| disease | Benign Prostatic Hyperplasia |
| alias | Prostate Hyperplasia, Prostatic Hypertrophy |
Benign prostatic hyperplasia (BPH) is one of the significant pathological conditions causing bladder neck obstruction in males. Pathologically, it is more appropriate to refer to it as prostatic hypertrophy. However, the term "prostatic hypertrophy" is more commonly used and thus continues to be employed. Additionally, the term "benign prostatic hypertrophy" is used to distinguish it from malignant prostate tumors. Since this does not seem to cause confusion, it is also omitted. BPH is a common disease among elderly males. Under the great socialist system of our country, the health standards of the people are continuously improving, and the average lifespan is steadily increasing, which inevitably leads to a gradual rise in the number of cases. Although BPH is a benign condition, the obstruction it causes in the urinary system affects urination and directly threatens kidney function, posing serious risks to the health and life of patients. Moreover, BPH often requires surgical treatment, and elderly patients frequently suffer from hypertension, vascular sclerosis, and cardiopulmonary insufficiency, which indeed places a heavy burden on them. Therefore, BPH is an important issue in the prevention and treatment of geriatric diseases. BPH is not uncommon in our country, although comprehensive statistical data are still lacking. In our hospital, 697 urological patients were treated in 1960 and 1961, of which 33 cases were BPH, accounting for approximately 4.6% of the urological inpatients. Shandong University Hospital treated 54 cases over 8 years, 15 hospitals in Shanghai treated 241 cases over 5 years, and Renji Hospital in Shanghai treated 58 cases over 5 years. The incidence of BPH varies among different ethnic groups worldwide. The incidence rate is lower in Asians compared to Caucasians, while Caucasians and Africans have similar rates. Additionally, the onset age is about ten years earlier in Caucasians and Africans than in Asians, with cases appearing as early as 40 years old and increasing with age. Among the cases, 10% are aged 40-49, and 20% are aged 50-59.
bubble_chart PathogenThe disease cause of prostatic hypertrophy has not been clearly understood to date. Previously, some (Carleton) believed that prostatic hypertrophy was related to excessive sexual activity, indulgence in lust, a disorderly lifestyle, incomplete treatment of posterior urethritis, urethral obstruction, and abnormal testicular function. Now, it seems difficult to say what the relationship is. Virchow once described the hypertrophied prostate as a "myoma" or "adenoma," using the theory of neoplasia to explain prostatic hypertrophy. Later, Deming (1935) and Moore (1943) and others raised objections to this theory, arguing that neoplasia is an abnormal mass of tissue that grows rapidly and irregularly; whereas hyperplasia is the hypertrophy of tissue cells, often compensating for the loss of similar tissue or compensating for the functional insufficiency of similar tissue. Similar situations can be seen in the thyroid, adrenal cortex, and pituitary gland. Other theories include the stirred pulse sclerosis theory, infection theory, metabolism and nutritional conditions theory, all of which are difficult to explain the essence of the problem. The endocrine theory is more capable of explaining the problem.
The endocrine theory has long observed that the development of the prostate is closely related to the testes. Removal of both testes can cause the prostate to atrophy. Destruction of the pituitary gland before puberty also stops the development of the prostate. Large amounts of estrogen can cause the prostate to atrophy. It is widely acknowledged that prostatic hyperplasia is due to the disorder of gonadal endocrine, but to date, there is still a lack of laboratory data to explain this issue. The details of endocrine disorders are also not precisely understood. For example, the testosterone content in the venous blood of the spermatic cord in normal males is between 0.025~1.6μg%. This value gradually decreases between the ages of 30 and 80 (Finkelstein 1961). Additionally, the excretion of 17-ketosteroids in urine at the age of 50~70 is only 40~55% of that in young males (Mac Donald 1962). However, the results of measuring the content of male hormones in patients are very inconsistent, with some being low, some high, and some unchanged. Lacssagne (1933) once believed that estrogen might be the disease cause of prostatic hypertrophy. Prostatic hypertrophy occurs in the "medullary part" such as the lateral and middle lobes of the prostate without causing the medullary part to degenerate; while the "cortical part" is not affected. Huggins believed that it was due to estrogen reducing the effect of androgen, thereby causing the medullary part to degenerate; while the "cortical part" or posterior lobe has a low response threshold to androgen, so it remains unchanged. Androgens and estrogens in the male body are simultaneously produced in the testes and adrenal cortex, and are controlled and regulated by pituitary endocrine to maintain their balance. From the perspective of treatment effects, estrogen and castration are more reliable for normal prostate and prostate cancer. Their effect on prostatic hypertrophy is not constant. The use of androgen or a combination of androgen and estrogen for the treatment of prostatic hypertrophy does not yield reliable results. In summary, prostatic hypertrophy is closely related to the disorder of gonadal endocrine, but its specific mechanism is still unclear.
