| disease | Ossification of the Posterior Longitudinal Ligament of the Cervical Spine |
| alias | Ligamentous Ossifying Spondylitis |
Ossification of the posterior longitudinal ligament of the cervical spine (OPLL) refers to a condition where the ossification of the posterior longitudinal ligament in the cervical spine compresses the spinal cord and nerve roots, leading to sensory and motor disturbances in the limbs and autonomic nervous system dysfunction. In 1983, Key first reported the phenomenon of spinal ligament ossification, naming it "ossifying spinal ligamentitis." In 1960, Japanese researchers discovered during autopsies that ossification of the posterior longitudinal ligament in the cervical spine caused spinal cord compression. In 1964, Terayama named this pathological change "ossification of the posterior longitudinal ligament of the cervical spine (OPLL)," which was widely accepted and became a distinct clinical entity.
bubble_chart Etiology
The posterior longitudinal ligament is located within the spinal canal, closely adhering to the posterior aspect of the vertebral bodies, extending from the second cervical vertebra to the sacrum. The ligament is wider at the top and narrower at the bottom, being thicker in the thoracic region compared to the cervical and lumbar regions. At the level of the intervertebral discs and the upper and lower edges of the vertebral bodies, the ligament is in close contact with the bone. In the middle part of the vertebral body, the ligament is separated from the bone by the basivertebral venous plexus. The posterior longitudinal ligament is denser and stronger than the anterior longitudinal ligament and is usually divided into deep and superficial layers. The superficial layer is continuously distributed over 3 or 4 vertebral segments, while the deep layer is only present between adjacent vertebral bodies. Ossification of the posterior longitudinal ligament is a disease of the elderly, most commonly occurring between the ages of 50 and 60. In patients over 60 years old, the incidence can be as high as 20%, and it accounts for about 1-3% of general adult outpatient visits.
The exact cause of ossification of the posterior longitudinal ligament is still unclear. Routine laboratory tests, such as blood count, serum protein, and blood sugar, are usually within normal ranges. However, among these patients, 12.6% have diabetes, and the proportion of those with latent diabetes is even higher, indicating a relatively close relationship between glucose metabolism and the tendency for ligament ossification. This also partially explains why the incidence of ligament ossification is particularly high among ethnic groups in East Asia where rice is the staple food.Since patients with ligament ossification often also have hypoparathyroidism or familial hypophosphatemic rickets, it suggests that abnormal calcium and phosphorus metabolism can lead to ligament ossification. Although blood chemistry tests are often normal, calcium intake tests show that patients with ossification of the posterior longitudinal ligament tend to have reduced intestinal calcium absorption.
Trauma is closely related to the onset of this disease. Due to the close relationship between the posterior longitudinal ligament and the venous plexus at the posterior edge of the vertebral body, when trauma or posterior disc herniation occurs, the veins are prone to injury and bleeding, which can enter the posterior longitudinal ligament and cause calcification and ossification.
Additionally, patients with ossification of the posterior longitudinal ligament also tend to have systemic hyperplasia. Besides being associated with spinal hyperostosis and ankylosing spondylitis, they often also have ossification of the anterior longitudinal ligament and ligamentum flavum. Therefore, some believe that ossification of the posterior longitudinal ligament may be a local manifestation of systemic hyperostosis and ligament ossification.
bubble_chart Pathological ChangesPosterior longitudinal ligament ossification grows along the longitudinal axis while simultaneously expanding horizontally, forming a space-occupying lesion within the spinal canal, leading to a reduction in spinal canal volume and spinal stenosis. This causes compression of the spinal cord and nerve roots, with the spinal cord being squeezed into a crescent shape and pushed toward the posterior wall of the spinal canal. The posterior wall of the ossified mass exhibits a wavy change.
The ossified mass is mainly composed of lamellar bone, with fibrous tissue, fibrocartilage, and calcified cartilage sequentially present from the posterior edge of the vertebral body to the lamellar bone. The ossified lesion adheres to the dura mater, and as the degree of compression increases, the dura mater becomes thinner or even disappears. In some cases, the dura mater may also ossify.
