| disease | Peptic Ulcer |
| alias | Stomach Ulcer, Stomach, Duodenal Ulcer |
Peptic ulcers mainly refer to chronic ulcers that occur in the stomach and duodenum, being a common and frequently encountered disease. The formation of ulcers involves various factors, among which the digestive effect of acidic gastric juice on the mucosa is the fundamental factor in ulcer formation, hence the name. Peptic ulcers can occur in any area exposed to acidic gastric juice, such as the lower esophagus, the anastomotic site after gastrointestinal surgery, the jejunum, and Meckel's diverticulum with ectopic gastric mucosa. The vast majority of ulcers occur in the duodenum and stomach, hence they are also called gastric and duodenal ulcers.
bubble_chart Epidemiology
This disease is a global and frequently occurring condition, and the exact incidence rate currently lacks large-scale population statistics. However, the incidence can vary significantly across different countries and regions. Some analyses based on X-ray examinations and autopsy data estimate that the overall incidence rate may account for 10–12% of the population; others estimate that 1 in 5 men and 1 in 10 women may suffer from this disease in their lifetime.
In most countries and regions, duodenal ulcers are more common than gastric ulcers. It is more prevalent in males, with a male-to-female ratio of 5.23–6.5:1. The disease can occur at any age but is most common among young and middle-aged adults. The onset age of gastric ulcers is generally about 10 years later than that of duodenal ulcers, but it is not uncommon for individuals aged 60–70 or older to experience their first episode. The average age of female patients is higher than that of male patients.
bubble_chart EtiologyRecent experimental and clinical studies have shown that excessive gastric acid secretion, Helicobacter pylori infection, and weakened gastric mucosal protection are key factors in the development of peptic ulcers. Delayed gastric emptying, bile reflux, the role of gastrointestinal peptides, genetic factors, medication factors, environmental factors, and psychological factors are all associated with the occurrence of peptic ulcers.
(1) Excessive Gastric Acid Secretion Hydrochloric acid is the main component of gastric juice, secreted by parietal cells and regulated by neural and humoral mechanisms. It is known that parietal cells contain three types of receptors: histamine receptors, cholinergic receptors, and gastrin receptors, which are activated by histamine, acetylcholine, and gastrin, respectively. When the receptors on the surface of parietal cells bind to their respective substances, intracellular second messengers are activated, thereby influencing gastric acid secretion. There are two primary second messengers in parietal cells: cAMP and calcium. After the membrane receptors of parietal cells bind to histamine, they couple with the stimulatory GTP-binding protein, activating adenylate cyclase, which catalyzes the conversion of ATP to cAMP. cAMP then activates a protein kinase, leading to the phosphorylation of an as-yet-unidentified intracellular protein, ultimately resulting in the activation of the H+K+-ATPase (also known as the hydrogen ion pump or proton pump) within the parietal cells, promoting acid secretion. When acetylcholine receptors and gastrin receptors bind to acetylcholine and gastrin, respectively, they couple with GTP-binding proteins, activating membrane-bound phospholipase C. This enzyme catalyzes the breakdown of membrane phospholipids, generating inositol trisphosphate (IP3
) and diacylglycerol. IP3 triggers the release of calcium from intracellular stores, which in turn activates the H+K+-ATPase, promoting H+ secretion. Acetylcholine also increases the permeability of the cell membrane to calcium. Gastrin and acetylcholine can stimulate enterochromaffin-like (ECL) cells to release histamine, and they exhibit synergistic effects with histamine. Parietal cells also have somatostatin receptors on their surface. Upon activation, these receptors bind to the inhibitory membrane receptor Gi, which, via the inhibitory GTP-binding protein, suppresses adenylate cyclase, thereby reducing intracellular cAMP levels and decreasing H+ secretion by parietal cells. Regardless of the type of stimulus, the excitation of parietal cell receptors ultimately influences the secretory membrane structure at the apical surface of the cell and the proton pump—H+K+-ATPase—through second messengers (cAMP and Ca2+), leading to either an increase or decrease in H+ secretion. The gastric proton pump is a hydrogen ion ATPase that relies on ATP for energy. It is a counter-transport pump, catalyzing the exchange of intracellular H+ and extracellular K+ in equal amounts. It can generate a H+ gradient of 4,000,000:1 across the parietal cell membrane, a gradient far exceeding those produced by proton pumps in other parts of the body (e.g., the colon or renal cortical collecting ducts).In parietal cells at rest, proton pumps are located in the smooth tubulovesicles of the cytoplasm. Upon parietal cell stimulation, tubulovesicles containing proton pumps migrate toward the apical membrane of the cell, and the tubulovesicle membrane fuses with the apical membrane, increasing the apical membrane surface area. After the apical membrane retracts, secretory canaliculi are formed and drain into the glandular lumen. The movement of tubulovesicles is promoted by cAMP and Ca2+
, while membrane fusion is accompanied by both the activation of H+, K+-ATPase and an increase in membrane permeability to Cl- and K+. It remains unclear whether the transport of Cl- and K+ across the membrane occurs through separate channels or via a KCl channel that mediates the cotransport of K+ and Cl-. Regardless of the mechanism, since K+ and Cl- are simultaneously transported out of the cell, the exchange of H+ and K+ driven by H+, K+-ATPase ultimately leads to HCl secretion. The concentration of hydrochloric acid secreted by parietal cells is constant at 160 mmol/L, with a pH of 0.9. However, the actual pH of gastric juice ranges from 1.3 to 1.8 due to the presence of alkaline mucus and refluxed intestinal fluid.In the pathogenesis of duodenal ulcer, excessive gastric acid secretion plays a significant role. The statement "no acid, no ulcer" holds true for duodenal ulcers. The basal acid output (BAO) and maximal acid output (MAO) of duodenal ulcer patients are significantly higher than those of normal individuals; duodenal ulcers never occur in individuals with no or very little gastric acid secretion.
After chyme enters the duodenum from the stomach, under the stimulation of gastric acid and chyme, the pancreas secretes large amounts of secretin, pancreozymin, and cholecystokinin. In addition to secreting mucus, the intestinal mucosa also releases hormones such as enteroglucagon, gastric inhibitory peptide (GIP), and vasoactive intestinal peptide (VIP). These hormones inhibit gastric acid secretion and stimulate gastrin secretion. Therefore, when the function of the duodenal mucosa in releasing these hormones declines, it can lead to increased secretion of gastrin and gastric acid, contributing to the formation of duodenal ulcers.
The chronicity and recurrence of gastric ulcers, the nature of complications, and the tendency of ulcers to heal under conditions of reduced gastric acid all suggest similarities in pathogenesis between gastric ulcers and duodenal ulcers. However, the BAO and MAO of gastric ulcer patients are similar to or even lower than those of normal individuals. Some gastric mucosal protective drugs (non-antacids), although they do not reduce gastric acid, can promote ulcer healing. Certain drugs that injure the gastric mucosa, such as aspirin, can cause gastric ulcers, and experimental evidence shows that continuously removing mucus from the gastric cavity in animals can lead to gastric ulcers. These facts suggest that the occurrence of gastric ulcers is due to local damage to the gastric mucosa. The destruction of the gastric mucosal protective barrier renders it unable to effectively counteract the erosive and digestive effects of gastric acid and pepsin, leading to ulcer formation.
