a drill to facilitate clearance of the membranous labyrinth. Streptomycin or neomycin powder may then be packed into the vestibular cavity to further destroy vestibular end organs. In the late 1960s [third stage], many scholars modified this procedure to selectively destroy the vestibular function while preserving cochlear function. The bony wall of the horizontal semicircular canal is thinned to 0.25–0.5mm without exposing the membranous labyrinth, followed by cryodestruction at −160°C. Alternatively, an ultrasonic generator head may be applied for destruction. During treatment, an assistant should closely observe the direction of the patient’s nystagmus until the fast phase shifts from ipsilateral to contralateral. This method can preserve hearing for a relatively long period, with about 80% of vertigo cases not recurring. Long-term follow-up shows difficulty in maintaining hearing (Figure 1).
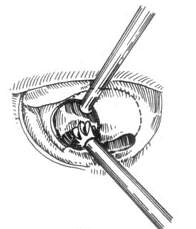

Figure 1 Labyrinthine destruction surgery
(1) Drilling away the bony wall between the two windows (2) Destroying the ampullary crests of the three semicircular canals with a hook
2. Membranous labyrinth occlusion or endolymphatic space blockage: Following the above method, the mastoid is fenestrated, and a window is created in the horizontal semicircular canal to expose the membranous labyrinth. Small pieces of gelatin sponge or autologous tragal cartilage are inserted into the vestibule without damaging the membranous labyrinth, merely occluding the endolymphatic space. This can suppress vertigo attacks for a relatively long period while preserving residual hearing.
3. Endolymphatic Sac Decompression First introduced by Portmann in 1926, this procedure involves a retroauricular incision, mastoid drilling, and extensive removal of the bone posterior to the labyrinth and anterior to the sigmoid sinus to expose the cerebellar dura mater and the endolymphatic sac. After identifying the sac wall, a longitudinal incision is made with a fine knife. To prevent healing and ensure long-term drainage, silver clips may be used to hold the incised sac wall open, or specialized thin membranes or small tubes can be placed within the sac cavity to drain endolymph into the mastoid cavity or subarachnoid space. Recently, some have suggested that simply incising and exposing the endolymphatic sac without drainage can also achieve therapeutic effects. According to recent reports, the surgical success rate ranges from 60% to 70%. As it is not a destructive procedure, it is suitable for early-stage patients with fluctuating hearing loss and can be considered a first-line surgical option (Figure 2).
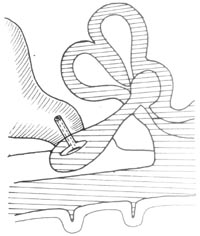
Figure 2 Endolymphatic Sac-Mastoid Shunt
4. Sacculotomy or Fistulization An ear incision is made, and the tympanic membrane is lifted according to the stapes surgery principle to expose the stapes footplate. A micro hand drill is used to create a hole in the footplate, and a prepared tack (cross-section 0.4mm × 0.4mm, thickness 0.1mm, length 1.3–2.1mm) is inserted into the hole and embedded in the footplate. This allows the enlarged saccule beneath the footplate to touch the tack and be punctured upon slight expansion under the tack's mechanism, enabling repeated punctures over time to achieve the goal of preventing vertigo attacks. The drawback is that it may cause endolymphatic hydrops, leading to sensorineural hearing loss. It is suitable for patients with poor hearing who have failed endolymphatic sac decompression.
5. Endolymphatic Shunt The tympanic membrane is lifted using the stapes surgery method. Pulec used a specially designed platinum tube to puncture the basilar membrane from the round window, connecting the cochlear duct to the promontory. Alternatively, Schuknecht's method employs a 300μm diameter, 3mm long right-angled hook needle to pierce through the round window membrane toward the oval window, reaching beneath the stapes footplate, and then through the osseous spiral lamina to the saccule, creating an artificial passage to form a permanent endolymphatic-perilymphatic fistula. This diverts endolymph into the perilymphatic space. Due to significant hearing damage, it is only suitable for patients with severe hearing impairment.
6. Cervical Sympathetic Ganglion (Stellate Ganglion) Resection Preoperatively, a stellate ganglion block should be performed to observe whether the patient's vertigo and hearing improve. Only those who respond positively are considered surgical candidates. Under local or general anesthesia, a 6cm horizontal incision is made one fingerbreadth above the clavicle, corresponding to the insertion point of the sternocleidomastoid muscle. The lateral sternocleidomastoid muscle and external jugular vein are severed to expose the anterior scalene muscle and phrenic nerve. The vertebral artery, branching dorsally from the subclavian artery, is identified. Medial to the vertebral artery and superior to the subclavian artery, the sympathetic stellate ganglion is located anterior to the seventh cervical vertebra. The upper and lower nerve branches are cut, and the ganglion is removed to enhance parasympathetic function, relieve inner ear vascular spasm, and achieve vasodilation to improve inner ear blood circulation. This is suitable for early-stage bilateral hearing impairment.
7. Vestibular Nerve Section As early as 1908, Frazer used auditory nerve section to treat otogenic vertigo. In 1932, Mekenzie began sectioning the vestibular branch instead to preserve hearing. Initially, a suboccipital craniotomy was used, but otologists now employ the labyrinthine or retrosigmoid approach and middle cranial fossa internal auditory canal opening.