bubble_chart Pathological ChangesBenign prostatic hyperplasia (BPH) can originate from the urethral glands or the prostate gland itself. When it originates from the prostate gland, it most commonly occurs in the median and lateral lobes, rarely in the anterior lobe, and never in the posterior lobe. The hypertrophic glandular nodules may be large and soft or small and hard, depending on the ratio of glandular tissue to muscle fibers. The hypertrophic glandular nodules compress the surrounding normal glandular tissue, forming a pseudocapsule (prostatic capsule), which is thick, relatively firm, and has a clear boundary with the hypertrophic glandular nodules, making it easy to surgically dissect. The clinically common types of hypertrophic glandular nodules include:
1. Bilateral lobe type: Hypertrophy of the glandular tissue in both lateral lobes protrudes and compresses the urethra centrally. If the hypertrophy of both lateral lobes is symmetrical, the urethral curvature is not obvious, and the main cause of urinary obstruction is the bilateral compression.
2. Median lobe type: Hypertrophy of the median lobe of the prostate protrudes into the bladder from behind the bladder neck, compressing the urethra anteriorly and causing it to bend and elongate, leading to significant urinary obstruction. A posterior prostatic recess forms in the bladder above the hypertrophic gland, and a large amount of residual urine can appear early.
3. Lateral and median lobe type: This type combines the above two conditions, with urinary symptoms appearing earlier and having a more severe impact. Catheter insertion is often more difficult.
4. Lateral, median, and anterior lobe type: Similar to type 3, but with hypertrophy of the anterior lobe, causing the hypertrophic glandular tissue to fuse into a complete ring, including both lateral lobes, the median lobe, and the anterior lobe. However, since the anterior lobe itself is small, the hypertrophic glandular tissue is also limited, and the majority of the mass still comes from the lateral and median lobes.
5. Subcervical lobe type: Hypertrophy of the urethral glands often presents as small nodules scattered around the bladder neck, which can exist alone or in combination with the above types.Histological examination of hypertrophic glandular nodules reveals varying degrees of glandular hyperplasia, fibrous tissue, and muscle tissue proliferation. Glandular hyperplasia is often the main component, with enlarged glands and papillary epithelial hyperplasia protruding into the glandular lumen, but only a slight increase in stromal tissue. In another scenario, the hypertrophic glandular nodules are mainly composed of fibromuscular hyperplasia, resulting in a smaller and harder mass. Based on the proportion of different tissues, they can be classified into fibroadenomatous, fibromyoadenomatous, leiomyomatous, and stromal types.
The primary pathology of BPH is the obstruction caused by the hypertrophic glandular tissue at the bladder neck, leading to urinary obstruction. If the obstruction is not relieved for a long time, it can affect kidney function, leading to adverse outcomes. The mechanism of obstruction in BPH is due to the hypertrophic glandular tissue compressing the urethra at the bladder neck, causing it to bend and elongate, forming a blockage or valve effect that prevents urination. Therefore, the degree of glandular hypertrophy does not directly correlate with the severity of obstruction. A larger hypertrophic lateral lobe may not cause significant obstruction, while a smaller hypertrophic median lobe can cause severe urinary obstruction.
