| disease | Furuncles and Carbuncles of the Face |
| alias | Furuncle and Carbuncle |
Facial skin is one of the areas richest in hair follicles, sebaceous glands, and sweat glands in the human body. It is also an exposed part, frequently coming into contact with external dust, dirt, and bacteria, making it prone to damage. The acute suppurative inflammation of hair follicles and their appendages caused by this is called a furuncle, with the lesion confined to the superficial layers of the skin. When multiple adjacent hair follicles and their appendages simultaneously develop acute suppurative inflammation, it is called a carbuncle. If the lesion extends to the deep dermal tissue between hair follicles, it can spread along the superficial fascia, affecting the subcutaneous fat layer, leading to a larger area of inflammatory infiltration or tissue necrosis.
bubble_chart Etiology
The main pathogen of facial boils and carbuncles is Staphylococcus aureus. Normal hair follicles and their appendages often harbor bacteria, but inflammation only occurs when local predisposing factors or systemic resistance declines. Local factors primarily include unclean skin or facial injuries caused by shaving and other reasons, which can serve as triggers. Patients with systemic exhaustion, wasting diseases, or diabetes are also prone to developing boils and carbuncles.
bubble_chart Clinical Manifestations
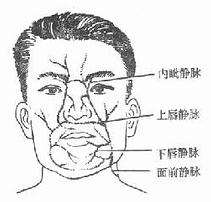
At the initial stage, a boil appears as a small, red, swollen, and painful hard nodule on the skin, forming a conical protrusion with tenderness. Soon after, a yellow-white pus head emerges at the top of the nodule, surrounded by a red, hard disk. The patient may experience localized itching, a burning sensation, and throbbing pain. Later, the pus head ruptures, discharging a small amount of pus, which reduces the pain. Alternatively, a pus plug may form at the top, separating and falling off from the surrounding tissue, leading to gradual resolution of inflammation and spontaneous healing of the wound. During the course of the disease, aside from possible swelling of the draining lymph nodes, there are generally no significant systemic symptoms. If the boil is improperly managed—such as through scratching, squeezing to expel pus, hot compresses, chemical cauterization, or inappropriate incisions—the inflammation may spread. Boils located on the upper or lower lip or nose, due to their position in the facial "danger triangle," can suddenly worsen, with increased redness, swelling, and pain, potentially leading to cellulitis or progression to a carbuncle. In severe cases, complications such as cavernous sinus thrombosis, sepsis, or pyemia may occur.
|
|
|
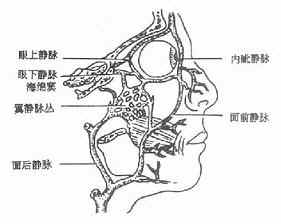
Figure 1: Veins of the facial "danger triangle" | Figure 2: Communication between facial veins and the cavernous sinus |
Carbuncles commonly occur on the lips (lip carbuncle), more frequently on the upper lip than the lower lip, and more often in males than females. The extent of infection and depth of tissue necrosis are more severe than in boils, accompanied by intense pain. When multiple hair follicles, sebaceous glands, and surrounding tissues undergo acute inflammation and necrosis, a rapidly expanding purplish-red inflammatory infiltrate may form. The infection can spread to the subcutaneous fascial layer and muscle tissue. In the initial stage [first stage], surrounding tissues may also necrotize, and after the necrotic tissue dissolves and is expelled, multiple honeycomb-like cavities may form. Subsequently, the skin, mucous membranes, or subcutaneous tissues between these cavities may also necrotize, causing the upper layer of the affected area to appear purplish-red, while the surrounding and deeper tissues exhibit infiltrative edema.
Patients with lip carbuncles experience extreme lip swelling, pain, and restricted mouth opening, leading to difficulties in eating and speaking. Regional lymph nodes may become enlarged and tender. Systemic toxic symptoms are pronounced, including fear of cold, high fever, headache, loss of appetite, elevated white blood cell count, and increased neutrophil ratio. Lip carbuncles are more likely than boils to be complicated by intracranial cavernous sinus thrombosis, sepsis, pyemia, toxic shock, and electrolyte imbalances, resulting in a higher mortality rate.
bubble_chart Treatment Measures
The treatment of facial boils and carbuncles should combine local and systemic therapy. In the early stages of inflammation, when there are no significant systemic symptoms, local treatment should be the primary approach, supplemented with necessary medication.