Due to the continuous enlargement of the ossified mass, the spinal cord undergoes severe deformation under compression, with hyperemia and edema in the neural tissue, a reduction in the number of anterior horn cells, and a decrease in their size. There is extensive demyelination in the white matter of the spinal cord.
bubble_chart Clinical Manifestations
The clinical manifestations of patients with ossification of the posterior longitudinal ligament (OPLL) of the cervical spine are very similar to those of adjacent spinal canal stenosis and cervical spondylosis. These manifestations can include symptoms of spinal cord compression as well as nerve root compression. Patients may experience neck pain or discomfort, gradually developing sensory and motor dysfunction in the limbs, as well as bladder and rectal dysfunction, which progressively worsen. Physical examination may reveal sensory disturbances in the limbs and trunk, hyperreflexia, and often pathological reflexes in both the upper and lower limbs. The majority of patients have no obvious precipitating factors at the onset, with a slow progression of symptoms. However, nearly one-fifth of patients may experience sudden onset or exacerbation of existing symptoms, or even quadriplegia, due to varying degrees of trauma, falls while walking, or sudden backward movement of the head and neck while riding in a vehicle.
The causes of spinal cord symptoms include: (1) gradual growth and thickening of the ossified posterior longitudinal ligament, directly compressing the anterior spinal cord (anterior spinothalamic tract and anterior corticospinal tract); (2) as the spinal cord is compressed and gradually shifts posteriorly, it is also subjected to continuous traction from the denticulate ligaments on both sides. This traction can create stress zones in the spinal cord, concentrated near the attachment sites of the denticulate ligaments (lateral corticospinal tract); (3) when the patient's neck suddenly extends backward, the thickened ligamentum flavum bulges forward, compressing the spinal cord. This results in the spinal cord being pinched between the anterior ossified posterior longitudinal ligament and the posterior bulging ligamentum flavum, leading to central cord injury syndrome and quadriplegia, with symptoms in the upper limbs being significantly more severe than those in the lower limbs; (4) when the ossified mass protrudes into the spinal canal and compresses the anterior spinal artery, it can cause blood supply disruption to the central sulcal artery, resulting in damage to the central part of the spinal cord, also manifesting as central cord injury syndrome.bubble_chart Auxiliary Examination
X-ray manifestations and ossification types: The main feature of ossification of the posterior longitudinal ligament (OPLL) in cervical spine X-rays is an abnormal high-density linear shadow at the posterior edge of the vertebral body. Based on the morphology and extent of the ossification, Japanese scholar Tsuyama classified it into four types (Figure 1): (1) Continuous type, where ossification appears as a continuous cord-like structure spanning several vertebrae, accounting for 27.3%; (2) Segmental type, where ossified masses are cloud-like at the posterior edge of each vertebra, with several ossified foci existing independently without connection. This type is the most common, accounting for 36%; (3) Mixed type, which includes both continuous and segmental ossified masses, accounting for 29.2%; (4) Isolated type, which straddles the upper and lower edges of two adjacent vertebrae, occurring at the intervertebral disc level, accounting for 7.5%. In cervical OPLL, the C2 vertebral segment is the most commonly affected, followed by C4 and C6. Generally, 2 to 5 vertebral segments are the most common number of affected segments, with an average of about 3 segments.
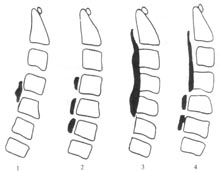
Figure 1 Classification of OPLL
1. Continuous type; 2. Segmental type; 3. Mixed type; 4. Isolated type
To accurately assess the degree of stenosis, conventional X-rays and tomograms can be used to measure the spinal canal stenosis rate. The stenosis rate is the ratio of the maximum anteroposterior diameter of the ossified mass to the sagittal diameter of the spinal canal at the same level on a lateral X-ray. Clinical symptoms and signs largely depend on the degree of spinal cord compression and the effective space within the spinal canal. The stenosis rate objectively reflects the relationship between the sagittal diameter of the spinal canal and the thickness of the ossified mass, indirectly indicating the degree of spinal cord compression. Clinically, patients with a stenosis rate greater than 40% often exhibit severe symptoms and signs, such as significant muscle weakness in the limbs, difficulty walking, or even paralysis, with obvious spinal cord symptoms. Patients with a stenosis rate less than 30% generally have milder clinical manifestations, with most being able to manage daily life independently, and some even able to work. Due to lower limb muscle weakness, these patients are prone to falls and cervical spinal cord injuries, which can suddenly worsen the condition. Patients with a stenosis rate between 30% and 40% typically exhibit clinical manifestations between these two extremes. However, the stenosis rate and spinal cord compression are not always directly proportional.
