| disease | High-arched Foot |
High-arched foot is a relatively common foot deformity in children, often caused by neuromuscular diseases that result in a fixed metatarsal flexion of the forefoot, thereby increasing the longitudinal arch of the foot. It is sometimes accompanied by hindfoot varus deformity. In rare cases where the cause is unknown, it may be referred to as idiopathic high-arched foot.
bubble_chart Etiology
The etiology is very complex, with approximately 80% of cases being neuromuscular diseases. Dynamic factors leading to the lowering of the arch include weakened strength of the tibialis anterior muscle and/or the triceps surae muscle, as well as contracture of the intrinsic muscles on the medial side of the metatarsus, resulting in an increased longitudinal arch of the foot. These neuromuscular diseases can occur at different levels, including the pyramidal system of the brain, corticospinal tracts, anterior horn cells of the spinal cord, peripheral nerves, and muscles. Common diseases include poliomyelitis, cerebral palsy, myelomeningocele, and neural tube defects. Other less common diseases include diastematomyelia, tethered cord syndrome, and Charcot-Marie-Tooth disease.
Some cases have a clear family history without evidence of neuromuscular pathology, possibly due to congenital sexually transmitted disease, or referred to as idiopathic pes cavus.
bubble_chart Clinical Manifestations
According to the degree of arch elevation and whether it is accompanied by other deformities of the foot, high-arched feet are usually divided into four types.
1. Simple high-arched foot: Mainly characterized by a fixed metatarsal flexion deformity in the forefoot, with the first and fifth metatarsals bearing weight evenly. The medial and lateral longitudinal arches are uniformly elevated, and the heel remains in a neutral position or has grade I eversion.
2. Inverted high-arched foot: This type involves only the medial column of the forefoot, i.e., the first and second metatarsals, with a metatarsal flexion deformity that elevates the medial longitudinal arch. The lateral longitudinal arch remains normal. When not bearing weight, the fifth metatarsal can easily be raised to a neutral position, while the first metatarsal, due to fixed metatarsal flexion, cannot be passively dorsiflexed to a neutral position and has a 20-30° internal rotation deformity. In the initial stage, the hindfoot is mostly normal. When standing and walking, the pressure on the first metatarsal head significantly increases. To reduce the pressure on the first metatarsal head, patients often adopt an inverted foot posture for weight-bearing. In the advanced stage, a fixed hindfoot inversion deformity appears. Patients often have claw toes, with the first metatarsal head protruding towards the sole, thickening of the soft tissue in the weight-bearing area of the sole, callus formation, and pain.3. Calcaneal high-arched foot: Commonly seen in poliomyelitis and spinal meningocele. It is mainly caused by paralysis of the triceps surae muscle, characterized by the calcaneus being in a dorsiflexed state and the forefoot fixed in a metatarsal flexion position (Figure 1).
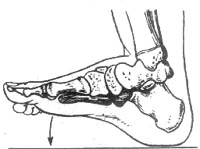
Figure 1: Calcaneal high-arched foot
4. Metatarsal flexion type high-arched foot: Often secondary to surgical treatment of congenital equinovarus. In addition to the fixed metatarsal flexion deformity in the forefoot, the hindfoot and ankle joint also exhibit significant metatarsal flexion deformity (Figure 2). The clinical manifestations of various types of high-arched feet are not entirely consistent, but all have a fixed metatarsal flexion deformity in the forefoot. The toes are mostly normal in the early stages, but as the disease progresses, the toes gradually retract, the interphalangeal joints flex, the metatarsophalangeal joints hyperextend, presenting as claw toe deformity. In severe cases, the toes cannot touch the ground. Due to the dorsiflexion deformity of the metatarsophalangeal joint causing semi-dislocation, the base of the proximal phalanx presses on the dorsal side of the metatarsal head, exacerbating the metatarsal flexion deformity, leading to thickening of the skin at the weight-bearing area, callus formation, and even ulceration.

Figure 2: Metatarsal flexion type high-arched foot
X-ray examination should include anteroposterior and lateral views of the foot under weight-bearing conditions. In a normal foot, the distal and proximal joint surfaces of the first cuneiform are parallel, but in a high-arched foot, due to the metatarsal flexion deformity in the forefoot, often occurring at the first cuneometatarsal joint, the parallel lines of the distal and proximal joint surfaces converge on the metatarsal side. M'eary measures the angle between the axis of the talus and the axis of the first metatarsal; in a normal arch, the two lines are continuous. If an angle can be measured, it indicates an elevated arch (Figure 3).