In the initial stage of obstruction, the bladder detrusor muscle undergoes compensatory hypertrophy to increase bladder contraction force and overcome urinary resistance. However, this compensatory ability has its limits. If the obstruction is not relieved for a long time, it will eventually lead to decompensation of the bladder detrusor muscle, bladder enlargement, trabeculation, and the formation of diverticula. These changes affect the ureteral orifice, disrupting its valve function and causing vesicoureteral reflux, leading to ureteral dilation, hydronephrosis, and direct impairment of kidney function, resulting in azotemia. Additionally, due to long-term urinary obstruction, there is often a large amount of residual urine in the bladder, which can lead to stone formation and urinary tract infections. Systemically, prolonged straining during urination can easily lead to complications such as hernias, hemorrhoids, and lung qi swelling.
bubble_chart Clinical Manifestations
As mentioned earlier, the symptoms of prostatic hypertrophy are primarily related to urinary obstruction, which manifest as follows:
1. Frequent and urgent urination: In the early stages of the disease, the increase in the frequency of urination, especially at night, often draws the patient's attention. This is mainly caused by congestion and edema at the bladder neck and residual urine, which reduces the bladder's capacity. When inflammation or accompanying stones are present, urgent and painful urination may occur.
2. Difficulty in urination: Characterized by a slow start to urination, weak urine stream, dribbling, and wetting of pants and shoes, making it inconvenient for the patient to urinate standing up and forcing them to squat. This can lead to segmented urination, where the patient can barely urinate when straining, but the urine flow stops as soon as they relax.
3. Urinary incontinence: The amount of residual urine continues to increase, and when there is a large amount of residual urine, overflow incontinence (pseudo-incontinence) often occurs, with frequent dribbling of urine, causing the patient's pants to be constantly wet, which is very distressing.
4. Acute urinary retention: On the basis of the aforementioned urinary obstruction, acute urinary retention can occur at any time, making it impossible for the patient to urinate, causing severe distending pain, and forcing the patient to seek emergency care. The triggers for acute urinary retention are often changes in weather, catching a cold, fatigue, alcohol consumption, etc. Although the disease itself is not seasonal, the occurrence of urinary retention often forces patients to seek emergency care, especially in the cooler autumn and winter seasons. The above are all symptoms of urinary obstruction. In addition, there may be changes in urine and accompanying symptoms such as:
5. Hematuria: Gross hematuria is uncommon in this disease. In a few cases, due to obstruction at the bladder neck and impaired venous return, varicose veins develop in the bladder, leading to the formation of "bladder hemorrhoids," which can sometimes rupture and cause significant bleeding. In cases accompanied by stone formation or tumor development, gross hematuria is also inevitable.
6. Complications caused by frequent straining during urination: Such as hernia, hemorrhoids, prolapse of the rectum, varicose veins in the lower limbs, lung qi swelling, and other complications can be observed.
7. Advanced stage symptoms: Due to renal impairment and failure, symptoms such as azotemia, acidosis, hypertension, poor appetite, anemia, emaciation, and even heart failure and cerebrovascular disease symptoms can be observed.
8. Examination findings
(1) Patients are generally elderly males, usually over 50 years old.
(2) During physical examination, a distended bladder can be observed in the lower abdomen.
(3) During a digital rectal examination, an enlarged and raised prostate can be palpated, with the central groove disappearing or the sides widening. The distended bladder can often be palpated above the upper edge of the hypertrophic gland.
(4) Signs of complications such as hernia, hemorrhoids, prolapse of the rectum, etc., can also be observed.
For men over the age of 50 with a history of sexually transmitted diseases and urinary disorders, the possibility of prostate hypertrophy should be considered first. Therefore, during the examination, attention should be paid to the following aspects:
1. Abdominal examination: Note the presence of a distended bladder. Patients with prostate hypertrophy often have a large amount of residual urine in the bladder, and a distended bladder can often be palpated during the examination. However, if there is a long history of seasonal diseases, the bladder may be in a state of chronic urinary retention for a long time, and the distended bladder may be flaccid and difficult to detect. In such cases, a percussion diagnostic method can be used to determine the condition.