(2) Helicobacter pylori infection HP infection is the primary cause of chronic gastritis and an important cause of peptic ulcers. In epithelial cells where HP adheres, microvilli are reduced, intercellular connections are lost, the cells appear swollen with irregular surfaces, intracellular mucus granules are depleted, and vacuolar degeneration occurs. Bacteria form adhesion pedestals and shallow cup-like structures with the cells.
(3) Gastric mucosal protective mechanisms Under normal circumstances, neither the physicochemical factors of various foods nor the digestive effects of acidic gastric juice can injure the gastric mucosa to cause ulcer formation. This is because the normal gastric mucosa has protective functions, including mucus secretion, the integrity of the gastric mucosal barrier, abundant mucosal blood flow, and epithelial cell regeneration.
On the surface of the gastric mucosa, there is a mucus layer approximately 0.25–0.5 mm thick, which is about 10–20 times the thickness of the surface epithelial cells and roughly equivalent to 1/2–1/4 the depth of the gastric glands. The mucus forms an unstirred zone on the cell surface; it also contains mucin at a concentration of about 30–50 mg/ml. Most of the water in the mucus fills the spaces between mucin molecules, thereby helping to prevent the back-diffusion of hydrogen ions. The surface epithelial cells of the stomach can also secrete bicarbonate, with a secretion rate approximately 5–10% of the maximum acid output. The process of gastric HCO3- secretion depends on metabolic energy. Intracellular CO2 and H2O, under the action of carbonic anhydrase, generate HCO3-; the latter crosses the luminal membrane and is secreted into the gastric lumen in exchange for Cl-. The basolateral membrane of the cell contains Na+K+-ATPase. Under the action of this enzyme, a high extracellular concentration of Na+ is maintained. Na+ then diffuses back into the cell, and in exchange, the H+ generated during the formation of HCO3- is expelled from the cell.
Neither mucus nor bicarbonate alone can protect the gastric epithelium from damage by gastric acid and pepsin, but when combined, they form an effective barrier. Mucus acts as a non-flowing layer that buffers; within the mucus layer, bicarbonate slowly moves toward the gastric lumen, neutralizing the acid that slowly moves toward the epithelial surface, thereby creating an H+ gradient across the mucus layer. When the gastric pH is 2.0, the pH within the mucus layer on the epithelial surface can remain at 7.0. The formation of this gradient depends on the rate of alkaline secretion and the thickness of the mucus layer it traverses, while the thickness of the mucus layer is determined by the rate of mucus renewal and its loss from the epithelial surface into the gastric lumen. Disruption of any one or several of these factors can reduce the pH gradient and compromise the protective barrier.
(4) Delayed Gastric Emptying and Bile Reflux In gastric ulcer disease, degenerative changes in the antrum and pyloric region can impair antral contractions, affecting the forward movement of chyme. Delayed gastric emptying may be a factor in the pathogenesis of gastric ulcer disease.
Certain components of duodenal contents, such as bile acids and lysolecithin, can injure the gastric epithelium. Reflux of duodenal contents into the stomach can cause chronic inflammation of the gastric mucosa. The damaged gastric mucosa becomes more susceptible to destruction by acid and pepsin. In gastric ulcer disease, the concentration of bile acid conjugates in fasting gastric juice is significantly higher than in normal controls, suggesting that bile reflux into the stomach may play an important role in the pathogenesis of gastric ulcer disease.
(5) Role of Gastrointestinal Peptides Many gastrointestinal peptides are known to influence gastric acid secretion, but only gastrin has been studied extensively in relation to peptic ulcers. The role of gastrin in the pathogenesis of common peptic ulcers remains unclear.
(6) Genetic Factors It is now widely accepted that genetic predisposition plays a role in the development of peptic ulcers, and it has been demonstrated that gastric ulcers and duodenal ulcers are inherited independently. The incidence of gastric ulcers is three times higher in the families of gastric ulcer patients than in the general population, while duodenal ulcers are more common in the families of duodenal ulcer patients than gastric ulcers.
(7) Drug Factors Certain antipyretic analgesics, anticancer drugs, and others—such as indomethacin, phenylbutazone, aspirin, adrenocortical hormones, fluorouracil, and methotrexate—have been implicated as ulcerogenic factors. Among these, aspirin has been studied the most, with results showing that regular aspirin users are more prone to developing gastric ulcers. Some studies indicate that the prevalence of gastric ulcers is about three times higher in regular aspirin users compared to non-users.
Adrenocortical steroids are likely associated with ulcer formation and reactivation. A study of 5,331 cases showed that corticosteroid therapy lasting more than 30 days or a total prednisone dose exceeding 1,000 mg can induce ulcers. In patients with a history of ulcers, these drugs can exacerbate the condition.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as indomethacin, phenylbutazone, ibuprofen, and naproxen, can also inhibit prostaglandin synthesis to varying degrees, theoretically producing clinical effects similar to aspirin. Reserpine and similar drugs have histamine-like effects, increasing gastric acid secretion and thus posing a potential ulcerogenic risk.
(8) Environmental Factors Smoking can stimulate increased gastric acid secretion, generally about 91.5% higher than in non-smokers; smoking can cause vasoconstriction and inhibit the secretion of pancreatic juice and bile, thereby weakening their ability to neutralize gastric acid in the duodenum, leading to persistent duodenal acidification. Nicotine in tobacco can reduce the tension of the pyloric sphincter, impairing its closing function and causing bile reflux, which damages the gastric mucosal barrier. The incidence of peptic ulcers is significantly higher in smokers compared to the control group. Under the same effective drug treatment conditions, the ulcer healing rate is also significantly lower in the former than in the latter. Therefore, long-term heavy smoking is detrimental to ulcer healing and can also lead to recurrence.
Food can cause physicochemical damage to the gastric mucosa. Overeating or irregular eating may disrupt the rhythmic secretion of gastric juices. Clinical observations suggest that foods such as coffee beans, strong tea, hard liquor, spicy seasonings, pickled vegetables, as well as poor dietary habits like picky eating, eating too quickly, consuming food that is too hot or too cold, and overeating, may all be contributing factors to the onset of this condition.
(9) Psychological Factors According to the modern biopsychosocial medical model, peptic ulcers are considered one of the classic psychosomatic diseases. Psychological factors can influence gastric acid secretion.
bubble_chart Pathological Changes
1. Location Gastric ulcers mostly occur on the lesser curvature of the stomach, especially at its lowest point—the gastric angle. They can also be found in the gastric antrum or the upper part of the gastric body, but are rarely seen on the greater curvature or the fundus of the stomach. Postoperative anastomotic ulcers, which develop after partial gastrectomy, are commonly located on the jejunal side of the anastomosis. Duodenal ulcers primarily appear in the bulb, with about 5% occurring below the bulb, known as postbulbar ulcers. When ulcers are present on both the anterior and posterior walls or the greater and lesser curvatures of the bulb simultaneously, they are referred to as kissing ulcers. If ulcers are found in both the stomach and duodenum, they are termed compound ulcers.
2. Number The vast majority of peptic ulcers occur singly, but a small number may have 2–3 ulcers coexisting, known as multiple ulcers.
