| disease | Thoracic Spinal Tuberculosis with Paravertebral Abscess Rupturing into the Lung Cavity |
Paravertebral abscesses penetrating into the lungs account for about 10% of patients with thoracic vertebral subcutaneous nodes. Chest X-rays are often misdiagnosed as pulmonary subcutaneous nodes, hilar lymph node subcutaneous nodes, or pneumonia, and in older individuals, they may be misdiagnosed as lung cancer. The thoracic vertebral lesions are mostly located at T8-10, with abscesses predominantly penetrating the right lung, accounting for 87% of cases.
bubble_chart Clinical Manifestations
In addition to the specific symptoms and signs of subcutaneous nodules along the spine, half of the patients experience respiratory symptoms. Mild cases present with symptoms similar to general bronchitis, while severe cases exhibit an irritating cough that worsens with changes in body position. Sputum is mostly white and frothy, occasionally containing small caseous lumps. A few cases may involve expectoration of blood or purulent sputum, and rarely, coughing up sequestra. When the superficial lung is affected, fine crackles may be heard in the affected area. Large areas of the lung field can be involved, leading to signs of lung excess.
bubble_chart Auxiliary Examination
1. Chest X-ray: A vaguely enlarged paravertebral shadow is seen in the mediastinum, protruding from the mediastinum into the lung field, presenting as a mass-like shadow with either clear or indistinct boundaries. There may be scattered patchy bronchial shadows in the ipsilateral or bilateral lung fields. The lesion may sometimes involve one lobe of the lung. In cases where the affected area is small, the chest X-ray may fail to show it, accounting for 12.7% of cases.
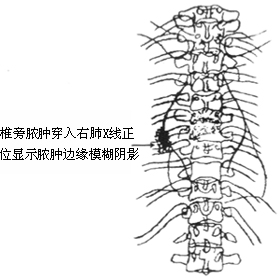
2. Thoracic X-ray (anteroposterior view): The shadows formed by abscesses penetrating the lungs and overlapping with paravertebral abscess shadows can be summarized as follows: ① In 35% of cases, the paravertebral shadow corresponding to the abscess penetrating the lung shows indistinct edges. ② In 33% of cases, patchy or linear projections of the lung lesion connect or overlap with the edge of a unilateral paravertebral abscess. ③ In 6.3% of cases, the unilateral paravertebral abscess shadow appears as a triangular protrusion (Figure 1). ④ In 25.4% of cases, there is no significant difference from the typical paravertebral shadow.
3. Posterior mediastinum anteroposterior tomography: Tomography is more significant for early diagnosis, especially in cases where the abscess penetrates the left lung. When the X-ray findings are suspicious but inconclusive, CT scanning is highly valuable for definitive diagnosis and differential diagnosis.
Based on the medical history, signs, and X-ray findings, the diagnosis is generally not difficult.
bubble_chart Treatment Measures
The principle for treating thoracic vertebral subcutaneous nodes is to first undergo anti-subcutaneous node drug therapy, followed by elective surgery after the pulmonary lesions have improved and been absorbed. For patients complicated with paraplegia, surgery should be performed earlier as appropriate.
1. Anesthesia General anesthesia with bronchial intubation can prevent intraoperative dissemination of lesions to the contralateral lung.
2. Position Lateral decubitus position, with the affected side upward.
3. Operative Steps
(1)Incision A posterolateral thoracotomy incision should be chosen, taking into account the locations of both the thoracic vertebral and pulmonary lesions to determine the appropriate level for the thoracotomy. Generally, for lesions in the upper lobe, a fifth rib incision is used, while for the middle or lower lobes, a sixth rib bed thoracotomy is preferred.
(2)Surgical Method Upon entering the thoracic cavity, extensive adhesions are often encountered. Fibrinous membrane-like adhesions are easily separated, whereas cord-like adhesions of larger size often contain blood vessels and should be clamped, cut, and ligated to prevent bleeding. Dense fibrous adhesions require gradual clamping, cutting, and ligation with vascular forceps. Fibrous adhesions at the lung apex or posterior chest wall may involve the subclavian vessels, brachial plexus, superior vena cava, or azygos vein. During left-sided thoracotomy, care should be taken to protect the innominate vein, main stirred pulse, left common carotid artery, and left subclavian stirred pulse. Adhesions near the mediastinum and hilum are usually less dense, and diaphragmatic pleural adhesions rarely contain large vessels. Dissection typically begins at the weakest point of adhesion, progressing sequentially upward, downward, anteriorly, and posteriorly. The extent of separation should be sufficient to address the vertebral and pulmonary lesions, without the need for extensive dissection. Areas where paravertebral abscesses penetrate the lung are difficult to separate, and local lung infiltration or cavity formation may occur. In severe cases, paravertebral abscesses may communicate with dilated bronchi.
Pulmonary lesions can be managed in the following four ways, depending on their nature and extent: ① No special treatment is needed for pulmonary lesions if the diameter of the local inflammatory mass is less than 2 cm, with no pus, caseation, or cavity formation on the surface. ② Pulmonary lesion debridement: For inflammatory masses approximately 2 cm in diameter containing pus, caseous material, or granulation tissue, debridement is performed. If a small cavity forms, especially with fistula disease and air, interrupted full-thickness sutures with silk thread should be applied, ensuring no dead space remains in the lung. ③ Wedge resection is suitable for small caseous nodules or cavities at the lung periphery. ④ Lobectomy is indicated for extensive lesions, those complicated by bronchiectasis, or cases of paravertebral abscess-bronchial fistula.(3)Postoperative Management Ensure the patient’s airway remains unobstructed, and intensify anti-subcutaneous node therapy along with treatment for general suppurative infections. Closely monitor for bronchial dissemination or bronchopleural fistula. Maintain the patency of the thoracic drainage tube, which is typically removed 72–96 hours postoperatively. If bloody or pale yellow serous fluid continues to drain, retain the tube until drainage ceases. Other management measures are the same as for debridement of thoracic vertebral subcutaneous node lesions.
Concurrent paraplegia.
It should be differentiated from lobar pneumonia, atypical pneumonia, hilar lymph node subcutaneous node, lung cancer, and mediastinal tumors.




