| disease | Atlas Fracture |
Atlas fracture dislocation is one of the more common upper cervical spine injuries, accounting for approximately 50% of cases. Clinically observed cases of atlas fracture dislocation present with varying degrees of neurological symptoms—some result in immediate death, while others involve severe conditions accompanied by varying levels of brainstem and high spinal cord injuries. These may manifest as cranial nerve paralysis, quadriplegia or incomplete paralysis, and respiratory dysfunction, often requiring immediate assisted ventilation. In some cases, symptoms may be mild, limited to occipital neck pain and restricted movement, with minimal neurological signs. However, such patients still carry potential risks and should be given high priority and appropriate treatment.
bubble_chart Pathogenesis
This condition occurs when an object falling from a height impacts the top of the head, or when a person falls from a height and the top of the head strikes the ground vertically. The atlas connects the occipital bone and other cervical vertebrae. It is an atypical vertebra with an elliptical ring-like shape, lacking a vertebral body. The ring thickens on both sides, forming the lateral masses, whose upper and lower surfaces are articular facets inclined inward and forward. The anterior and posterior arches extending from the lateral masses are the weakest parts of the atlas and the most common sites of fracture. When force and counterforce accumulate and act on the atlas, due to the inward inclination of its articular facets, the resultant force subjects the lateral masses to centrifugal stress, leading to fracture at the weakest points where the anterior and posterior arches connect to the lateral masses. This type of fracture is also called a Jefferson fracture. Its characteristic feature is that the atlas fracture occurs at four corresponding points, resulting in four fracture segments: the two lateral masses and the anterior and posterior arches (Figures 1 and 2). If the direction of the force is not aligned properly, acting only on one side of the head or when the head is tilted to one side during impact, it may cause a unilateral arch fracture, and occasionally a lateral mass fracture.
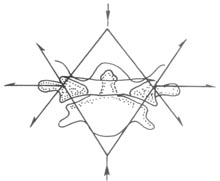
Figure 1: Mechanism of atlas fracture
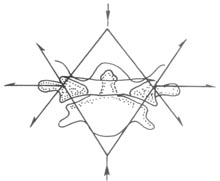
Figure 2: Jefferson fracture
Four-part fracture and displacement of the atlas arches
Force acts downward from the occipital condyles, transmitting to the lateral masses of the atlas
Classification
Based on the fracture location and displacement, atlas fractures are divided into three types:
Type I: Fracture of the posterior arch of the atlas, caused by hyperextension and axial force between the occipital condyles and the spinous process of the axis, resulting in compressive forces. It may also occur concurrently with fractures of the second cervical vertebra or the odontoid process.
Type II: Fracture of the lateral mass of the atlas, usually unilateral, with the fracture line passing through the anterior and posterior parts of the articular facet, sometimes involving the vertebral artery foramen.
Type III: Bilateral fractures of the anterior and posterior arches of the atlas, i.e., fractures occurring in both the anterior and posterior parts of the lateral masses, also known as a Jefferson fracture, typically caused by pure vertical force.
bubble_chart Clinical Manifestations
Neck pain and stiffness, patients often hold their heads with both hands to avoid movement. If the second cervical nerve (greater occipital nerve) is affected, patients may experience occipital pain, neck muscle spasms, and restricted neck movement. If accompanied by spinal cord injury, there may be loss of motor and sensory functions. Severe injury can lead to paralysis or even immediate death.
bubble_chart Auxiliary Examination
An open-mouth X-ray and a lateral X-ray should be taken. On the open-mouth X-ray, measurements should be made to assess the compression fracture of the atlas and atlantoaxial instability. Normally, the outer edges of the lateral masses of the atlas align with the outer edges of the articular processes of the axis. In cases of atlas fracture, the bilateral lateral masses shift outward, with their outer edges extending beyond those of the articular processes of the axis. The distance of the lateral mass displacement is measured; if the sum of both sides exceeds 6.9 mm, it indicates a rupture of the transverse ligament of the atlas, leading to atlantoaxial instability. On the lateral X-ray, a double fracture of the posterior arch of the atlas may be observed, with the fracture line passing through the vertebral artery groove.
The distance between the bilateral lateral masses of the atlas and the odontoid process should be equal and symmetrical. The normal atlantodental interval, measured between the posterior edge of the anterior arch of the atlas and the anterior edge of the odontoid process, is 3 mm. This measurement is a relatively constant landmark within 3 mm. If the atlantodental interval exceeds the normal range, it may indicate an atlas fracture combined with a transverse ligament rupture.To evaluate subtle structural changes in the atlantoaxial region, tomography and CT scans are recommended. These imaging modalities often reveal the separation of the atlas burst fracture and are beneficial for determining the degree of stability. Additionally, attention should be paid to avulsion fractures of the medial edges of the atlas lateral masses, as they are indicative of transverse ligament tears and suggest fracture instability.