3. Size Duodenal ulcers generally have a diameter of <1 cm, while gastric ulcers typically measure <2.5 cm. However, giant ulcers with diameters >2.5–4 cm are not uncommon.
4. Morphology The typical ulcer is round or oval, deep, and firm-walled, resembling a "punched-out" or "fistula disease funnel" shape. The ulcer margin is often thickened with hyperemia and edema, while the base is smooth and clean, usually covered by a fibrinous or fibropurulent membrane, appearing grayish-white or grayish-yellow (membranous exudate).
5. Complications If an ulcer progresses further, it may penetrate the muscular layer, termed a penetrating ulcer. When it perforates the serosal layer, it causes perforation. Perforation of the anterior wall often leads to acute peritonitis, whereas perforation of the posterior wall tends to adhere to adjacent organs such as the liver, pancreas, or transverse colon, resulting in a penetrating ulcer. When the blood vessels at the ulcer base, particularly the stirred pulse, are eroded, massive hemorrhage may occur. Repeated recurrences or extensive destruction may leave scars after healing. Scar contraction can lead to local deformity and pyloric obstruction as sequelae of ulcer disease.
bubble_chart Clinical Manifestations
(1) Characteristics of Peptic Ulcer Pain
1. Chronicity Since ulcers can heal on their own but often recur after healing, patients typically experience long-term, recurrent episodes of upper abdominal pain. The average course of the disease lasts 6–7 years, with some cases persisting for 10–20 years or even longer.
2. Periodicity Recurrent and periodic episodes of upper abdominal pain are a hallmark of peptic ulcers, particularly duodenal ulcers. The pain may last for days, weeks, or longer, followed by extended periods of relief. While episodes can occur year-round, they are more common in spring and autumn.
3. Rhythm Ulcer pain exhibits a clear correlation and rhythm with meals. During the day, gastric acid secretion is lowest between 3 a.m. and breakfast, so pain rarely occurs during this time. Duodenal ulcer pain often arises between meals, persisting until the next meal or after taking antacids. Some duodenal ulcer patients may experience nighttime pain due to higher gastric acid levels, especially if they ate before bedtime. Gastric ulcer pain is less regular, usually occurring within an hour after a meal and gradually subsiding over 1–2 hours, only to recur with the next meal.
4. Pain Location Duodenal ulcer pain is typically felt in the mid-upper abdomen, either above the navel or slightly to the right. Gastric ulcer pain is also located in the mid-upper abdomen but tends to be slightly higher, near the xiphoid process or slightly to the left. The pain area is usually a few centimeters in diameter. Since visceral pain localization on the body surface is imprecise, the pain location may not accurately reflect the ulcer's anatomical position.
5. Pain Nature The pain is often dull, burning, or hunger-like, generally mild and tolerable. Persistent severe pain suggests ulcer penetration or perforation.
6. Influencing Factors Pain can be triggered or worsened by emotional stress, fatigue, dietary indiscretion, medications, or weather changes. It may be relieved or alleviated by rest, eating, taking antacids, applying pressure to the painful area, or vomiting.
(2) Other Symptoms and Signs of Peptic Ulcer
1. Other Symptoms In addition to mid-upper abdominal pain, patients may experience increased salivation, heartburn, regurgitation, acid belching, belching, nausea, vomiting, and other gastrointestinal symptoms. Appetite usually remains normal, though some may avoid eating due to postprandial pain, leading to weight loss. Systemic symptoms may include insomnia and other neurofunctional manifestations, or signs of autonomic imbalance such as moderate pulse and profuse sweating.
2. Signs During an active ulcer episode, there may be localized tenderness in the mid-upper abdomen, usually mild and corresponding roughly to the ulcer's location.
(3) Special Types of Peptic Ulcer
1. Asymptomatic Ulcer These ulcers show no obvious symptoms and are discovered incidentally during endoscopy or X-ray barium meal exams for other conditions, or when complications like bleeding or perforation occur, or even during autopsies. Such ulcers can occur at any age but are more common in the elderly.
2. Childhood Peptic Ulcer Peptic ulcers are less common in children than in adults and can be classified into four types.
(1) Infantile Type: Infantile ulcers are acute and occur in newborns and infants under two years old. The cause is unknown. In newborns, duodenal ulcers are more common than gastric ulcers. These ulcers may heal quickly or lead to perforation or bleeding, which can be rapidly fatal. In infants between newborns and two years old, the ulcer presentation is similar to that in newborns, primarily manifesting as bleeding, obstruction, or perforation.
(2) Secondary type: The occurrence of this type of ulcer is associated with some serious systemic diseases, such as sepsis, central nervous system diseases, severe burns, and the application of corticosteroids. It can also occur after congenital pyloric stenosis, liver diseases, and cardiac surgery. This type of ulcer occurs with equal frequency in the stomach and duodenum and can be seen in children of any age and gender.
(3) Chronic type: This type of ulcer mainly occurs in school-age children. As age increases, the manifestations of the ulcer become more similar to those in adults. However, in young children, the pain is more diffuse, often around the navel, and unrelated to meals. Vomiting frequently occurs, likely due to the smaller duodenum being more prone to obstruction caused by edema and spasms. It is not until adolescence that the typical localized, rhythmic pain in the upper abdomen appears. Duodenal ulcers are more common than gastric ulcers, and boys are more affected than girls. The pathogenesis of this type of ulcer is the same as the fundamental causes of adult ulcer disease.
(4) Ulcers associated with endocrine adenomas: This type of ulcer occurs in gastrinomas and multiple endocrine neoplasia type I (MEN I), also known as Wermer syndrome.
3. Peptic ulcers in the elderly Gastric ulcers are more common, but duodenal ulcers can also occur. Gastric ulcers often exceed 2.5 cm in diameter and are frequently located in the high posterior wall of the gastric body or the lesser curvature. Peptic ulcers in the elderly typically present with irregular mid-epigastric pain, hematemesis, and/or melena, as well as weight loss. Rhythmic pain, nocturnal pain, and acid reflux are rare. They are prone to major bleeding, which is often difficult to control.
4. Pyloric channel ulcers These are relatively rare and often associated with excessive gastric acid secretion. The main manifestations include: ① Severe mid-epigastric pain immediately after meals, which is non-rhythmic and may cause food aversion; antacids can relieve the pain. ② Frequent vomiting, with pain relief after vomiting. Abdominal pain, vomiting, and reduced food intake can lead to weight loss. The efficacy of medical treatment for this type of peptic ulcer is poor.
5. Postbulbar ulcers These account for about 5% of peptic ulcers and are usually located proximal to the duodenal papilla. Nocturnal abdominal pain and referred back pain are more common in postbulbar ulcers, as is massive bleeding. Medical treatment is less effective.
6. Combined ulcers This refers to the simultaneous presence of gastric and duodenal ulcers, with the duodenal ulcer usually developing first. This condition accounts for about 7% of peptic ulcers and is more common in males. The clinical symptoms are nonspecific, but the incidence of pyloric stenosis is higher, and the bleeding rate is as high as 30–50%, with bleeding mostly originating from the gastric ulcer. The disease is often stubborn, with a high complication rate.