2. Digital rectal examination: This is an important step in diagnosing this disease. Most cases of prostate hypertrophy can be clearly diagnosed through this examination. Positive findings include an enlarged prostate, protrusion, disappearance of the central groove, widened lateral edges, and a tough and smooth surface. Based on these characteristics, it can be differentiated from prostate cancer, subcutaneous nodes, and stones. However, if the prostate is not enlarged, the possibility of prostate hypertrophy cannot be ruled out based solely on this examination. This is because if only the middle lobe is hypertrophied, the hypertrophied gland may protrude into the bladder, making it impossible to detect through a digital rectal examination. During the digital rectal examination, attention should be paid to the function of the anal sphincter, which can help differentiate from neurogenic bladder urinary disorders.
3. Cystoscopy: Cystoscopy is necessary for some cases because it can confirm whether the prostate is hypertrophied, which lobe is hypertrophied, and the degree of hypertrophy. This examination can also provide information about the condition inside the bladder and exclude other lesions. However, cystoscopy can easily cause injury, bleeding, and infection in patients with prostate hypertrophy, so it should be used with caution. The operation must be careful and meticulous, and close observation is required after the examination.
4. Measurement of residual urine: Measuring residual urine is of great significance for this disease. As mentioned earlier, the degree of gland hypertrophy is not proportional to the severity of the condition, so grading the disease based on the size of the gland has no clinical significance. However, the amount of residual urine can indicate the degree of obstruction and is closely related to the condition. Methods for measuring residual urine include: ① Ultrasound examination: Simple and easy to perform, with minimal burden on the patient, and the results can also provide useful information. ② Catheterization: After the patient urinates on their own, a catheter is immediately inserted to accurately measure the amount of residual urine. A urine sample can also be obtained for culture, and a phenol red test and cystography can be performed. However, there is a risk of traumatic hemorrhage and infection, so it should be performed with caution and strict prevention. If a large amount of residual urine is detected, the catheter should be left in place for drainage. ③ During intravenous pyelography, after the last film is taken with the pressure band removed, the patient is asked to empty the bladder and another film is taken to show the residual urine.
5. Other examinations: In addition to routine hematuria examination, urine culture and renal function tests are also important. If surgical treatment is considered, heart, lung, liver, and vascular examinations, as well as blood generation and transformation tests, should be performed.
bubble_chart Treatment Measures
It can be divided into emergency treatment, non-surgical treatment, and surgical treatment:
(1) Emergency treatment: Patients often come to the hospital due to acute urinary retention, which needs to be resolved promptly to relieve pain and save lives. The usual method is to first use a No. F-14 rubber catheter for catheterization. If the catheter is obstructed, the tip of the catheter can be pushed forward under the lower edge of the hypertrophic gland in the anus with a finger to lift the tip of the catheter, allowing it to be inserted into the bladder. A large amount of retained urine should not be emptied quickly at once; adjust the depth of the catheter, fix it for drainage, and simultaneously start endocrine hormone therapy.
If the catheter cannot be inserted, an emergency suprapubic bladder fistula should be created. This procedure is simple and not burdensome for the patient, and can be performed under local or acupuncture anesthesia. Similarly, in cases of large amounts of retained urine, it should not be emptied quickly. Attention should also be paid to the following two points: a thorough and comprehensive exploration of the bladder's condition, including the degree of prostate hypertrophy, which lobe is hypertrophic, the texture, and any other complications. The findings should be detailed and recorded in the surgical notes to provide necessary guidance for future treatment. Additionally, the fistula drainage tube should be placed at a high position in the bladder, i.e., a high bladder fistula. As for bladder puncture, this method is not used when there are conditions to treat the disease, to avoid other complications and more suffering for the patient. Whether an emergency prostatectomy can be performed to solve the problem of acute urinary retention is generally not recommended. Most patients are elderly, with long-term urinary obstruction and renal function impairment, and often have other systemic diseases. The surgery itself is a major procedure, and the risks and benefits must be weighed carefully. After creating a bladder fistula and resolving the urinary problem, under the condition of sex hormone treatment, a comprehensive examination should be conducted to understand all aspects of the situation before deciding whether and if an intermediate stage [second stage] prostatectomy can be performed.
