| disease | Idiopathic Scoliosis |
Scoliosis of unknown cause during growth and development is called idiopathic scoliosis. Based on age characteristics, idiopathic scoliosis is generally classified into three types: infantile (0–3 years old); juvenile (4–9 years old); and adolescent (10–16 years old). According to the anatomical location of the apical vertebra of the spinal curvature, it can also be divided into: ① Cervical curve: the apical vertebra is between C1 and C6. ② Cervicothoracic curve: the apical vertebra is between C7 and T1. ③ Thoracic curve: the apical vertebra is between T2 and T11. ④ Thoracolumbar curve: the apical vertebra is between T12 and L1. ⑤ Lumbar curve: the apical vertebra is between L2 and L4. ⑥ Lumbosacral curve: the apical vertebra is at L5 or S1.
bubble_chart Etiology
Since idiopathic scoliosis accounts for the vast majority of scoliosis cases, understanding its disease cause is of great significance for prevention and treatment. Therefore, over the years, people have been committed to exploring the disease cause of idiopathic scoliosis, but its exact cause has not yet been identified.
In 1979, Herman demonstrated that patients with idiopathic scoliosis have labyrinthine function injury. In 1984, Yamada also conducted balance function tests on idiopathic scoliosis patients, with results showing that 79% had significant balance dysfunction, compared to only 5% in the control group. Wyatt also found significant vibration imbalance in scoliosis patients, suggesting central disturbances in the posterior column pathways of these patients. However, these studies did not clarify the relationship between idiopathic scoliosis and balance disorders, nor did they explain the disease cause of idiopathic scoliosis itself.
Observations have revealed that the height of idiopathic scoliosis patients is greater than that of their normal peers. The author's 1984 survey also yielded the same results. This has prompted investigations into the relationship between growth hormone and idiopathic scoliosis. However, conclusions from different authors vary, and the role of growth hormone levels remains a contentious issue. More literature discusses the relationship between paravertebral muscles and idiopathic scoliosis, with examinations of paravertebral muscles including muscle spindles, muscle fiber morphology, muscle biochemistry, electromyography, and levels of calcium, copper, and zinc. Although abnormalities have been found, none directly elucidate its disease cause. Studies have also explored familial and twin cases of scoliosis to investigate genetic factors, but the majority of patients cannot be explained by a single genetic abnormality. Therefore, the disease cause of idiopathic scoliosis remains an important subject for future research.bubble_chart Clinical Manifestations
1. Infantile Type
Infantile scoliosis refers to structural scoliosis that appears before the age of 3. Idiopathic scoliosis at this stage is relatively rare. Its characteristics include a higher prevalence in males than females, predominantly left-sided thoracic curvature, and frequent association with other deformities, the most common being plagiocephaly, followed by intellectual disability or congenital hip dislocation. During examination, the infant is suspended by the armpits to observe the stiffness or flexibility of the curvature. A neurological examination is performed to assess muscle tone (hypertonia or hypotonia) and identify other congenital anomalies. Full-length anteroposterior and lateral spinal radiographs are taken in both suspended and supine positions to measure the Cobb angle, Mehta sign, and rib-vertebra angle difference (RVAD). The rib-vertebra angle difference is defined as follows: at the apex of the thoracic curve, a line perpendicular to the endplate is drawn from the center of the vertebral body, and another line is drawn along the central axis of the corresponding rib head and neck. The angle formed by these two lines is the rib-vertebra angle (Figure 1A). In a normal spine, the RVAD on both sides is 0. In scoliosis, the rib-vertebra angle on the convex side is smaller than that on the concave side, resulting in an RVAD greater than 0. Additionally, Mehta described two signs: - **Mehta Sign I**: On an anteroposterior radiograph, the rib head does not overlap with the vertebral body in early infantile scoliosis (Figure 1B). - **Mehta Sign II**: The rib head on the convex side overlaps with the vertebral body (Figure 1C). A progression from Mehta Sign I to Sign II indicates worsening scoliosis. Mehta used these signs and the RVAD to classify infantile idiopathic scoliosis into resolving and progressive types, which provides prognostic value for predicting the outcome of infantile scoliosis.
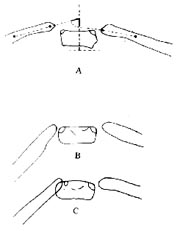
**Figure 1**: Rib-vertebra angle (A), Mehta Sign I (B), and Mehta Sign II (C).
2. Juvenile Type
Juvenile idiopathic scoliosis occurs between the ages of 3 and adolescence, accounting for approximately 15% of cases. Some of these cases may represent undetected infantile scoliosis before the age of 3, often presenting as left-sided thoracic curvature. However, scoliosis developing between 7 and 10 years of age typically exhibits characteristics similar to adolescent scoliosis. Koop (1988) reported that juvenile idiopathic scoliosis is most commonly a simple right-sided thoracic curvature, followed by thoracolumbar double curvature.