7. Giant ulcers A giant gastric ulcer is defined as an ulcer with a diameter exceeding 2.5 cm on X-ray barium meal examination, though not all are malignant. The pain is often atypical and may not be fully relieved by antacids. Vomiting and weight loss are significant, and life-threatening bleeding can occur. Sometimes, a hard mass formed by fibrous tissue can be palpated in the abdomen. Long-standing giant gastric ulcers often require surgical treatment.
Giant duodenal ulcers refer to those with a diameter of 2 cm or more, mostly located in the bulb but sometimes postbulbar. Ulcers on the posterior wall of the bulb are often surrounded by inflammatory masses and may invade the pancreas. The pain is severe and persistent, often radiating to the back or right upper abdomen. Vomiting and weight loss are significant, and bleeding, perforation, and obstruction are common. Bleeding and perforation may occur simultaneously. Giant duodenal ulcers with complications are primarily treated surgically.
8. Esophageal ulcers These also result from contact with acidic gastric fluid. Ulcers usually occur in the lower esophagus and are mostly solitary, though about 10% are multiple. Their size ranges from a few millimeters to quite large. This condition often occurs in patients with reflux esophagitis and sliding hiatal hernia accompanied by gastroesophageal reflux. The ulcers may develop in squamous epithelium or columnar epithelium (Barrett’s epithelium). Esophageal ulcers can also occur after esophagogastrostomy or esophagojejunostomy, resulting from the reflux of bile and pancreatic secretions.
Esophageal ulcers mostly occur between the ages of 30 and 70, with about two-thirds of patients being over 50 years old. The main symptom is pain behind the lower sternum or in the upper abdomen, often occurring during eating or drinking and worsening when lying down. The pain may radiate to the interscapular region, the left side of the chest, or upward to the shoulders and neck. Dysphagia is also relatively common, resulting from secondary esophageal spasms or fibrosis-induced esophageal strictures. Other possible symptoms include nausea, vomiting, belching, and weight loss. The main complications are obstruction, bleeding, and perforation into the mediastinum or upper abdomen. Diagnosis primarily relies on X-ray examination and endoscopy.
9. Refractory ulcer refers to a peptic ulcer that does not respond to general medical treatment. There is no unified diagnostic standard, but it includes the following conditions: ① Under hospitalization; ② Chronic ulcers that recur frequently over many years and show increasingly poor response to medical treatment. The development of refractory ulcers may be related to the following factors: ① Complications such as penetrating ulcers or pyloric obstruction; ② Ulcers in special locations (e.g., postbulbar or pyloric canal) that respond poorly to medical treatment; ③ Failure to eliminate underlying causes (e.g., psychological factors like anxiety or stress, improper diet, or inappropriate treatment); ④ Diseases that cause refractory ulcers, such as hyperacidic states (e.g., gastrinoma, hyperparathyroidism).
10. Stress ulcer refers to acute ulcers that develop in the stomach and duodenum under conditions of severe stress, such as major burns, craniocerebral trauma, brain tumors, intracranial neurosurgery, other central nervous system diseases, severe trauma, major surgery, or serious acute or chronic internal diseases (e.g., sepsis, pulmonary insufficiency). Acute stress ulcers caused by severe burns are also called Cushing ulcers; those caused by craniocerebral trauma, brain tumors, or intracranial neurosurgery are also termed Cushing ulcers. The incidence of stress ulcers has shown an increasing trend in recent years.
The pathogenesis of stress ulcers remains unclear, but their development may involve two mechanisms: ① Excessive gastric secretion during stress, leading to autodigestion of the mucosa and the formation of stress ulcers. Cushing ulcers may result directly from significantly increased gastric acid secretion. ② Intense and prolonged stress triggers strong sympathetic stimulation and elevated circulating catecholamine levels, which can open arteriovenous shunts in the submucosa of the stomach and duodenum. As a result, blood that normally flows through the mucosal capillary bed is diverted to these shunts, bypassing the gastric and duodenal mucosa. This leads to mucosal ischemia during severe stress, lasting hours or even days, ultimately causing significant injury. When necrotic areas form in the ischemic mucosa, stress ulcers develop. At this stage, the digestive action of hydrochloric acid and pepsin can accelerate ulcer formation, as ischemic mucosa is more susceptible to digestion than normal mucosa. Another possible cause of ischemic injury to the gastric and duodenal mucosa is acute thrombosis in mucosal vessels due to disseminated intravascular coagulation (DIC). DIC is often a complication of severe sepsis or burns, which may explain the high incidence of stress ulcers in these patients.
The primary manifestation of stress ulcers is bleeding, typically occurring 2–15 days after the onset of the underlying disease and often difficult to control. This is because stress ulcers develop rapidly, and the underlying blood vessels fail to form thrombi. Additionally, perforation may occur. In some cases, only upper abdominal pain is present.
The diagnosis of stress ulcers relies mainly on emergency endoscopy. Characteristically, these ulcers are multiple, superficial, irregular, and located in the upper gastric body, measuring 0.5–1.0 cm or even larger. They heal without scarring.
bubble_chart Auxiliary Examination
(1) Endoscopy Whether using fiberoptic gastroscopy or electronic gastroscopy, both serve as primary methods for diagnosing peptic ulcers. Under direct endoscopic visualization, peptic ulcers typically appear round, oval, or linear, with sharp edges and a relatively smooth surface covered by a grayish-white or grayish-yellow fibrin membrane. The surrounding mucosa shows congestion, edema, and slight elevation (Figures 1, 2).
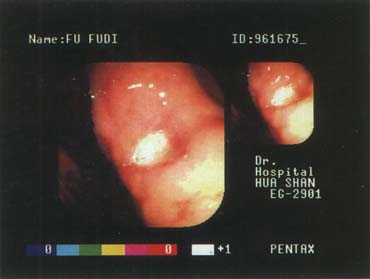
Figure 1A: Gastric angle ulcer, 0.6×0.5 cm (active stage)

Figure 1B: Gastric angle ulcer, 0.8×0.5 cm (active stage)

Figure 2A: Duodenal bulb ulcer, 0.5×0.6 cm (active stage, with blood crust)
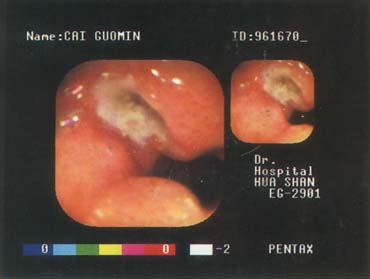
Figure 2B: Duodenal bulb ulcer, 0.7×0.5 cm (active stage)
Japanese scholars classify the endoscopic manifestations of peptic ulcers into the following stages:
Active stage (Stage A), further divided into A1 and A2.
A1: Round or oval, with a central white coating, often accompanied by minor bleeding, surrounding redness, and inflammatory edema.
A2: The ulcer surface is covered with yellow or white fibrin, without bleeding, and the surrounding inflammatory edema subsides.
Healing stage (Stage H), further divided into H1 and H2.
H1: Swelling around the ulcer disappears, the mucosa turns red, accompanied by newly formed capillaries.
H2: The ulcer becomes shallower and smaller, with surrounding mucosal folds.
Scarring stage (Stage S), also divided into S1 and S2.
S1: The white coating of the ulcer disappears, and newly formed red mucosa appears (red scar stage).
