| disease | Sick Sinus Syndrome |
| alias | Sick Sinus Syndrome, Sick Sinus Syndrome, SSS, Sinus Node Insufficiency |
Abbreviated as sick sinus syndrome, also known as sinoatrial node dysfunction. It is caused by pathological changes in the sinoatrial node and its adjacent tissues, leading to impaired sinoatrial node pacing function and/or sinoatrial conduction disorders, resulting in various arrhythmias and clinical symptoms. Symptoms mostly appear after the age of 40. According to data from Zhongshan Hospital Affiliated with Shanghai Medical University, the most common age groups for patients with clear symptoms are 40–50 and 60–70 years old.
bubble_chart Etiology
Common disease causes include cardiomyopathy, coronary heart disease, and myocarditis, as well as connective tissue diseases, metabolic or infiltrative disorders. In many cases, the disease cause remains unknown. According to data from Zhongshan Hospital of Shanghai Medical University, 37.9% of SSS cases have no identifiable cause. Autopsy literature indicates that idiopathic degenerative changes in the cardiac conduction system are the most common cause of SSS. In addition to the sinoatrial node and its adjacent tissues, other parts of the cardiac conduction system may also be affected, leading to multiple potential pacemaker and conduction dysfunctions. Cases combined with atrioventricular junctional pacemaker or conduction insufficiency are also referred to as binodal disease; when both the left and right bundle branches are involved, it is called a complete conduction system disorder.
The progression of SSS is mostly slow, with the period from symptom onset to severe symptoms lasting 5 to 10 years or longer. A few cases present acutely, seen in acute myocardial infarction and acute myocarditis.
bubble_chart Clinical ManifestationsThe clinical manifestations vary in severity and may present as intermittent episodes. They are primarily characterized by symptoms of insufficient blood supply to organs such as the brain, heart, and kidneys due to slow heart rate, especially cerebral hypoperfusion. Mild cases include lack of strength, dizziness, blurred vision, insomnia, poor memory, slow reaction time, or irritability, which can easily be misdiagnosed as neurasthenia. In elderly patients, they are also often misdiagnosed as cerebrovascular accidents or aging syndrome. Severe cases may cause transient blackouts, near-syncope, syncope, or Adams-Stokes syndrome attacks. Some patients experience paroxysmal episodes of supraventricular tachyarrhythmia, also known as bradycardia-tachycardia syndrome. During tachyarrhythmia episodes, the heart rate may suddenly accelerate to over 100 beats per minute, lasting for varying durations. After the tachycardia abruptly terminates, cardiac arrest may occur with or without syncope. Severe bradycardia or tachycardia, in addition to causing palpitations, can exacerbate pre-existing cardiac symptoms, leading to heart failure or cardiac colicky pain. Extremely low cardiac output severely impairs perfusion to organs like the kidneys, resulting in oliguria and indigestion. Bradycardia-tachycardia syndrome may also lead to thromboembolic symptoms.
bubble_chart Auxiliary Examination
[ECG Characteristics]
include the ECG manifestations of sinus node dysfunction itself and the escape beats and/or escape rhythms secondary to sinus node dysfunction, as well as possible concurrent short bursts of tachyarrhythmias and/or ECG manifestations of involvement in other parts of the conduction system. ① Sinoatrial block and/or sinus arrest and/or marked sinus bradycardia; ② Escape beats, short bursts or sustained escape rhythms, escape-capture bigeminy, wandering pacemaker; ③ Associated atrial tachyarrhythmias, such as frequent atrial premature beats, paroxysmal or recurrent short bursts of atrial fibrillation, atrial flutter, or atrial tachycardia, forming the so-called bradycardia-tachycardia syndrome with the slow sinus rhythm (Figure 1). After the spontaneous cessation of tachyarrhythmias, sinus rhythm often reappears following a pause of more than 2 seconds; ④ Dysfunction of the atrioventricular junctional pacemaker and/or conduction, manifested as delayed atrioventricular junctional escape beats, slow atrioventricular junctional escape rhythm (escape cycle >1.5s), or atrioventricular block, occasionally combined with bundle branch block.