3. Adolescent Type
Adolescence is a rapid stage of skeletal growth and development, as well as a period when scoliosis progression accelerates. There are many factors influencing scoliosis progression, including not only age but also the type of curvature, menarche, Risser sign, and Harrington factor. Lonstein's epidemiological survey reported varying incidence rates of scoliosis across different age groups: 2.5% for those under 9 years old, 4.1% for 10-year-olds, 8.8% for 11-year-olds, 19.8% for 12-year-olds, 24.5% for 13-year-olds, 19.5% for 14-year-olds, and 20.8% for those aged 15 and above, illustrating the relationship between age and progression. Based on survey results from 1970 to 1979, Lonstein concluded that the progression of the scoliosis angle is positively correlated with the initial angle size and inversely correlated with age and Risser sign. For example, among patients with an initial scoliosis angle of less than 19° and a Risser sign of grade 2, 3, or 4 (or degrees I, II, III, IV), only 1.6% experienced progression. In contrast, another group with a scoliosis angle of 20°–29° and a Risser sign of grade 0 (unossified) or grade 1 (degree I) had a progression rate as high as 68%. Additionally, the Harrington factor—calculated by dividing the number of vertebral segments involved in the curvature by the scoliosis angle—also relates to progression. The average value for non-progressive cases is 2.7, while a value exceeding 3.4 indicates a progressive type. Among single factors, the type of scoliosis also plays a role. Double curvatures are more likely to progress than single curvatures, and among double curvatures, thoracolumbar and lumbar scoliosis are more prone to progression than thoracic scoliosis. Therefore, treatment methods should be selected based on the patient's age, type of scoliosis, and clinical manifestations.
1. Infantile Type
The treatment plan should first be formulated based on X-ray findings. If the X-ray shows Mehta's sign in the initial stage (first stage) with a rib-vertebral angle difference of less than 20 degrees, it is considered the resolving type and generally does not require treatment. However, X-ray follow-up examinations should be conducted every six months until complete resolution is achieved. Subsequently, X-rays should be taken every 1–2 years for review until skeletal maturity is reached. If the X-ray shows Mehta's sign in the intermediate stage (second stage) with a rib-vertebral angle difference greater than 20 degrees, early treatment is necessary. Correction under anesthesia with a plaster cast may be considered, followed by Milwaukee brace fixation as the patient grows. If the brace fails to control progression, subcutaneous internal fixation may be considered, but fusion should be avoided. Spinal fusion is only considered as a last resort for rigid scoliosis that cannot be controlled by conservative methods.
2. Juvenile Type
The incidence of idiopathic scoliosis varies by age and gender, but most scholars agree that juvenile scoliosis is more common in females than males, with right thoracic curves being predominant. The indications for treating juvenile idiopathic scoliosis are broader than those for adolescent scoliosis because juvenile curves tend to worsen. For curves below 20 degrees, physical therapy is recommended, with standing X-rays taken every six months for follow-up observation. For thoracic or double curves of 20–40 degrees, a Milwaukee brace should be used, while thoracolumbar or lumbar curves should be treated with a thoracolumbosacral brace. If bracing fails to control progression and the curve exceeds 40 degrees but remains flexible with good correction potential, subcutaneous rod instrumentation may be considered. For rigid, poorly flexible curves, or if the Cobb angle cannot be controlled below 50 degrees despite bracing or subcutaneous rod treatment, spinal fusion may be considered. Otherwise, conservative treatment should be pursued as long as possible until the age of fusion.
3. Adolescent Type
Adolescent idiopathic scoliosis is the most common type, with a higher incidence in females and a predominance of right thoracic curves. The most critical aspect of treatment is assessing the patient's developmental stage using the Risser sign. For mature patients with curves below 20 degrees, no treatment is necessary. For immature patients, physical therapy is recommended, with X-rays taken every six months until maturity is reached. If the curve exceeds 25 degrees and growth is incomplete, early treatment with a Milwaukee brace or thoracolumbosacral brace, combined with physical therapy or electrical stimulation, should be initiated. The brace should be worn until spinal growth ceases and the Risser sign reaches grade IV or higher. For adolescent scoliosis with a Cobb angle exceeding 40 degrees and ongoing growth, conservative treatment should be abandoned in favor of spinal instrumentation and fusion, with Harrington instrumentation being the most commonly used.
For adult patients who developed scoliosis before skeletal maturity but sought treatment in adulthood, some authors note that thoracic curves between 50–80 degrees may still progress, while curves below 50 degrees or above 80 degrees are less likely to progress. They recommend surgical fusion for progressive thoracic scoliosis exceeding 50 degrees after skeletal maturity. For thoracolumbar curves exceeding 50 degrees, surgery may also be considered to prevent low back pain.
In summary, the treatment of idiopathic scoliosis should be tailored based on the patient's age, curve type, and other factors.