S2: The red color gradually turns white (white scar stage).
(2) X-ray Barium Meal Examination The primary X-ray finding of peptic ulcers is a niche or crater, caused by barium suspension filling the ulcer's depressed area. In frontal view, the crater appears round or oval with smooth edges. A translucent ring may form due to inflammatory edema around the ulcer.
Gastric ulcers often show craters along the lesser curvature, with a spastic notch on the opposite side. Duodenal ulcers typically present with craters in the bulb, usually smaller than gastric ones. The crater is a direct sign of ulcer presence. Due to inflammation and local spasm around the ulcer, localized tenderness and irritability may be observed during X-ray examination. Healing and scar contraction can lead to local deformation, especially in duodenal bulb ulcers, which may appear cloverleaf-shaped or petal-like.
(3) Detection of HP infection The methods for detecting HP infection can be roughly divided into four categories: ① Direct examination of HP from gastric mucosal tissue, including bacterial culture, tissue smear or section staining for microscopic examination of bacteria; ② Measurement of gastric urease activity using methods such as the urease test, breath test, or gastric fluid urea nitrogen detection; ③ Serological testing for anti-HP antibodies; ④ Application of polymerase chain reaction (PCR) technology to measure HP-DNA. Bacterial culture is the most reliable method for diagnosing HP infection.
(4) Gastric Juice Analysis The basal acid output (BAO) in normal males and females averages 2.5 and 1.3 mmol/h, respectively (range: 0–6 mmol/h). In male and female duodenal ulcer patients, the average BAO is 5.0 and 3.0 mmol/h, respectively. When BAO exceeds 10 mmol/h, it often suggests the possibility of gastrinoma. After injection of pentagastrin at 6 μg/kg, the maximal acid output (MAO) in duodenal ulcer patients often exceeds 40 mmol/h. Due to overlapping gastric acid levels between various gastric diseases and normal individuals, gastric juice analysis serves only as a reference for ulcer diagnosis.
bubble_chart Treatment Measures
After the diagnosis of this disease, comprehensive treatment measures are generally adopted, including basic medical treatment, drug therapy, treatment of complications, and surgical treatment. The goals of treating peptic ulcers are: ① alleviating clinical symptoms; ② promoting ulcer healing; ③ preventing ulcer recurrence; ④ reducing complications. However, the various therapies currently available cannot alter the natural course of peptic ulcers or completely cure them.
(1) Basic Medical Treatment
1. Lifestyle Peptic ulcers fall under the category of typical psychosomatic diseases, where psychological and social factors play a significant role in their onset. Therefore, maintaining an optimistic mood, a regular lifestyle, and avoiding excessive stress and fatigue are crucial, whether during the active or remission stages of the disease. During the active ulcer phase, when symptoms are severe, bed rest for a few days to 1–2 weeks is recommended.
2. Diet Before the advent of H2 receptor antagonists, dietary therapy was once the sole or primary treatment for peptic ulcers. In 1901, Lenhartz noted that frequent small meals were beneficial for patients. Later, the Sippy dietary therapy was introduced and remained in clinical use for decades. The Sippy diet mainly consisted of milk, eggs, and cream, and later included some "soft," non-irritating foods, based on the principle that these foods could persistently dilute and neutralize gastric acid. The following dietary perspectives are held for peptic ulcer patients: ① Chew food slowly and avoid rushing; chewing increases saliva secretion, which dilutes and neutralizes gastric acid and may enhance the mucosal barrier; ② Maintain regular, timed meals to preserve the rhythm of normal digestive activity; ③ During the acute active phase, frequent small meals are advisable, with 4–5 meals per day, but once symptoms are controlled, a quicker return to the usual three meals per day should be encouraged; ④ Focus on nutritional intake without adhering to a special diet; ⑤ Avoid snacks between meals and refrain from eating before bedtime; ⑥ During the acute active phase, abstain from alcohol and tobacco, and avoid stimulants such as coffee beans, strong tea, concentrated meat broth, hot peppers, vinegar, and other irritating condiments or spicy beverages, as well as medications that damage the gastric mucosa; ⑦ Avoid overeating to prevent excessive dilation of the gastric antrum, which increases gastrin secretion.
3. Sedation For a small number of patients with symptoms such as anxiety, tension, or insomnia, short-term use of sedatives or tranquilizers may be considered.
4. Avoid Ulcer-Inducing Medications Patients should be advised to discontinue medications that induce or exacerbate ulcers or cause complications such as bleeding, including: ① Salicylates and non-steroidal anti-inflammatory drugs (NSAIDs); ② Adrenocortical hormones; ③ Reserpine. If medications such as Bi disease or similar Bi disease require the use of the above drugs, enteric-coated dosage forms or intermittent low-dose administration should be employed as much as possible. Concurrently, adequate acid-suppressing therapy and mucosal protective agents should be administered.
(2) Drug Therapy Medications for treating peptic ulcers primarily include acid-reducing drugs, drugs to eradicate Helicobacter pylori infection, and drugs that enhance gastric mucosal protection.
1. Acid-Reducing Drugs These include antacids and antisecretory agents.
Antacids react with hydrochloric acid in the stomach to form salts and water, thereby reducing gastric acid. There are many types, such as sodium bicarbonate, calcium carbonate, magnesium oxide, aluminum hydroxide, and magnesium trisilicate. Their therapeutic effects lie in: ① Binding and neutralizing H+, thereby reducing the back-diffusion of H+ into the gastric mucosa and also decreasing the amount of gastric acid entering the duodenum; ② Raising the pH of gastric juice, which reduces the activity of pepsin. Gastric pepsin is most active when the gastric pH is between 1.5 and 2.5.
Antacids are divided into two major categories: soluble and insoluble. Sodium bicarbonate belongs to the soluble type, while others are insoluble. The former provides fast pain relief, but with long-term or excessive use, the side effects are more significant. Antacids containing calcium, bismuth, or aluminum can cause constipation, while magnesium-based ones may lead to diarrhea. Therefore, two or more types of antacids are often combined into compound formulations to counteract their side effects.
Anti-secretory drugs mainly include two categories: histamine H2 receptor antagonists and proton pump inhibitors.
(1) Histamine H2 receptor antagonists: These selectively compete with H2 receptors, thereby reducing the production of cAMP7 in parietal cells and decreasing gastric acid secretion, making them effective in treating peptic ulcers.
(2) Proton pump inhibitors: The final step in gastric acid secretion involves the parietal cell membrane proton pump driving the exchange of H+ with K+ in the tubules. The proton pump is H+, K+-ATPase. Proton pump inhibitors can significantly reduce acid secretion stimulated by any factor.
2. Treatment of H. pylori infection: The primary treatment for H. pylori infection involves the use of bactericidal drugs. "Clearance" refers to the disappearance of H. pylori at the end of drug treatment, while "eradication" means no recurrence of H. pylori for at least 4 weeks after treatment. Clinically, achieving H. pylori eradication can greatly reduce the recurrence rate of peptic ulcers. In vitro drug sensitivity tests show that, under neutral pH conditions, H. pylori is most sensitive to penicillin, and highly sensitive to aminoglycosides, tetracyclines, cephalosporins, ofloxacin, ciprofloxacin, erythromycin, and rifampin. It shows grade II sensitivity to macrolides, nitrofurans, and chloramphenicol, but is highly resistant to vancomycin. However, H. pylori is grade II sensitive to bismuth salts.