Non-surgical treatment
Hyperextension reduction, or skull traction for 3 weeks with a traction weight of 3–5 kg. After reduction, perform head-neck-thorax gypsum external fixation, or connect the traction device to a gypsum vest and fix for 3–5 months. Surgery is generally not required.
Surgical treatment
To achieve permanent stability of the occipitoatlantoaxial joint, some authors actively advocate surgical treatment. There are two surgical methods:
Atlantoaxial fusion: Includes the traditional Gallie procedure and the more recent Brooks and modified Brooks techniques. Atlantoaxial fusion cannot be used for fresh fractures and must be performed only after the posterior arch and both lateral masses have achieved solid bony union. The method is as follows:
1. Incision: Starting 2.0 cm below the occipital bone protuberance, follow the midline through the hairline to the C4 spinous process. Incise the skin and subcutaneous tissue, and achieve hemostasis with electrocautery.2. Exposure of the C2 spinous process and lamina: Perform a midline subperiosteal dissection to the base of the nuchal ligament. Detach the muscle insertion from one side of the C2–C3 spinous process, and use a periosteal elevator to bluntly dissect subperiosteally from the lateral side of the spinous process and lamina. Pack with dry gauze for hemostasis, retract the nuchal ligament to the opposite side, and repeat the dissection. Fix with self-retaining retractors to fully expose the C2–C3 spinous processes and laminae.
3. Exposure of the C1 posterior arch: Detach the muscle attachments from both sides of the C2 lamina, and incise the muscle layers and loose connective tissue along the midline at the occipitocervical junction. The C1 posterior arch tubercle can be palpated with a finger between the posterior edge of the occipital bone foramen magnum and the C2 lamina. Incise the occipitoatlantal ligament and fibrous tissue, and carefully dissect with a small sharp elevator. Incise the periosteum of the posterior arch and perform subperiosteal dissection, ensuring the dissection does not exceed 1.5 cm lateral to the posterior tubercle to avoid injury to the vertebral artery (i.e., the exposed segment).
4. Bone grafting and wire fixation:
(1) Gallie method and modifications: For C1 posterior arch dissection, use a long-handled scalpel to carefully incise the adhesion between the superior edge of the exposed C1 posterior arch and the posterior atlanto-occipital membrane. Insert a nerve dissector into the space and fully dissect along the deep surface of the posterior arch.
After complete mobilization of the C1 posterior arch, use a rongeur to remove the cortical bone from its inferior edge to create a bony surface. Similarly, prepare a rough bony surface on the superior edge of C2, including the lamina and spinous process.
Trim autologous iliac bone into two wedge-shaped grafts, with cancellous bone on the wedge surfaces and cortical bone on the base.
Use high-quality medium-gauge wire. Pass a double-stranded wire from the deep surface of one side of the C1 posterior arch from top to bottom using a hook-shaped conductor or aneurysm needle, then loop and tighten the wire ends above the posterior arch. Repeat the same process on the other side. Embed the two wedge-shaped grafts between C1 and C2 bilaterally. Pass the wires fixed to the C1 posterior arch over the surface of the grafts, then through the C2 spinous process, and tighten and tie.
In recent years, various modifications have been developed, such as the Fielding method, where a large bone block is embedded between C1 and C2, or bone grafting is performed between the C1 posterior arch and C2 lamina, followed by wire fixation. Most of these techniques are based on the Gallie method.
(2) Brooks method and modifications: Unlike the Gallie method, the wire is passed through the C1 posterior arch and then through the inferior aspect of the C2 lamina. During bone grafting, the cancellous surface of the graft faces the C1 posterior arch and C2 lamina. A notch is made on the inferior surface of the graft to fit snugly against the base of the C2 arch. The wire is then tightened and tied. Depending on the Brooks principle, grafts of different shapes and wire fixation methods may be used.
Occipitocervical fusion: There are various methods for occipitocervical fusion. Here, we describe only the occipital bone flap turnover and autologous iliac bone grafting method.
The patient is placed in the prone position on a Gypsum bed. Local anesthesia is administered. A posterior midline incision is made from the occipital protuberance to the 4th cervical vertebra. The posterior arch of the atlas and the lamina of the axis are exposed. Starting 6 cm above the posterior edge of the foramen magnum, bilateral sharp osteotomes are used to chisel two bone flaps, each 1 cm to 1.2 cm wide, from below the occipital protuberance. The depth is limited to the outer table of the occipital bone, extending downward to 2 cm above the posterior edge of the foramen magnum. The bone flaps are then folded downward to cover the laminae of C1–C2, ensuring the hinge remains intact. Autologous iliac bone grafts are placed over the superficial surface of the bone flaps, extending from the hinge area above to the laminae and spinous processes of C2 or C3 below. The wound is closed in layers. Postoperatively, the patient remains in the Gypsum bed but can turn over. After one month, a head-neck-thorax Gypsum cast can be applied for fixation.