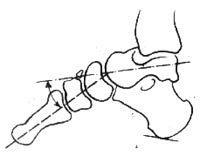
Figure 3: Increased M'eary angle indicating forefoot metatarsal flexion deformity
Hibbs measures the angle between the axis of the calcaneus and the axis of the first metatarsal, with a normal value of 150-175°. In high-arched foot deformity, this angle decreases (Figure 4). Additionally, the calcaneal-talar angle measured on the anteroposterior view, if less than 20°, indicates a hindfoot inversion deformity.
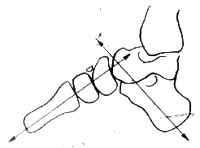
Figure 4: Increased Hibbs angle indicating calcaneal dorsiflexion deformity
bubble_chart Treatment Measures
Early-stage mild pes cavus can be treated by passively stretching the contracted plantar fascia and shortened intrinsic muscles of the foot. To alleviate pressure on the metatarsal bones and ensure even weight distribution, a 1cm thick felt pad can be added inside the shoe at the position corresponding to the metatarsal bones, and the outer rear part of the shoe sole can be thickened by 0.3 to 0.5cm to reduce the tendency of the hindfoot to invert during walking. However, these measures can only alleviate symptoms; they cannot correct the pes cavus deformity nor prevent its progression.
When pes cavus hinders weight-bearing, walking, or wearing shoes, or when it progressively worsens, surgical treatment should be considered. Surgical methods can be divided into soft tissue release and bony procedures. The choice of surgical method generally depends on factors such as the patient's age, type and severity of the deformity, and the status of the underlying disease. In principle, soft tissue surgery is performed first, such as releasing the soft tissues on the lateral side of the metatarsus, transferring the tibialis anterior and posterior tendons, and relocating the extensor digitorum longus. If soft tissue surgery fails to correct the deformity, or if older children have a fixed pes cavus deformity, bony corrective surgery may be chosen.Soft tissue release on the lateral side of the metatarsus is a traditional method. A longitudinal incision is made along the posterior inner edge of the foot to expose the lateral soft tissues of the metatarsus. The plantar fascia and long plantar ligament are first severed, followed by the detachment of the flexor digitorum brevis, flexor hallucis brevis, and flexor digiti minimi from their origins on the calcaneus and pushing them distally. If complete release is needed, the bifurcate ligament can be severed, and the lateral part of the joint capsules of the first to third metatarsal tarsal joints can be incised, along with the expansion of the tibialis posterior tendon that inserts into the metatarsal bones and cuneiform bones. Postoperatively, a series of corrective plaster casts are applied for 8 weeks.
Bony corrective surgeries include open wedge osteotomy of the first cuneiform, dorsal wedge or V-shaped osteotomy of the tarsal bones, and posterior displacement osteotomy of the calcaneus. Dorsal V-shaped osteotomy of the tarsal bones has several advantages: it does not injure the tarsal epiphysis, making it suitable for children over 6 years old; it does not shorten the foot; and it can correct forefoot adduction and internal rotation deformities. The key surgical steps are: ① A transverse or longitudinal dorsal foot incision is made to expose the tarsal bones outside the periosteum; ② A V-shaped osteotomy line is designed at the apex of the foot arch, usually located at the center of the navicular bone, with the medial limb extending obliquely from the navicular to the medial cortex of the first cuneiform; ③ After completing the osteotomy, the surgeon pulls the forefoot distally, elevates it, and presses down on the distal osteotomy end. If there is internal rotation or adduction deformity, the forefoot can be externally rotated and abducted to correct it. A Kirschner wire is then inserted from the medial side of the first metatarsal, passing through the osteotomy line to the lateral part of the calcaneus. Postoperatively, a lower leg plaster cast is applied for six weeks. After removing the plaster cast, the Kirschner wire is extracted, and X-rays are taken to assess the healing of the osteotomy. If healing is confirmed, weight-bearing walking can gradually begin.
Based on the child's abnormal gait, increased longitudinal arch of the foot with claw toe deformity, and X-ray findings of an increased Meary's angle and decreased Hibbs angle, a diagnosis of pes cavus can be made. However, pes cavus is often a deformity caused by neuromuscular diseases, and further investigations should be conducted to identify the primary disease or underlying causes, such as electromyography, cranial or spinal CT, or MRI. Identifying the cause is crucial for determining the prognosis.