3. Drugs that enhance gastric mucosal protection: It is known that weakened gastric mucosal protection is a significant factor in ulcer formation. Recent research suggests that strengthening gastric mucosal protection and promoting mucosal repair are key aspects of treating peptic ulcers.
(1) Colloidal bismuth subcitrate (CBS): Brand names include De-Nol, De-Nol, and De-Luo.
CBS is generally as effective as H2 receptor antagonists in treating peptic ulcers. CBS is safe at conventional doses, primarily acting in the stomach after oral administration, with only about 0.2% absorbed into the bloodstream. It is contraindicated in patients with severe renal insufficiency. A few patients may experience constipation, nausea, or transient elevation of serum transaminases.
(2) Prostaglandin E: This is a class of drugs recently used to treat peptic ulcers.
Prostaglandins have cytoprotective effects, enhancing the defensive capacity of the gastrointestinal mucosa, but their anti-ulcer action is primarily based on their inhibition of gastric acid secretion.
(3) Sucralfate: Sucralfate is a complex of sulfated disaccharides and aluminum hydroxide. In acidic gastric juice, it forms a sticky paste that adheres to the surface of the gastric and duodenal mucosa, with particularly strong adhesion to ulcer sites.
(4) Epidermal growth factor (EGF): EGF is a polypeptide secreted by the salivary glands, Brunner's glands, and pancreas. EGF is not absorbed by the intestines and resists protease digestion, playing a crucial role in mucosal defense and wound healing. EGF not only stimulates mucosal cell proliferation and maintains mucosal integrity but also increases the release of prostaglandins, somatostatin, and other factors. Parenteral EGF can also inhibit parietal cell activity and acid secretion induced by various stimuli.
(5) Somatostatin: Somatostatin inhibits gastrin secretion, thereby reducing gastric acid secretion, and works synergistically with prostaglandins to protect the gastric mucosa. It is mainly used to treat bleeding complications of gastroduodenal ulcers.
4. Prokinetic drugs In cases of peptic ulcer, if significant nausea, vomiting, and abdominal distension and fullness are observed, and laboratory tests reveal gastric retention, delayed emptying, bile reflux, or gastroesophageal reflux, prokinetic drugs should be administered concurrently. Examples include (1) Metoclopramide; (2) Domperidone; (3) Cisapride.
5. Choice of Drug Therapy Nowadays, there are numerous types of drugs available for treating peptic ulcers, and new medications continue to emerge. There is no unified standard for how to make a choice, but the following opinions can serve as clinical references.
(1) Principles of Drug Selection: Histamine H2 receptor antagonists can be used as the first-line drugs for gastric and duodenal ulcers. Antacids and sucralfate can also be employed as first-line treatments, but their efficacy is inferior to H2 receptor antagonists. The prostaglandin analogue misoprostol is primarily used to prevent NSAID-related ulcers. Omeprazole can be used as a first-line drug, but more often, it is reserved for refractory ulcers that fail to respond to other treatments. For HP-positive cases, dual or triple therapy should be adopted to eradicate HP infection.
(2) Treatment of Refractory and Intractable Ulcers: Ulcers that show no significant improvement after standard medical treatment—including persistent non-healing, symptom recurrence during maintenance therapy, or complications—are termed refractory ulcers. Duodenal ulcers that do not heal after 8 weeks or gastric ulcers that persist after 12 weeks of treatment are classified as intractable ulcers. In such cases, increasing the dose of H2 receptor antagonists or switching to omeprazole may be attempted, with the latter achieving healing in 90% of intractable ulcers. Combination therapy with bismuth and antibiotics to eliminate HP infection may also be effective for some intractable ulcers. If drug therapy fails, surgical intervention should be considered.
(3) Treatment of NSAID-Related Ulcers: Aspirin and other NSAIDs inhibit prostaglandin synthesis in the mucous membrane, weaken cytoprotective effects, and increase mucosal susceptibility to injury, leading to peptic ulcers, particularly gastric ulcers. A significant number of gastric ulcer patients, especially the elderly, have a history of NSAID use. NSAID-induced ulcers are often asymptomatic (50%), and many patients present with bleeding as the first symptom.
Once an NSAID-related ulcer occurs, NSAIDs should be discontinued or reduced in dose, or alternative medications should be used. H2 receptor antagonists are far less effective for such ulcers compared to conventional ulcers. Some studies suggest that omeprazole (40mg/day) is highly effective, promoting ulcer healing regardless of whether NSAIDs are discontinued. Misoprostol, either alone or in combination with H2 receptor antagonists, has been proven to aid ulcer healing.
(4) Prevention and Treatment of Ulcer Recurrence: Peptic ulcers are a chronic relapsing condition, with approximately 80% of ulcers recurring within one year after healing and a 100% recurrence rate within five years. Preventing recurrence remains an unresolved issue. It is recognized that smoking, gastric hypersecretion, long disease duration, prior complications, ulcerogenic drug use, and Helicobacter pylori infection are significant risk factors for ulcer recurrence. Clinically, each peptic ulcer patient should undergo thorough history analysis and relevant tests to eliminate or minimize these risk factors as much as possible.
(5) Maintenance therapy for peptic ulcer: Due to the high recurrence rate after discontinuation of treatment for peptic ulcer, the relatively high incidence of complications, and the natural course lasting 8–10 years, drug maintenance therapy is an important measure. The following three regimens are available for selection: ① Standard maintenance therapy: Suitable for patients with frequent recurrence, persistent unrelieved symptoms, multiple risk factors, or complications. Maintenance methods: Take cimetidine 400 mg, ranitidine 150 mg, or famotidine 20 mg once at bedtime, or take sucralfate 1 g orally twice daily. The ideal duration of standard long-term maintenance therapy is difficult to determine, but most recommend at least 1–2 years. For elderly patients or those for whom ulcer recurrence may have serious consequences, lifelong maintenance may be considered. ② Intermittent full-dose therapy: When patients experience severe symptom recurrence or endoscopic evidence of ulcer recurrence, a full-dose course of treatment can be administered. Reports indicate that over 70% of patients achieve satisfactory results with this method. This approach is simple, convenient, and easily accepted by most patients. ③ On-demand therapy: This method involves administering short-term treatment when symptoms recur and discontinuing medication once symptoms resolve. For symptomatic patients, short-term drug therapy aims to control symptoms while allowing the ulcer to heal spontaneously. In fact, a considerable number of peptic ulcer patients discontinue medication on their own once symptoms disappear. Although ulcer healing is slower with on-demand therapy, the overall efficacy is not significantly different from full-course treatment. This method is not suitable for the following cases: patients over 60 years old, those with a history of ulcer bleeding or perforation, those with recurrence more than twice a year, or those with other serious comorbidities.