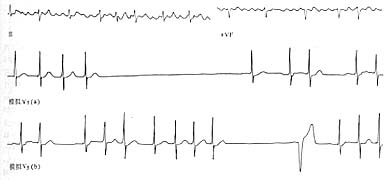
Figure 1 Sick Sinus Syndrome
The first strip (Ⅱ)(aVF) shows atrial flutter. The second strip, simulating V5 (a), demonstrates a cardiac pause lasting up to 3.96 seconds after the cessation of atrial fibrillation. The third strip, simulating V5 (b), shows a cardiac pause following the cessation of a short burst of supraventricular tachycardia, followed by a ventricular escape beat.
Zhongshan Hospital of Shanghai Medical University classified the dynamic ECG (DCG) manifestations into 4 types: Type I, severe and persistent sinus bradycardia (21.1%); Type II, sinus bradycardia with sinus arrest or sinoatrial block (30.5%); Type III, bradycardia-tachycardia syndrome (12.6%); Type IV, dual node disease (35.8%). Among these, the incidence of syncope or blackout in the dual node disease type (70.6%) was significantly higher than in the other types. The average pause time in DCG for patients with clinical manifestations of syncope or blackout was 4.9±0.7 seconds, significantly longer than in asymptomatic patients. For patients not treated with pacemakers, an average follow-up of 9.5 years showed a relatively long natural history, with no deaths from this syndrome during the follow-up period. However, Sutton et al. observed a one-year survival rate of 85–92% and a seven-year survival rate of 52%.
The diagnosis is primarily based on the electrocardiographic manifestations of sinoatrial node dysfunction, excluding hypervagotonia or drug effects. In early or atypical cases, sinoatrial node dysfunction may present intermittently or manifest predominantly as sinus bradycardia, making it difficult to confirm the diagnosis. The following tests can help evaluate sinoatrial node function. A 24-hour Holter monitor may capture various characteristic ECG features of sick sinus syndrome (SSS). If results are negative, the test can be repeated within a short period. To exclude the influence of autonomic tone changes, an atropine test (intravenous injection of 1–2 mg atropine) or an isoproterenol test (intravenous bolus or infusion of 1–2 µg) can be performed. If the heart rate fails to increase to 90 beats per minute after administration, it suggests impaired sinoatrial node function. However, a negative result (heart rate increasing to 90 beats per minute or higher) does not rule out the condition. Atrial pacing can also be used to measure the sinus node recovery time (SNRT) and sinoatrial conduction time (SACT). Patients with sick sinus syndrome often exhibit SNRT and SACT significantly exceeding the upper normal limits. There are differing opinions on the value of these electrophysiological indicators for assessing sinoatrial node function. Generally, normal results do not exclude the diagnosis, while results significantly above the upper normal limit (e.g., SNRT exceeding 2000 ms) may be clinically relevant. Many believe these tests are less diagnostically valuable than Holter monitoring.
Treatment should target the disease cause. Asymptomatic patients can undergo regular follow-ups with close monitoring of their condition. For those with significantly slow heart rates or accompanying symptoms, oral atropine or salbutamol may be tried. Patients with dual node disease, tachycardia-bradycardia syndrome, or obvious symptoms of insufficient cerebral blood supply, such as near-syncope or syncope, should be fitted with an on-demand artificial cardiac pacemaker. Atrioventricular sequential demand pacemakers are more physiologically suitable than VVI pacemakers. For those with concurrent rapid arrhythmias, medications should be added after pacemaker implantation to control the episodes of rapid arrhythmia. Recently, programmable automatic scanning cardioverters have also been used to treat tachycardia-bradycardia syndrome (see the chapter on artificial cardiac pacemakers). During bradycardia, the device operates in VVI pacing mode, and during tachycardia episodes, it switches from VVI to VVT, delivering scanning stimuli or short bursts of rapid stimulation to terminate the tachycardia. Patients with sick sinus syndrome should avoid medications that may slow the heart rate, such as antihypertensives, antiarrhythmics, cardiotonics, beta-adrenergic blockers, and calcium antagonists. Electrical cardioversion should not be performed during episodes of atrial fibrillation or atrial flutter.