(1) Retrolabyrinthine Approach Under local or general anesthesia, a postauricular incision is made, and the mastoid is drilled to remove as much bone as possible between the labyrinth and the anterior sigmoid sinus, exposing the dura mater. The dura is incised in a "U" shape and reflected forward. Cerebrospinal fluid is aspirated to enter the cerebellopontine angle, where the seventh and eighth cranial nerves are located. The surgical field is small (0.5cm × 0.7cm, rarely exceeding 1cm²), making illumination and exploration challenging. For convenience, the retrosigmoid approach is now preferred. A "∩" or oblique straight-line incision is made behind the mastoid, and a 3cm × 4cm occipital bone segment posterior to the sigmoid sinus is removed. The dura is incised to enter the cerebellopontine angle, providing a surgical field 2–3 times larger. Under microscopic guidance, the facial and auditory nerves are separated, and the anterior half of the auditory nerve fibers (vestibular nerve) are identified and cut with scissors.
(2) Middle Cranial Fossa Approach This technique was pioneered by House (1960) and is performed under local or general anesthesia. The patient is placed in a semi-sitting or lateral position. A vertical incision is made 1 cm anterior to the tragus and 6 cm above the zygomatic arch, extending deep into the temporal bone. A 3 cm × 4 cm bone window is created in the temporal bone. The dura mater at the skull base is separated from the outside inward to identify the three key landmarks: the foramen spinosum, the hiatus semilunaris, and the arcuate eminence. The foramen spinosum is where the middle meningeal artery enters the skull, and 0.5–1 cm posterior to it lies the facial hiatus, through which the greater superficial petrosal nerve exits. Using an electric drill, the bone is gradually removed outward from this point by 3 mm to expose the geniculate ganglion. From the posterior aspect of the ganglion, the roof of the internal auditory canal is drilled along the long axis of the facial nerve to expose the dura mater of the internal auditory canal. A "C"-shaped incision is made, and under the microscope, the medially and laterally arranged facial nerve and superior vestibular nerve branches are identified. Inferiorly lies the inferior vestibular branch, and medially inferior is the cochlear branch. At this stage, the superior and inferior vestibular branches can be severed without damaging the cochlear branch or the facial nerve. Sometimes, the vestibular nerve may also be excised to prevent regeneration. This method carries a high risk of facial nerve injury and requires advanced technical skills, making its widespread adoption challenging.
8. Others Rosen (1954) applied chorda tympani neurectomy, and Arslan (1971) used sodium chloride particles placed on the round window membrane, among other methods. However, these were abandoned due to uncertain efficacy or excessive damage to cochlear function. Tumarkin (1966) pointed out that negative pressure in the tympanic cavity could cause neurovascular disturbances in the inner ear, leading to Ménière's disease, which could be cured by tympanic membrane puncture or tube drainage. Hall (1977) found that nearly one-third of Ménière's disease patients exhibited negative pressure in the tympanic cavity, and sometimes tympanic tube insertion could achieve dramatic therapeutic effects.
In summary, there are many surgical treatment methods for this condition, each with its pros and cons, and the choice should be made based on individual circumstances. The most effective surgical treatment is vestibular nerve section, which can eliminate vertigo in 95% of cases. However, it does not cure endolymphatic hydrops, and hearing may continue to deteriorate in the future. Further research is needed to develop a definitive cure.
- Lermoyez Syndrome: First reported by Lermoyez (1919), characterized initially by tinnitus and deafness, followed by a sudden onset of vertigo, after which hearing improves. This differs slightly from Ménière's disease, where vertigo precedes deafness and tinnitus. It is now considered a variant of Ménière's disease, relatively rare, possibly caused by dysfunction of the autonomic nervous system in the inner ear. Treatment is the same as for Ménière's disease.
- Ototoxicity: Delayed vestibular damage, easily confused with this condition. However, tinnitus and deafness have a clear history of medication use, such as aminoglycosides, quinine, salicylates, and anticancer drugs.
- Positional vertigo: Occurs in a specific position and resolves with a change in position, with no tinnitus or deafness. Vestibular function may be normal.
- Sudden deafness: Occurs suddenly without any predisposing factors, with a one-time severe hearing loss, primarily in high frequencies, or even total deafness, sometimes accompanied by severe vertigo. There is no history of tinnitus or deafness before the onset. Vertigo improves within 3–7 days, but hearing rarely recovers.
- Vestibular neuronitis: No tinnitus or deafness, sudden onset of vertigo, possibly triggered by a cold. Spontaneous nystagmus toward the healthy side is observed, with weakened or lost vestibular function on the affected side. Sometimes, leukocytosis is present.
- Vertebrobasilar insufficiency: Cervical spine deformities or hyperostosis, hypertension, or arterial sclerosis can induce insufficient blood supply to the brainstem vestibular center or inner ear. Due to the complexity of symptoms, cardiovascular examinations, blood tests, and cervical spine CT or X-rays should be performed.
- Acoustic neuroma: Early unilateral tinnitus and deafness, occasional dizziness, rarely rotational sensations. Hearing tests indicate retrocochlear damage, such as tone decay, prolonged I–V wave intervals, disappearance of wave V. X-rays of the internal auditory canal show enlargement, and CT scans reveal tumor images for differentiation.
- Chronic brainstem ischemia: Young and middle-aged individuals with hypotension may experience dizziness and falls when standing. In the elderly, arterial sclerosis and ischemia can cause bilateral tinnitus and deafness, often with unsteadiness upon rising or standing, but not episodic vertigo. Vestibular function is usually within the normal range.