(3) Treatment of Complications
1. Massive Hemorrhage Massive hemorrhage caused by peptic ulcer disease often leads to peripheral circulatory failure and hemorrhagic anemia, requiring emergency treatment: ① Blood transfusion and fluid infusion to replenish blood volume, correct shock, and stabilize vital signs are critical steps; ② Simultaneously administer systemic hemostatic drugs, such as somatostatin diluted to 25μg for intravenous drip, followed by 250μg per hour for 24–48 hours to achieve hemostasis. Histamine H2 receptor antagonists can reduce gastric acid secretion, aiding hemostasis and ulcer healing. Options include cimetidine 0.8g/day or famotidine 40mg/day, dissolved in 500ml of glucose solution for intravenous drip. Proton pump inhibitors like omeprazole 40mg/day may also be added to the infusion; ③ Endoscopic local hemostasis can be achieved by spraying 1% adrenaline solution, 5% Monsel's solution, thrombin 500–1000u, or reptilase 1–2ku. Alternatively, inject 1% ethoxysclerol, hypertonic saline-adrenaline, or reptilase into the bleeding site. Electrocautery, microwave, or laser therapy may also yield good results.
The following conditions warrant emergency or imminent surgical intervention: ① Elderly or middle-aged patients with preexisting hypertension or arteriosclerosis, where massive hemorrhage is difficult to control; ② Recurrent massive hemorrhage from peptic ulcer; ③ Persistent bleeding unresponsive to aggressive medical treatment; ④ Massive hemorrhage combined with pyloric obstruction or perforation, where medical therapy is often ineffective.
2. Acute Perforation In cases of acute perforation due to gastroduodenal ulcers, fasting and gastric tube insertion to aspirate gastric contents are necessary to prevent secondary peritoneal infection. Small perforations without peritonitis may be managed non-surgically. Perforations occurring after a meal, often accompanied by diffuse peritonitis, require emergency surgery within 6–12 hours. Chronic perforations progress slowly, involving adjacent organs and leading to adhesions or fistula formation, necessitating surgical intervention.
3. Pyloric Obstruction In the initial stage of functional or organic pyloric obstruction, treatment methods are similar and include: ① Intravenous fluids to correct edema, electrolyte imbalances, or metabolic alkalosis; ② Continuous gastric tube aspiration for 72 hours, followed by gastric lavage 4 hours after dinner each day to relieve gastric retention and restore gastric tone; ③ If gastric retention is reduced to less than 200ml after lavage, indicating near-normal gastric emptying, a liquid diet may be introduced; ④ Severely malnourished or emaciated patients should receive total parenteral nutrition early; ⑤ Oral or injectable histamine H2 receptor antagonists; ⑥ Prokinetic agents like domperidone or cisapride may be used, but anticholinergic drugs such as atropine or belladonna are contraindicated as they relax the stomach and impair emptying, worsening gastric retention.
(4) Surgical Treatment Most peptic ulcers respond to aggressive medical therapy, with symptom relief and ulcer healing. Eradicating H. pylori infection and maintaining medication can prevent recurrence. Surgical treatment is primarily indicated for: ① Acute ulcer perforation; ② Penetrating ulcers; ③ Massive or recurrent hemorrhage unresponsive to medical therapy; ④ Organic pyloric obstruction; ⑤ Gastric ulcers with suspected or confirmed malignancy; ⑥ Refractory or intractable ulcers, such as those in the pyloric canal or postbulbar region.
Peptic ulcer is a chronic sexually transmitted disease with a tendency to recur, and the course can last for ten to twenty years or even longer. However, many cases do not recur after multiple episodes. Many patients experience repeated attacks but never develop complications, while others have mild symptoms that go unnoticed or resolve without medication. This indicates that for most patients, the disease follows a pathological process with a favorable prognosis. However, in elderly patients, once massive bleeding occurs, the condition can become severe, and without proper treatment, the mortality rate can be as high as 30%. Postbulbar ulcers are more prone to massive bleeding and perforation. Patients with peptic ulcers complicated by pyloric obstruction or massive bleeding have an increased risk of recurrence. A small number of gastric ulcer patients may develop cancer, significantly worsening their prognosis.
It is crucial to eliminate and avoid factors that can trigger the onset of peptic ulcers, such as emotional stress, excessive fatigue, irregular lifestyle, poor dietary habits, smoking, and excessive alcohol consumption. After peptic ulcers are treated with medication to achieve symptom relief and ulcer healing, it is still necessary to continue maintenance-dose drug therapy for 1 to 2 years, which plays a positive role in preventing ulcer recurrence. For Helicobacter pylori (HP)-related gastroduodenal ulcers, effective antibacterial drugs should be administered alongside acid-reducing medications to eradicate HP infection, which is also a key measure in preventing ulcer recurrence. Additionally, conditions such as gastrinoma or multiple endocrine neoplasia, hyperparathyroidism, Meckel's diverticulum, and Barrett's esophagus are often associated with peptic ulcers and should be treated promptly.
(1) Massive hemorrhage is the most common complication of this disease, occurring in approximately 20–25% of patients, and is also the most frequent cause of upper gastrointestinal bleeding. It is more commonly associated with duodenal ulcers than gastric ulcers, and even more prevalent with postbulbar ulcers. In most cases of hemorrhage, the history of peptic ulcer is within one year, but after the first episode, the likelihood of a second or further episodes increases. Additionally, 10–15% of patients may present with massive hemorrhage as the initial symptom of peptic ulcer.
The clinical manifestations of peptic ulcer hemorrhage depend on the site, speed, and volume of bleeding. For instance, ulcers on the posterior wall of the duodenum often erode into the adjacent pancreaticoduodenal artery, leading to exceptionally rapid and massive hemorrhage. In contrast, the anterior wall lacks large adjacent arteries, making massive hemorrhage less common. Bleeding from granulation tissue at the ulcer base or erosive bleeding around the ulcer mucosa typically results in minor and transient hemorrhage. In cases of rapid and voluminous bleeding, hematemesis and melena are observed. If the bleeding is slow and persistent, it may manifest as gradually developing hypochromic microcytic anemia and positive fecal occult blood. Melena is more common than hematemesis in duodenal ulcer hemorrhage, whereas both occur with similar frequency in gastric ulcer hemorrhage. Sudden massive blood loss can lead to dizziness, blurred vision, weakness, thirst, palpitations, tachycardia, hypotension, syncope, or even shock due to a sharp reduction in blood volume. Before hemorrhage occurs, upper abdominal pain often worsens due to sudden exacerbation of local congestion in the ulcer. After bleeding, the pain may alleviate as congestion subsides and the alkaline blood neutralizes and dilutes gastric acid.
Diagnosis is generally straightforward based on the history of peptic ulcer and clinical manifestations of bleeding. For atypical or diagnostically challenging cases, emergency endoscopy within 24–48 hours of bleeding is recommended, with a diagnostic accuracy exceeding 90%, enabling timely diagnosis and treatment.
(2) Perforation: When an ulcer penetrates the serosal layer and reaches the free peritoneal cavity, it causes acute perforation. If the ulcer penetrates and adheres to adjacent organs or tissues, it is termed a penetrating ulcer or chronic ulcer perforation. Perforations on the posterior wall or small perforations causing localized peritonitis are referred to as subacute perforations.