Myelography can reveal the compression of the dura mater by the ossified mass of the posterior longitudinal ligament, often showing partial or complete obstruction at the level of ossification. To determine the extent of compression and obstruction, both ascending and descending myelography are required. Elevated cerebrospinal fluid protein levels and partial or complete obstruction in the Queckenstedt test are common findings.
CT scanning is an important method for diagnosing OPLL, allowing observation and measurement of the morphology and distribution of ossified masses and their relationship with the spinal cord in the axial plane. On CT images, high-density ossified masses can be seen protruding into the spinal canal at the posterior edge of the vertebral body, causing spinal canal stenosis, reduced capacity, and compression, displacement, and deformation of the spinal cord and nerve roots. The degree of spinal canal stenosis can be represented by the axial stenosis rate. Sagittal reconstruction of the ossified mass on CT images can provide a more comprehensive understanding of the longitudinal and transverse development of the ossification within the spinal canal. On CT images, ossified masses are classified into four types based on morphology: flat type, mushroom type (with a wide free edge and narrow base, resembling a mushroom), hill type (with a wide base and uneven free edge, resembling a hill, the most common type), and bouquet type (with an uneven free edge and lobulated appearance, the least common type). From CT observations, the majority of patients have centrally located ossified masses, with lateral or even fusion with the vertebral side wall being relatively rare.
MRI can determine the normal or abnormal condition of spinal ligaments based on their morphology and signal changes. On T1-weighted and T2-weighted MRI images, ossified posterior longitudinal ligaments often show low signal intensity protruding into the spinal canal, with visible reduction of extradural fat and compression of the dural sac. On corresponding cross-sectional images, ossified posterior longitudinal ligaments with low signal intensity can be seen compressing the spinal cord and nerve roots from the anterior aspect of the spinal canal. Tobias believes that since ossified ligament tissue, like other bone tissues, contains bone marrow and fat, it can also exhibit high signal intensity changes on T1-weighted images. In a group of cases with ossification of the posterior longitudinal ligament, the author observed similar manifestations and found that continuous-type ossification of the posterior longitudinal ligament is easier to diagnose than segmental-type, while isolated-type ossification of the posterior longitudinal ligament, located at the intervertebral disc level, is difficult to differentiate from ossified herniation of the intervertebral disc. Although MRI is deficient compared to CT scans and X-ray tomography in diagnosing ossification of the posterior longitudinal ligament, it can directly outline the extent of ossification while reflecting signal changes in the spinal cord after compression, which is significant for judging surgical prognosis and can exclude other causes of spinal cord compression.
Based on the aforementioned neurological examination, combined with imaging findings from X-rays, CT, and MRI, a definitive diagnosis can often be made. However, two issues need to be clarified: (1) Ossification of the posterior longitudinal ligament does not necessarily present with clinical symptoms. Many cases of severe ossification of the posterior longitudinal ligament discovered through X-ray screenings show that individuals can still live normally without significant symptoms. Similarly, in some cases of extensive ossification of the posterior longitudinal ligament in the cervical spine, not every level produces compressive symptoms. When necessary, nerve evoked potentials and electromyography can be used to determine the affected nerve range and level; (2) Besides ossification of the posterior longitudinal ligament, ossification can also occur in the ligamentum flavum. Simultaneous ossification of these two ligaments can severely affect the size of the spinal canal, leading to significant spinal cord compression. If the thoracic and lumbar spine are also involved, the condition will become more complex and variable.
bubble_chart Treatment Measures
The treatment of posterior longitudinal ligament ossification includes conservative treatment and surgical treatment. For those with mild symptoms, or those whose symptoms are obvious but can be relieved after rest, as well as older individuals with organic diseases, non-surgical therapy can be adopted. Commonly used methods include continuous skull traction, bed rest, cervical collar fixation, physical therapy, and drug treatment. Since the ossified mass of the posterior longitudinal ligament can both directly compress the spinal cord and cause friction on the spinal cord during neck movement, fixing the neck with conservative therapy can eliminate the irritation caused by friction, often achieving better results than expected. For intermittent cervical traction and tuina therapy, there have been reports of worsening symptoms, so they should be used with caution. In addition to anti-inflammatory and analgesic injections and neurotrophic drugs, nerve growth factor has recently been used clinically, showing certain therapeutic effects. Patients with cervical posterior longitudinal ligament ossification should first undergo conservative treatment, and surgical treatment should be considered if conservative therapy is ineffective after a period of time.
