| disease | Wet Lung |
| alias | Newborn Wet Lung, Temporary Difficulty Breathing, Transient Dyspnea, Wet Lung of the Newborn |
Wet lung is a self-limiting disease caused by fluid accumulation in the lungs, and the incidence of this condition is quite high in China.
bubble_chart Pathogenesis
Before birth, the fetal alveoli contain a certain amount of fluid (approximately 30 ml/kg; refer to the fetal lung fluid in the anatomical and physiological characteristics of the respiratory system). This fluid prevents alveolar adhesion before birth and contains a certain amount of surfactant, facilitating alveolar expansion after birth. During passage through the birth canal, the fetal chest is subjected to a pressure of 9.31 kPa (95 cmH2O), causing about 20–40 ml of alveolar fluid to be expelled through the trachea. The remaining fluid moves to the pulmonary interstitium and is then transported by pulmonary lymphatic vessels and veins, primarily via lymphatic vessels. The absorption and distribution of fetal lung fluid are hindered when capillary and/or lymphatic pump pressure decreases, hydrostatic pressure increases, or alveolar or interstitial osmotic pressure rises. Conversely, decreased hydrostatic pressure also impairs fluid absorption. The volume of fetal lung fluid increases near term, making this condition more common in full-term infants. The incidence is higher in cases of intrauterine distress or postnatal asphyxia. Additionally, delayed absorption occurs in conditions like hypoalbuminemia or hypervolemia. The absorption of fetal lung fluid is related to Black Catechu phenolamines. In cesarean deliveries without labor, fetal blood levels of Black Catechu phenolamines are low, and albumin levels are reduced, leading to delayed lung fluid absorption and an increased risk of this condition.
bubble_chart Clinical ManifestationsThe medical history may include intrauterine distress or birth asphyxia, and it is more common in male infants than in females. Breathing is mostly normal at birth, with tachypnea appearing approximately 2–5 hours later. If asphyxia occurs at birth, tachypnea appears immediately after resuscitation, with a respiratory rate of 60–80 breaths per minute or more, sometimes exceeding 100. Cyanosis is present around the lips, but the infant’s response is normal, crying is loud, and feeding is unaffected. In more severe cases, cyanosis is pronounced, responsiveness is poor, the infant may groan, refuse to eat or cry, body temperature remains normal, and lung sounds are diminished or coarse moist rales are heard. Wet lung can be classified into clinical and asymptomatic types, with the latter showing signs of wet lung only on chest X-rays.
Blood gas analysis shows that pH, Pco2 , and BE are generally within the normal range. In severe cases, respiratory acidosis and metabolic acidosis may occur, along with grade I hypoxemia and hypercapnia. The prognosis is good, with milder cases recovering normal breathing within 5–6 hours or one day, while more severe cases may take 4–5 days to recover.
The medical history may include intrauterine distress or birth asphyxia, and it is more common in male infants than in females. Breathing is mostly normal at birth, with tachypnea appearing approximately 2–5 hours later. If asphyxia occurs at birth, tachypnea appears immediately after resuscitation, with a respiratory rate of 60–80 breaths per minute or more, sometimes exceeding 100. Cyanosis is present around the lips, but the infant’s response is normal, crying is loud, and feeding is unaffected. In more severe cases, cyanosis is pronounced, responsiveness is poor, the infant may groan, refuse to eat or cry, body temperature remains normal, and lung sounds are diminished or coarse moist rales are heard. Wet lung can be classified into clinical and asymptomatic types, with the latter showing signs of wet lung only on chest X-rays.
Blood gas analysis shows that pH, Pco2 , and BE are generally within the normal range. In severe cases, respiratory acidosis and metabolic acidosis may occur, along with grade I hypoxemia and hypercapnia. The prognosis is good, with milder cases recovering normal breathing within 5–6 hours or one day, while more severe cases may take 4–5 days to recover.X-ray findings are varied (Figures 1 and 2): ① Alveolar fluid accumulation signs: patchy, veil-like, or hazy opacities in the lung fields, or small nodular shadows with diameters of 2–4 mm. ② Interstitial fluid accumulation: reticular or linear shadows on X-ray. ③ Interlobar pleural effusion (mostly between the right upper and middle lobes) and small amounts of pleural effusion. ④ Other signs: dilation of hilar vessels due to static blood, appearing as thickened lung markings with clear margins, radiating outward from the hilum. ⑤ Signs of pulmonary edema: increased translucency. X-ray findings resolve within 24 hours in 71% of cases and within 72 hours in 97.8%, with occasional cases taking up to 4 days to resolve.
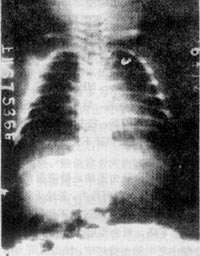
Figure 1: Wet lung
(showing alveolar fluid accumulation signs, with widespread patchy and nodular shadows in both lungs, particularly in the lower lobes)

Figure 2: Wet lung
(showing vascular static blood signs, with thickened lung markings radiating outward from the hilum, and linear fluid accumulation in the right horizontal fissure)
bubble_chart Treatment Measures
The main focus is on enhanced nursing care and symptomatic treatment. Provide oxygen when there is rapid breathing or cyanosis. If unable to ingest milk, administer 10% glucose solution intravenously at 60–80 ml/kg per day. In cases of metabolic acidosis, add 5% sodium bicarbonate at 2–3 ml/kg per dose, either intravenously or diluted and slowly injected, repeating if necessary. For dysphoria or moaning, administer phenobarbital at 3–5 mg/kg per dose. When there are numerous moist rales in both lungs, use furosemide at 1 mg/kg and address heart failure as needed.
bubble_chart DifferentiationThere are many disease causes of respiratory distress in newborns, which need to be differentiated from wet lung.
1. Differentiation between wet lung and mild hyaline membrane disease: see table
2. Amniotic fluid aspiration syndrome: This syndrome has a history of asphyxia or fetal distress, with rapid respiration mostly occurring after resuscitation, and some becoming apparent only several hours after birth. In contrast, wet lung mostly has no asphyxia, and rapid respiration appears later. X-ray signs and dynamic observation aid in diagnosis.
Table: Comparison between hyaline membrane disease and wet lung
| Hyaline membrane disease | Wet lung |
| More common in premature infants | More common in full-term infants or near-term premature infants |
| Often accompanied by perinatal distress | Mothers may have a history of excessive sedative use |
| Caused by surfactant deficiency | Caused by delayed absorption of lung fluid |
| Chest X-ray shows hypoventilation, reticular granularity, bronchial air shadow, and atelectasis | Chest X-ray shows normal aeration, thickened lung markings, and signs of interstitial and alveolar fluid accumulation; sometimes requires oxygen but not assisted ventilation |
| Requires continuous oxygen for several days, often needs assisted ventilation | Mild condition, good prognosis |
| Severe condition, poor prognosis |
3. Cerebral hyperventilation: Common in full-term infants with asphyxia, caused by cerebral edema. There are no lung lesions, but rapid respiration is present, often accompanied by respiratory alkalosis. The prognosis depends on the severity of asphyxia and the disease cause.




