| disease | Submandibular Space Infection |
Submandibular space infection refers to an acute suppurative infection in the submandibular space, with main clinical manifestations including fullness in the submandibular region, lymphadenopathy, and tenderness.
bubble_chart Etiology
The submandibular space is located within the submandibular triangle and contains the submandibular gland, submandibular lymph nodes, as well as the passage of the external maxillary artery, facial vein, lingual nerve, and hypoglossal nerve. This space communicates superiorly with the sublingual space along the posterior border of the mylohyoid muscle; it is adjacent posteromedially to the pterygomandibular space and parapharyngeal space; anteriorly, it connects with the submental space; and inferiorly, it links with the carotid triangle and anterior cervical space via loose connective tissue. Consequently, infections in the submandibular space can spread to become multi-space infections of the floor of the mouth (Figure 1).
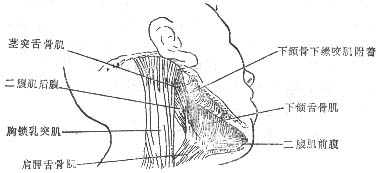
Figure 1 Anatomical location of the submandibular space
It commonly arises from the spread of odontogenic infections such as pericoronitis of the mandibular wisdom tooth, periapical inflammation of mandibular posterior teeth, and alveolar abscesses. Secondary causes include the spread of submandibular lymphadenitis. Suppurative submandibular sialadenitis may also occasionally lead to submandibular space infection.
bubble_chart Clinical Manifestations
Most submandibular space infections initially manifest as submandibular lymphadenitis, clinically presenting as fullness in the submandibular region, with palpable lymph node enlargement and tenderness upon examination. Suppurative submandibular lymphadenitis can spread beyond the nodes, leading to cellulitis. Submandibular space cellulitis clinically presents as swelling in the submandibular triangle, obliteration of the mandibular lower border contour, tense and tender skin, and pitting edema upon pressure. After abscess formation, the central area exhibits skin congestion and palpable fluctuation. Due to the continuity between the submandibular space and the sublingual space, infection can easily spread to the sublingual space (Figure 2), which may be accompanied by swelling in the posterior floor of the mouth, pain during tongue movement, and swallowing discomfort.
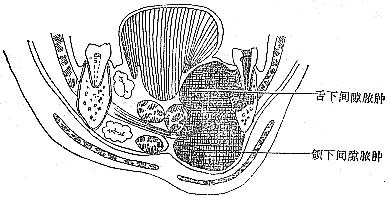
Figure 2 Anatomical relationship of submandibular space abscess causing sublingual space abscess
Submandibular space infections should be differentiated from suppurative lymphadenitis and obstructive sialadenitis of the submandibular gland caused by duct obstruction.
1. Medical History Adults often have a history of suppurative periapical periodontitis in mandibular molars or pericoronitis of mandibular wisdom teeth. In infants and children, a history of submandibular lymphadenitis secondary to upper respiratory tract infections can usually be elicited.
2. Clinical Manifestations Inflammatory redness, swelling, and tenderness in the submandibular triangle are observed. In the early stage, an inflammatory infiltrating mass with tenderness is present. During the suppurative phase, throbbing pain, fluctuance, and skin erythema occur. Pus is easily aspirated upon puncture. Patients exhibit systemic symptoms such as varying degrees of fever and leukocytosis.
3. Differential Diagnosis Acute suppurative submandibular sialadenitis often presents as an acute exacerbation of chronic submandibular sialadenitis. It shares acute inflammatory signs such as redness, swelling, and tenderness in the submandibular triangle, along with fever and leukocytosis. However, submandibular abscess formation is rare. Additionally, redness and swelling are observed at the sublingual caruncle and the orifice of the submandibular duct on the affected side, with purulent discharge from the duct upon submandibular pressure. X-ray occlusal films of the mouth floor often reveal calculi in the submandibular duct.
bubble_chart Treatment Measures
When an abscess forms in the submandibular space, the affected area is usually extensive and the abscess cavity is large. However, if it is cellulitis caused by lymphadenitis, the abscess may be confined to one or several lymph nodes. In such cases, incision and drainage must involve separating the abscessed lymph node's capsule to achieve the desired outcome.