Surgical indications: (1) Severe symptoms, obvious ossification, and sagittal diameter of the spinal canal less than 12mm; (2) Progressive worsening of symptoms and signs, and ineffective conservative treatment; (3) Very obvious ossification foci on imaging, at which point the cervical spinal canal is extremely narrow, and minor trauma can cause spinal cord injury, some advocate for aggressive surgery.
Surgery for cervical posterior longitudinal ligament ossification can be performed via anterior or posterior approaches, aiming to relieve the compression of the ossified posterior longitudinal ligament on the spinal cord and expand the spinal canal.
Anterior decompression surgery: Indications for anterior cervical surgery: (1) Segmental posterior longitudinal ligament ossification below C3, ossification thickness less than 5mm, spinal canal stenosis rate less than 45%, anterior surgery is safer; (2) For ossification foci in three or fewer segments, anterior decompression with bone graft fusion is preferred.
Theoretically, all posterior longitudinal ligament ossification should be treated with anterior cervical surgery, directly removing the ossified ligament to relieve spinal cord compression. However, due to technical reasons, for some special cases of posterior longitudinal ligament ossification, surgeons have to choose posterior cervical surgery. Anterior cervical surgery includes two methods: resection and floating of the ossified posterior longitudinal ligament. In the floating method, the intervertebral discs within the decompression range are first removed, then part of the vertebral body is bitten off with rongeurs, and the posterior edge of the vertebral body is ground and removed with a micro-drill, gradually exposing the yellowish-white ossified mass of the posterior longitudinal ligament into the surgical field, and completely freeing and softening the ossified mass around it to make it float. After decompression, the pulsation and expansion of cerebrospinal fluid under the dura mater can gradually move the ossified mass forward, achieving decompression. The decompression area must be implanted with iliac bone blocks.
In recent years, the author has performed anterior cervical resection of posterior longitudinal ligament ossification, and through follow-up, it is concluded that:
1. Strictly grasping the indications for anterior surgery is one of the keys to surgical success.
2. Thoroughly remove the ossified mass, expand the decompression range, and expose the normal dura mater at both ends and sides of the ossified mass.
3. Thoroughly stop bleeding to keep the surgical field clear, facilitating smooth surgery.
4. Operate accurately, gently, and steadily during surgery to prevent spinal cord injury.
5. When the effective sagittal diameter of the spinal canal is less than 6mm (original sagittal diameter of the spinal canal minus the thickness of the ossified mass), more attention should be paid to non-invasive operation. If the sagittal diameter of the spinal canal is less than 3mm, the possibility of paralysis during surgery is very high.
6. Using microsurgical techniques to remove the corresponding intervertebral discs and ossified masses can improve surgical outcomes.
7. Implant trimmed iliac or fibular bones in the decompression area, but do not exceed four vertebral segments to avoid cervical curvature deformity in the advanced stage postoperatively.
8. A semi-tube drainage strip must be placed in the cervical wound for 24 hours.
9. Use upper and lower interface screw fixation during surgery, or use cervical-chin gypsum fixation for three months postoperatively until the bone graft fusion.
Posterior Cervical Surgery Indications for posterior cervical surgery: (1) Continuous or mixed-type ossification of the posterior longitudinal ligament involving 4 or more segments; (2) Ossification of the posterior longitudinal ligament involving C1-C2; (3) Ossification of the posterior longitudinal ligament extending from the cervicothoracic junction to the cervical spine, affecting the lower vertebral segments; (4) Ossification of the posterior longitudinal ligament accompanied by acute cervical spinal cord injury, requiring extensive multi-segment laminectomy for decompression.
