| disease | Buccal Space Infection |
Buccal space infection refers to an acute suppurative infection in the buccal space. The main manifestations include redness and swelling in the vestibular groove of the mandibular or maxillary molar area, with the vestibular groove becoming shallow and elevated. Severe pain is felt upon touch, along with a sense of fluctuation. Pus is easily extracted by puncture, while the redness and swelling of the facial skin are relatively mild.
bubble_chart Etiology
The buccal space can be classified into broad and narrow definitions. The broad buccal space refers to the space located between the skin of the cheek and the buccal mucosa. Its upper boundary is the lower edge of the zygomatic bone; the lower boundary is the lower edge of the mandible; the anterior boundary extends from the lower edge of the zygomatic bone, passing through the corner of the mouth to the lower edge of the mandible; the posterior boundary superficially corresponds to the anterior edge of the masseter muscle, while its deep aspect includes structures such as the zygomatic muscle and the pterygomandibular ligament (Figure 3). In addition to containing areolar tissue and adipose tissue (the buccal fat pad), this space also accommodates the facial nerve, the long buccal nerve, the external maxillary artery, the anterior facial vein, as well as the buccal lymph nodes and the superior maxillary lymph nodes. The narrow buccal space refers to a small fascial space between the masseter muscle and the buccinator muscle, where the buccal fat pad is situated. This space is also known as the masseteric-buccal space.
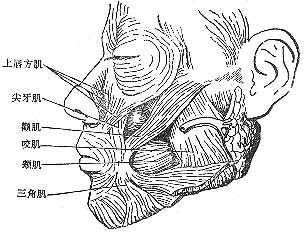
Figure 3 Anatomical location of the buccal space.
The buccal space communicates with the infratemporal space, temporal space, masseteric space, pterygomandibular space, and infraorbital space via blood vessels, adipose connective tissue.
Infections in the buccal space can originate from apical infections or alveolar abscesses of the posterior teeth in the upper or lower jaw, as well as from injuries to the cheek skin, ulcers of the buccal mucosa, or inflammation of the buccal or superior maxillary lymph nodes.bubble_chart Clinical Manifestations
The clinical features of the buccal space depend on the location of abscess formation. Abscesses in the subcutaneous tissue or submucosa of the cheek progress slowly and have a relatively localized swelling. When the infection involves the buccal fat pad, the inflammation develops rapidly, with swelling spreading to the entire cheek and potentially extending to adjacent spaces, leading to multi-space infections.
1. Medical History A history of acute suppurative wisdom tooth pericoronitis or acute periapical periodontitis of the upper or lower molars.
2. Clinical Manifestations When the abscess occurs between the buccal mucosa and the buccinator muscle, the vestibule groove in the molar region of the mandible or maxilla appears red and swollen, with a shallow and raised surface. Severe pain is elicited upon palpation, along with a sense of fluctuation, and pus can be easily aspirated during puncture. The skin redness and swelling on the face are relatively mild. If the abscess develops between the skin and the buccinator muscle, especially when the entire buccal fat pad is involved in the inflammation, the facial skin exhibits severe redness and swelling, with a shiny and distended appearance. Inflammatory edema may spread beyond the anatomical boundaries of the buccal space, but the center of redness, swelling, and tenderness remains at the buccinator muscle. Pus can be aspirated during local puncture. The patient may present with fever and elevated white blood cell count.
bubble_chart Treatment MeasuresAfter the formation of an abscess, the decision to perform incision and drainage should be based on the location of the abscess, either intraorally or externally on the face. The intraoral incision should be made at the dependent part of the abscess, specifically in the oral vestibule or the buccal sulcus of the mandible (Figure 1). For subcutaneous abscesses in the cheek, an incision can be made on the superficial skin overlying the abscess. In cases of extensive buccal space infection, an incision should be made 1–2 cm below the lower border of the mandible, parallel to it, followed by blunt dissection upward through the subcutaneous tissue to reach the abscess cavity in the cheek. Care must be taken to avoid injury to the facial nerve, parotid duct, and blood vessels in the cheek (Figure 2).

Figure 1 Intraoral incision and drainage for buccal space abscess
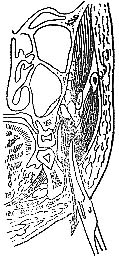
Figure 2 External incision and drainage for buccal space abscess