Local treatment should be conservative to avoid injury. Squeezing, pricking, hot compresses, or cauterization with phenol or silver nitrate are strictly prohibited to prevent the spread of infection. For lip carbuncles, lip movements such as speaking and chewing should also be restricted. Feeding can be done via tube or nasogastric liquid diet.At the onset of a boil, 2% iodine tincture can be applied locally once daily while maintaining local cleanliness. For carbuncles, local treatment with hypertonic saline or saline gauze containing antibiotics for continuous wet compresses can promote early localization, softening, and rupture of the carbuncle. Only when acute inflammation is under control, the local swelling is confined, and a clear subcutaneous abscess has formed without rupture for an extended period, may a conservative incision be considered at the center of the abscess where the skin has thinned to drain the pus. The abscess cavity must not be separated. After rupture or incision and drainage, local hypertonic saline gauze should continue to be used for wet compresses to effectively draw out pus; however, soiled saline gauze should be promptly replaced. Wet compresses should generally continue until the pus disappears and the wound begins to heal. Stopping compresses too early may lead to recurrence or worsening due to pus blockage. Occasionally, if pus plugs are difficult to expel, tweezers may be gently used to assist removal; however, unseparated pus plugs or necrotic tissue must not be forcibly pulled to prevent tearing and spreading.
Patients with facial boils accompanied by local cellulitis or facial carbuncles should receive systemic antibiotics. It is best to collect pus from the abscess head for bacterial culture and drug sensitivity testing to guide appropriate antibiotic selection. For suspected sepsis, repeated blood bacterial cultures should be performed to guide medication choices. If the causative bacteria cannot be immediately identified, drugs sensitive to Staphylococcus aureus, such as penicillin, new-generation penicillins, cephalosporins, or erythromycin, may be temporarily used. Broad-spectrum antibiotics can also be administered. Combination therapy may yield better results.
Critically ill patients should receive enhanced systemic supportive care, including bed rest, improved nutrition, intravenous fluids, or small blood transfusions. In cases of toxic shock, comprehensive measures should be actively implemented to quickly correct hypotension caused by circulatory failure. For patients who are unconscious or have severe pulmonary complications, with excessive respiratory secretions and poor cough reflexes, a tracheostomy may be considered to facilitate secretion suction and improve hypoxia.When systemic complications arise clinically, collaboration with other relevant departments is necessary for joint emergency treatment.
In oral and maxillofacial infections, facial boils and carbuncles are most prone to systemic complications. This is due to the following factors: the pathogenic bacteria of boils and carbuncles are highly virulent; the veins in the "danger triangle" of the upper lip and nose often lack valves; and the physiological movements of facial expression muscles and lips can easily spread the infection.
When the infection invades the facial vein, causing phlebitis and thrombosis, venous return is obstructed, leading to widespread facial edema and pain. If the infection spreads retrograde along the valveless facial vein, it can cause cavernous sinus thrombophlebitis. Symptoms include eyelid edema on the affected side, proptosis, increased intraocular pressure, restricted movement, reduced vision, photophobia, tearing, and subconjunctival edema or static blood. Systemic manifestations include high fever, headache, and even unconsciousness. If meningitis or brain abscess occurs simultaneously, severe headache, nausea, vomiting, neck stiffness, elevated blood pressure, deep breathing, convulsions, unconsciousness, and other signs of meningeal irritation, intracranial hypertension, and space-occupying lesions may appear. Bacteria spreading through the bloodstream can cause sepsis or pyemia. High fever (often above 39°C) may be sustained or remittent. The patient may experience dysphoria, delirium, apathy, sluggish reactions, drowsiness, or even unconsciousness. Skin may show petechiae or small pustules. Total white blood cell count and neutrophil ratio are significantly elevated. In cases of toxic shock, blood pressure drops and the pulse becomes rapid and thready. Without timely and proper treatment, death may occur. In pyemia, metastatic abscesses may also appear in vital organs (such as the liver and lungs) as well as the trunk and limbs.