In acute perforation, duodenal or gastric contents spill into the peritoneal cavity, leading to acute diffuse peritonitis, characterized by sudden severe abdominal pain. The pain typically starts in the right upper or mid-upper abdomen and rapidly spreads to the periumbilical region and then the entire abdomen. Irritation of the diaphragm by gastrointestinal contents may cause referred pain to one shoulder (usually the right). If the spilled contents flow along the mesenteric root into the right lower pelvis, pain may localize to the right lower abdomen, mimicking acute appendicitis perforation. Pain worsens with movement, coughing, etc., so patients often lie still with legs drawn up. Nausea and vomiting frequently accompany the pain. Patients appear restless, pale, with cold, clammy extremities and tachycardia. If perforation occurs after a meal, extensive spillage causes marked abdominal rigidity, generalized tenderness, and rebound tenderness. With lesser spillage, rigidity and tenderness may be confined to the mid-upper abdomen. Bowel sounds diminish or disappear. Reduced or absent liver dullness indicates pneumoperitoneum. If gastrointestinal contents reach the pelvis, rectal examination may reveal tenderness in the right rectal pouch. Peripheral blood leukocyte and neutrophil counts rise. Abdominal X-ray often shows subdiaphragmatic free air, confirming gastrointestinal perforation, though its absence does not rule out perforation. In severe perforations or when the ulcer penetrates the pancreas, serum amylase may rise, though usually not exceeding five times the normal value.
Subacute or chronic perforations cause less severe symptoms than acute perforations, often resulting in localized peritonitis, intestinal adhesions, or obstruction, with improvement observed within a short period.
(3) Pyloric Obstruction Mostly caused by duodenal ulcer, but can also occur with prepyloric and pyloric canal ulcers. The cause is usually due to inflammatory congestion, edema around the ulcer during the active phase, or reflex-induced pyloric spasm. This type of pyloric obstruction is temporary and may resolve as the ulcer improves; it responds to medical treatment, hence termed functional or medical pyloric obstruction. Conversely, obstruction caused by ulcer healing, scar formation, scar tissue contraction, or adhesion to surrounding tissues blocking the pyloric passage is persistent and cannot resolve without surgical intervention, termed organic or surgical pyloric obstruction. Due to gastric retention, patients may experience upper abdominal fullness and discomfort, often accompanied by reduced appetite, belching, acid reflux, and other digestive symptoms, especially after meals. Vomiting is the main symptom of pyloric obstruction, typically occurring 30–60 minutes after eating. The frequency of vomiting is not high, usually once every 1–2 days. A single episode of vomiting may exceed 1L and contain fermented retained food. Patients may experience significant weight loss due to prolonged, repeated vomiting and reduced food intake. Abdominal pain is not always present; if it occurs, it is more likely in the early morning and lacks rhythmicity. Due to repeated large-volume vomiting, large amounts of H+ and K+ are lost, potentially leading to metabolic alkalosis, accompanied by shortness of breath, limb weakness, dysphoria, restlessness, and even hand-foot convulsions. On an empty stomach, upper abdominal fullness, counterflow of liver qi, visible gastric peristalsis, and a splashing sound in the upper abdomen are characteristic signs of pyloric obstruction.
(4) Malignant Transformation The issue of gastric ulcer malignant transformation remains a subject of debate. It is generally estimated that the incidence of gastric ulcer malignant transformation is only 2-3%, whereas duodenal bulb ulcers do not lead to malignant transformation.
This disease should be differentiated from the following conditions:
(1) Stomach cancer The differentiation between benign gastric ulcer and malignant ulcer is very important, and the key points for differentiation are shown in Table 18-10. The differentiation between the two can sometimes be difficult. The following situations should be given special attention: ① Middle-aged and elderly individuals who recently develop mid-epigastric pain, bleeding, or anemia; ② Patients with gastric ulcer whose clinical manifestations change significantly or who show no response to anti-ulcer medication; ③ Patients with gastric ulcer whose biopsy pathology shows intestinal metaplasia or atypical hyperplasia. Clinically, patients with gastric ulcer should be closely monitored with regular endoscopic follow-ups under active medical treatment until the ulcer heals.
Table 18-10 Key Points for Differentiating Benign Gastric Ulcer from Malignant Ulcer
| Benign ulcer | Malignant ulcer | ||
| Clinical manifestations | Age | Mostly young and middle-aged | Mostly middle-aged and older |
| Medical history | Periodic intermittent episodes | Progressive and continuous development | |
| Disease course | Longer, often measured in years | Shorter, often measured in months | |
| Systemic manifestations | Mild | Often obvious, with significant weight loss | |
| Antacid medication | Can relieve abdominal pain | Poor effect | |
| Gastroscopic examination
| Ulcer shape | Round or oval, regular | Irregular |
| Ulcer edge | Punched-out, sharp and smooth, congested | Uneven, tumor-like protrusion, hard and brittle, may erode and bleed | |
| Base tongue coating color | Smooth, clean, with gray-white or gray-yellow coating | Uneven, dirty coating, bleeding, island-like remnants | |
| Surrounding mucosa | Soft, folds often converge toward the ulcer | Shows cancerous infiltration, thickening, often with nodular protrusions, interrupted folds | |
| Gastric wall peristalsis | Normal | Weakened or absent | |
| X-ray examination
| Niche diameter | Mostly <2.5 cm | Mostly >2.5 cm |
| Niche shape | Often round or oval | Often triangular or irregular | |
| ulcer margin | Smooth | Irregular | |
| Location of niche | Outside the gastric cavity | Inside the gastric cavity | |
| Surrounding mucous membrane | The mucosal folds are uniform in thickness and soft, with a low-density transparent band around the niche caused by inflammatory edema. The ulcer orifice often shows a 1–2 mm translucent fine line, known as the Hampton line. | Due to cancerous infiltration, it becomes raised into nodular or polypoid shapes, with thickened, irregular, and rigid mucous membrane. The folds are interrupted, with club-shaped or tapered ends, rough edges, and the niche lacks a translucent zone or the Hampton line. | |
| Gastric peristalsis | Normal | Weakened or absent | |
| Other Examinations | Fecal occult blood | May be positive during the active phase, turning negative after treatment. | Often persistently positive. |
| Gastric acid analysis | Normal or low gastric acid, without true achlorhydria. | Achlorhydria is more common. |
(2)Chronic gastritis: This condition also presents with chronic upper abdominal discomfort or pain, with symptoms resembling peptic ulcers, but the periodicity and rhythm of episodes are generally atypical. Gastroscopy is the primary method for differentiation.
(3)Gastric neurosis : This condition may present with upper abdominal discomfort, nausea, vomiting, or symptoms mimicking peptic ulcers, but it is often accompanied by prominent systemic neurotic symptoms, with emotional fluctuations closely related to the onset. Endoscopy and X-ray examinations reveal no significant abnormalities. (4)Cholecystitis and gallstones
: More common in middle-aged women, it typically presents with intermittent, episodic right upper abdominal pain, often radiating to the right scapular region, and may include biliary colic, fever, jaundice, and Murphy's sign. Consumption of greasy foods often triggers it. Diagnosis can be made via ultrasound.
(5)Gastrinoma: Also known as Zollinger-Ellison syndrome, this condition presents with refractory multiple ulcers or ectopic ulcers, which often recur after subtotal gastrectomy, accompanied by diarrhea and significant weight loss. Patients have non-beta cell tumors in the pancreas or hyperplasia of gastric antrum G cells, elevated serum gastrin levels, and markedly increased gastric acid secretion.

