| disease | Replantation of Severed Fingers |
In 1963, Chen Zhongwei, Qian Yunqing, and others reported the world's first successful replantation of a completely severed limb 2.5 cm above the right wrist in medical history. After rehabilitation, the patient regained good function in the right hand. In 1964, Malt and Mckhann also reported their successful replantation of a 12-year-old boy's upper arm in May 1962. In 1965, Kleinert achieved successful anastomosis of finger blood vessels, and the same year, Harry Buncke successfully conducted experimental research on rabbit ear and monkey thumb replantation. By 1967, Chen Zhongwei, Komatsa, Tamai, and others successively reported successful finger replantations. The success of limb replantation demonstrated that under certain conditions, severed human tissues and organs can have their blood supply reconstructed using microsurgical techniques, allowing them to reintegrate into the body—a significant breakthrough in medical concepts. Nearly 40 years have passed since China's first successful limb replantation in 1963, and the country has maintained world-leading expertise in the field of limb (and finger) replantation.
bubble_chart Treatment Measures
Key Points of Surgery
1. Thorough Debridement Cover the wound with sterile gauze. First, repeatedly wash the skin with soap and hydrogen peroxide, then clean the wound and rinse it with saline. Both the severed finger and the proximal stump should be cleaned in the same manner. Under the microscope, excise the contused skin edges and remove a full layer of contaminated, edematous, and contused tissue to eliminate the basis for infection. During debridement, identify and mark the tendons, nerves, and vessels to be anastomosed at both ends according to the finger's anatomy. For multiple severed fingers, they can be stored in a refrigerator before and after debridement. Ensure timely administration of antibiotics.
2. Management of Bones and Joints(1) To facilitate vascular and nerve anastomosis, slightly trim the bone ends, but avoid excessive shortening to preserve finger length, shape, and function.
(2) Fix the fracture ends with crossed or oblique Kirschner wires, penetrating both cortices. This method ensures stable fixation without crossing the joint, allowing early mobilization of finger joints to prevent stiffness and accelerate functional recovery. The wire ends should not protrude to reduce infection risk. The conventional intramedullary pinning method is not recommended as it immobilizes the joint, leading to stiffness and inability to control rotational movement, which hinders bone healing.
(3) Preserve joints as much as possible and avoid fusion. If the joint is severed and one articular surface is damaged, retain the intact opposing articular surface, reshape the fractured surface to resemble an articular surface, and suture the joint capsule (Figure 1). Begin active movement after two weeks. Preserve metacarpophalangeal joint mobility at all costs; fusion is prohibited. If the articular surface is damaged, suture the joint capsule to form a mobile or pseudojoint.

Figure 1: Preserve the intact articular surface of the metacarpal or proximal phalanx, reshape the other end, and suture the joint capsule to form a pseudojoint.
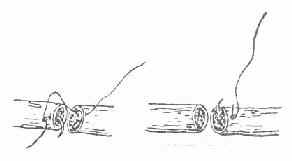
Figure 2: Reverse needle insertion method for nerve suturing.
3. Initial Stage [First Stage] Tendon Repair For the flexor digitorum profundus tendon, use No. 4 silk thread for a "double cross" suture. Since the proximal tendon often retracts significantly, if it cannot be located with wrist flexion, make a small incision near the proximal palmar crease to locate it. Avoid probing the carpal tunnel with forceps to prevent injury to nerves and vessels.
4. Suture two digital nerves whenever possible to restore sensation and nutrition. If necessary, use the less functional stump nerve to repair the more critical one. Debride the nerve ends before suturing and use 9-0 nylon thread for four sutures, preferably with the reverse needle insertion method to avoid injuring nerve bundles (Figure 2).5. Vascular Anastomosis Technique Aim to anastomose as many vessels as possible, ideally two digital arteries and 2–4 digital veins per finger. When freeing vascular stumps, minimize injury and preserve maximum length, temporarily marking them with 8-0 ligatures. Ligate vessels not intended for anastomosis to maintain a clear surgical field and reduce postoperative bleeding. After debridement, small vessels should appear normal under microscopy, with smooth inner membranes. Excise any "floating" inner membrane layers or intraluminal debris to prevent thrombosis. Use 11-0 nylon thread for interrupted everting sutures with two anchoring points. Typically, suture 6–8 stitches for digital arteries, ensuring appropriate tension—neither too tight nor too loose—and avoiding twisting.
If circulatory issues arise in the replanted finger during or after surgery, immediately explore the arteries or veins as needed. If thrombosis is found, excise the anastomosis and redo it. If length is insufficient, perform vascular grafting.
6. Multiple Digit Replantation The survival and functional recovery of multiple digits are crucial in replantation. However, the prolonged surgery time for multiple digit replantation extends the ischemic period of the severed digits, increasing the risk of tissue degeneration and postoperative infection. Nevertheless, due to the absence of muscle tissue in fingers, their tolerance to ischemia is relatively high, allowing for a longer replantation window. The severed fingers should be stored in a 4°C refrigerator. Medical personnel are required to demonstrate strong perseverance and patience.
7. Replantation of Severed Fingers in Children The blood vessels in children are very small, with diameters as narrow as 0.2 mm, requiring extremely precise anastomosis. As long as the surgeon possesses refined skills and strictly adheres to replantation principles and methods, successful outcomes can be achieved in pediatric cases, with faster recovery compared to adults.
8. Postoperative Management Postoperative management is largely similar to limb replantation. Close monitoring of systemic and replanted finger circulation is essential. Antibiotics should be administered, room temperature maintained, and cold stimuli avoided. The affected limb should be kept slightly above heart level. Systemic anticoagulants such as heparin are generally not used, but low-molecular-weight dextran, oral aspirin, and vasodilators like papaverine may be administered. Vascular crises should be promptly investigated and managed. Emphasis should also be placed on functional rehabilitation.