(2) Non-surgical treatment: This refers to sex hormone therapy. Since the cause of prostate hypertrophy is related to gonadal endocrine disorders, it is believed that gonadal endocrine therapy should yield good results. The situation in this regard is as follows:
① Androgen therapy: From 1935 to 1958, Walther and others recommended androgen therapy for prostate hypertrophy. Later, Menllner pointed out that the effect of androgens mainly lies in increasing the tension of the bladder muscles. Enfedznier's experience summary suggests that androgens have a certain effect on early-stage prostate hypertrophy but are ineffective for advanced-stage patients. Greissman believes that androgens are effective for purely myomatous prostate hypertrophy but not for glandular hypertrophy. Jackot's experience is that it has good effects on very elderly patients aged 76 to 86 and above, but poor effects on patients under 75. In summary, androgen therapy for prostate hypertrophy has many selection conditions and has not been widely promoted.
② Combined application of androgens and estrogens: Using androgens and estrogens in a 3:1 ratio to treat this disease can enhance bladder tension and reduce the prostate. Gloss used testosterone propionate 5-10 mg plus diethylstilbestrol to treat prostate gland hypertrophy, observing significant improvement in 20 cases over three months to four years. Kanfman used testosterone propionate 25 mg plus estrogen 1.25 mg, three times a week for six months, and found that residual urine decreased in 15 out of 28 cases, the gland shrank in 14 cases, and none increased. It seems that the combined application of the two hormones has better effects than using androgens alone.
③ Estrogen Therapy: Extensive clinical experience has proven that the application of estrogen in the treatment of prostatic hypertrophy yields favorable results. In 1959, Cao Chentao from China reported an 80% success rate using estrogen therapy for this condition. Wang Ligeng reported a 75% success rate in 1962. Internationally, Topchan reported in 1951 that 76.2% of 244 cases treated with Synestrol showed good results, and later, 82% of 103 cases treated also showed good results. The dosage of Synestrol was 40-60 mg intramuscularly, with a treatment course of two months. Ende treated 17 cases of prostatic hypertrophy complicated by urinary retention with intravenous Premarin, and all cases were cured, with 16 cases showing no recurrence after more than a year of follow-up. Currently, the use of estrogen in the treatment of prostatic hypertrophy is a widely adopted method.
(3) Surgical Treatment: For patients with a good constitution who can tolerate surgery, surgical treatment is still the best option. Hormonal therapy only offers relative cure, and the chance of recurrence still exists, far from being as thorough and complete as surgical resolution. There are several surgical methods, with the important ones listed below:
① Suprapubic Prostatectomy: This is an ancient surgical method of removing the prostate above the pubic bone. It can be performed in the initial stage [first stage] or divided into the intermediate stage [second stage]. For patients in poor general condition, such as those with severe kidney damage and heart failure, a bladder fistula drainage should be performed first. Surgical treatment should be considered only after kidney function is restored and heart condition improves enough to tolerate surgery. For such patients, whether it is appropriate to use sex hormones in conjunction with bladder fistula drainage, the conclusion is that sex hormone therapy can reduce intraoperative bleeding without creating unfavorable surgical factors. Zhao Yuqi reported in 1966 on the treatment experience of 112 cases, illustrating this issue (Figure 1)
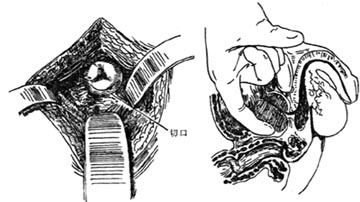
Figure 1 Suprapubic Prostatectomy
② Retropubic Prostatectomy: Introduced by Millin in 1945, this surgical approach is behind the pubic bone and outside the bladder, without the need to open the bladder. The prostate is exposed in the space in front of the bladder behind the pubic symphysis, and the hypertrophic part of the prostate is excised below the internal sphincter plane, then the membrane is sutured. This method is most suitable for the removal of smaller and fibrotic glands.