Includes two categories: laminectomy decompression and spinal canal plasty. Laminectomy can be further divided into hemilaminectomy and total laminectomy. The former involves the removal of one side of the lamina, the medial edge of the articular process, the base of the spinous process, and the ligamentum flavum. The latter involves the removal of the spinous process and bilateral laminae. The extent of removal should include not only the spinal segments compressed by the ossified lesion but also the laminae of one normal vertebral segment above and below. Hemilaminectomy is relatively simple and has less impact on spinal stability, but the extent of spinal canal expansion is limited. It is usually performed on the side with more severe clinical symptoms and signs. However, if the ossified lesion is more severe on one side of the posterior vertebral edge, or even connected to the lateral wall of the spinal canal, causing significant narrowing on that side, performing hemilaminectomy on that side may increase the risk of spinal cord injury. In such cases, decompression can be performed on the opposite side of the ossified wall to avoid this situation. In total laminectomy, the spinous process of the decompressed segment is first removed, and then the lamina is thinned using bone rongeurs or a micro-drill until the dura mater is faintly visible. The thinned lamina is then cut with scissors, allowing the dura mater and spinal cord within the decompressed area to expand simultaneously. Total laminectomy provides more thorough decompression and is not overly complex, but it significantly compromises spinal stability and may lead to spinal cord compression due to annular scar formation. Long-term follow-up reports of patients who underwent total laminectomy for cervical posterior longitudinal ligament ossification found that about one-third of patients experienced varying degrees of progression in the ossified lesion, and the rate of cervical kyphotic deformity reached 43%.
To address these issues, some have improved laminectomy techniques and designed spinal canal plasty procedures, such as unilateral open-door and bilateral open-door techniques. Although some believe there is no significant difference between laminectomy and laminoplasty in terms of decompression, nerve recovery, spinal stability, and cervical kyphotic deformity, more studies have shown that cervical canal plasty can enhance spinal stability, prevent cervical kyphotic deformity, and control the progression of posterior longitudinal ligament ossification. A crucial technical aspect of spinal canal plasty is maintaining the stability of the posterior spinal structures during surgery to ensure effective spinal cord decompression. Early methods involved suturing the lamina and spinous process to adjacent muscles and articular processes. Although this technique was relatively simple, the sutures were often not secure, leading to the posterior spinal structures reverting to their pre-surgery positions and causing spinal canal stenosis again. To prevent this "door-closing" phenomenon, various laminoplasty methods have been developed (Figures 1, 2, 3). These procedures require precise hand-controlled high-speed drills, bone grafting, and internal fixation techniques. However, due to the complexity of these procedures, intraoperative bleeding increases, surgery time is prolonged, and the risk of spinal cord injury also rises.

Figure 1: Unilateral Open-Door Cervical Laminoplasty
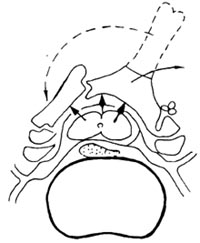
Figure 2: Unilateral Open-Door Cervical Laminoplasty with Bone Grafting
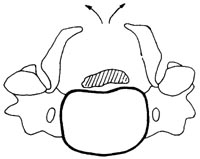
Figure 3: Bilateral Open-Door Cervical Laminoplasty
Cervical Degenerative Changes: Cervical degenerative changes worsen with age, involving pathological alterations in the intervertebral discs, vertebral bodies, laminae, facet joints, ligaments, and other areas. These changes include disc dehydration and degeneration, herniation, narrowing of the intervertebral space, osteophyte formation at the posterior edges of the vertebral bodies, hyperplasia of the facet joints, thickening of the laminae, and hypertrophy of the ligaments. There is a close relationship between cervical degenerative changes and ossification of the posterior longitudinal ligament (OPLL). On one hand, although the exact cause of OPLL remains unclear, it is widely accepted that degenerative changes are one of the factors contributing to OPLL. On the other hand, when OPLL occurs in a segment of the cervical spine, limiting movement, the load on the adjacent intervertebral spaces and facet joints increases, which can gradually lead to and accelerate degenerative changes.
Diffuse Idiopathic Skeletal Hyperostosis (DISH): Also known as Forestier's disease, DISH is a common condition in the elderly, with most patients showing no significant clinical symptoms. The main pathological changes include calcification and ossification of the anterior and lateral aspects of several consecutive vertebral bodies, with or without nerve compression. Calcification and bone hyperplasia also commonly occur at the attachment sites of peripheral bones, tendons, and ligaments. DISH is most frequently seen in the lower thoracic and lumbar regions. Typical X-ray findings show a continuous, broad ossification band along the anterior and lateral aspects of the spine, with normal intervertebral spaces in the affected areas. Clinically, it has been observed that a significant number of OPLL cases are accompanied by DISH, or vice versa. Some authors consider OPLL to be a specific manifestation of DISH. However, epidemiological studies have revealed differences between DISH and OPLL, indicating that they should not be regarded as the same disease.