③ Perineal Prostatectomy: This surgery requires an incision in the perineum to expose the prostate and special urethral traction instruments to better expose the bladder neck to the perineal incision. This method has a deep and narrow operating range and is prone to injure the rectum and internal bladder sphincter, making it a necessary approach for prostate cancer resection.
④ Transurethral Resection of the Prostate: Through electrocautery and scraping with an endoscope, the hypertrophic glands are scraped out piece by piece through the urethra until urination is smooth. This surgery can be repeated multiple times, but it cannot completely remove the hypertrophic glands.
In addition, there are infrapubic prostatectomy and parasacral approach prostatectomy, which have not been widely used. The advantages and disadvantages of the above four prostate surgeries are compared as follows.
Table 1 Comparison of Advantages and Disadvantages of Four Prostate Surgeries
| Surgical Method | Advantages | Disadvantages |
| Suprapubic Prostatectomy | Simple surgical method. Clear exposure of the bladder, allowing a comprehensive understanding of the bladder's condition, and complete removal of hypertrophic glandular tissue. | More bleeding. Long healing time after bladder fistula. Not suitable for cancerous conditions. |
| Retropubic Prostatectomy | Complete removal of hypertrophic tissue. Simple surgical approach, allowing tight suturing and control of bleeding. Faster postoperative recovery. | Poor exposure. Prone to bleeding from the anterior venous plexus. Inability to understand the bladder's condition. Higher incidence of pubic osteitis. |
| Perineal Prostatectomy | Complete removal of hypertrophic tissue. Early tumors can also be removed. External urethral membrane can be sutured. Low drainage. | Risk of injury to the rectum and external sphincter. Poor bladder exposure. |
| Transurethral Resection of the Prostate (TURP) | Minimal patient burden, low mortality rate. Can be performed in stages and multiple times. Allows observation of bladder conditions. | Requires special instruments. Requires specialized operative skills. Can cause hemolytic reactions. |
Hernia; hemorrhoids; prolapse of the rectum; varicose veins in the lower limbs; lung qi swelling
This disease should be differentiated from prostate cancer, prostate subcutaneous node, prostate stones, prostate cysts, bladder neck contracture (Marion's disease), hypertrophy of the interureteric ridge, neurogenic bladder, bladder tumors, stones, foreign bodies, etc. The aforementioned diseases can mostly be differentiated through physical examination, laboratory tests, digital rectal examination, and cystoscopy. Only in atypical cases of prostate cancer, it is difficult to reach a conclusion based on the aforementioned examination methods. The following methods can be used to assist in differential diagnosis:
1. Serum acid phosphatase determination: Prostate tissue contains a particularly high level of acid phosphatase, which increases when cancerous. This principle is utilized in this test. The normal value of serum acid phosphatase is 1-5 units according to King-Armsstrong and 0.5-2 units according to Bodansky. Since 1950, new testing methods have established its value at 0.7 K-A units. More than half of prostate cancer patients have values higher than normal. Note that false positives may occur after the application of testosterone or prostate massage.
2. Serum alkaline phosphatase determination: When there is bone metastasis, serum alkaline phosphatase is elevated. The normal value is 2-4.5 units according to Bodahsky and 8-14 units according to King-Armstrong, but false positives should be noted.
3. Prostate biopsy: Transperineal or transrectal prostate needle biopsy can be performed.
4. Seminal vesicle and ejaculatory duct radiography: Prostate hypertrophy only shows symmetrical enlargement with smooth edges; prostate cancer shows stenosis, irregularity, uneven edges, or defects.




