| disease | Oral and Maxillofacial Soft Tissue Injury |
Oral and maxillofacial soft tissue injuries can occur alone or simultaneously with jaw and facial bone fractures. The clinical symptoms and treatment methods for various types of injuries each have their own characteristics.
bubble_chart Etiology
Injuries can be classified into abrasions, contusions, incised wounds, puncture wounds, crush injuries, lacerations, bites, and firearm wounds based on the cause and nature of the injury.
bubble_chart Clinical Manifestations
(1) Abrasion Wounds
Contusion is an injury to the subcutaneous and deep tissues without an open wound. Small blood vessels and lymphatic vessels in the injured area rupture, often leading to internal tissue bleeding, forming ecchymosis or even hematoma. The main characteristics are local skin changes, swelling, and pain. The treatment of contusion primarily involves stopping bleeding, relieving pain, preventing infection, promoting hematoma absorption, and restoring function. In the early stages, cold compresses and pressure bandages can be used to stop bleeding. If the hematoma is large, under sterile conditions, a thick needle can be used to aspirate the blood, followed by pressure bandaging. For hematomas that have already formed, after 1–2 days, hot compresses, physical therapy, or the application of Chinese medicinals can be used to promote absorption and dissipation. If the hematoma becomes infected, it should be incised to remove pus and necrotic blood clots, establish drainage, and use antibiotics to control the infection.
(2) Contusion Wounds
In this type of injury, the skin and soft tissues have already developed lacerations. Puncture wounds are small but deep, often forming blind tracts. The penetrating object can carry dirt and bacteria deep into the wound. Incised wounds have neat edges, and if large blood vessels are injured, significant bleeding can occur. If the facial nerve is severed, deviation of the mouth may result. The treatment for puncture and incised wounds should involve early surgical intervention, i.e., debridement.
(3) Incised and Puncture WoundsThese are caused by significant mechanical force tearing or avulsing tissues, such as when long braids are caught in machinery, leading to the avulsion of large sections of the scalp. In severe cases, the entire scalp, along with the auricle, eyebrows, and upper eyelid, may be torn off. Avulsion injuries are severe, with heavy bleeding, intense pain, and a high risk of shock. The wound edges are often irregular, with contusions in the subcutaneous tissue and muscles, and exposed bone surfaces are common. Lacerations should be promptly debrided and sutured in place. If the facial nerve is severed, deviation of the mouth may occur. The treatment for puncture and incised wounds should involve early surgical intervention, i.e., debridement.
(4) Lacerated Wounds
These are caused by significant mechanical force tearing or avulsing tissues, such as when long braids are caught in machinery, leading to the avulsion of large sections of the scalp. In severe cases, the entire scalp, along with the auricle, eyebrows, and upper eyelid, may be torn off. Avulsion injuries are severe, with heavy bleeding, intense pain, and a high risk of shock. The wound edges are often irregular, with contusions in the subcutaneous tissue and muscles, and exposed bone surfaces are common. Lacerations should be promptly debrided and sutured in place. If the avulsed tissue has viable blood vessels for anastomosis, immediate vascular anastomosis and tissue replantation should be performed. If no vessels are available for anastomosis, within 6 hours of the injury, the avulsed skin can be debrided and trimmed into full-thickness or split-thickness skin grafts for replantation. If the avulsed tissue flap is too severely injured or more than 6 hours have passed, making the tissue unusable, healthy tissue grafts should be harvested for free transplantation to cover the wound after debridement.
I. Debridement of Oral and Maxillofacial Injuries
As long as the general condition of the patient with oral and maxillofacial injuries permits, or after emergency treatment improves their condition, and if the necessary conditions are available, early surgical management of the local wound—i.e., debridement—should be performed as soon as possible. Debridement is a fundamental method for preventing wound infection and promoting healing.
(1) Wound Irrigation
Within 6–12 hours after bacteria enter the wound, they mostly remain in the superficial layers of the injured tissue and have not yet proliferated extensively, making them easier to remove through mechanical irrigation. First, cover the wound with sterile gauze and cleanse the surrounding skin with soapy water or saline solution. If there is grease, use gasoline or a detergent to wipe it clean. Then, under anesthesia, irrigate the wound with a large amount of physiological saline or 1–3% hydrogen peroxide solution, while scrubbing repeatedly with a gauze pad or soft brush to remove as much bacteria, dirt, tissue debris, or other foreign material as possible. During irrigation, further examination of the tissue injury can be performed.
(2) Wound Cleaning
After irrigation, disinfect the skin around the wound, drape it, and proceed with debridement. In principle, maxillofacial tissue should be preserved as much as possible. Except for clearly necrotic tissue, only minor trimming of the wound edges is generally required. Lacerations of the lips, tongue, nose, ears, and eyelids, even if largely detached or completely severed, should be preserved as much as possible if there is no infection or necrosis, and efforts should be made to suture them back into place, as they may still heal.
(3) Suturing
Due to the rich blood supply and strong regenerative capacity of oral and maxillofacial tissues, even within 24–48 hours post-injury, tight suturing can be performed after debridement. Even beyond 48 hours, as long as there is no obvious suppurative infection or tissue necrosis, thorough debridement can still be followed by tight suturing. For wounds at risk of infection, drainage may be placed inside the wound. Wounds with evident infection should not undergo initial (first-stage) suturing; instead, local wet compresses can be applied, and further treatment can proceed after infection control.
First, suture and close wounds connected to the oral cavity, nasal cavity, or maxillary sinus. Exposed bone surfaces should be covered with soft tissue whenever possible. Deep wounds should be sutured in layers to eliminate dead space. Facial wounds, in particular, should be sutured with fine needles and thin thread, ensuring precise edge alignment, especially for the lips, nose, and eyelids, where meticulous suturing is crucial.
If there is tissue loss, displacement, or conditions such as edema or infection preventing tight suturing after debridement, directional approximation sutures can be applied first to restore or approximate the tissue to its normal position as much as possible. Further suturing can be performed after infection control and swelling reduction. Common methods for directional approximation sutures include button mattress tension-reducing sutures or wire-and-bead directional sutures (Figures 1 and 2).
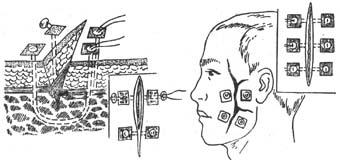
Figure 1: Button Mattress Directional Suture Method
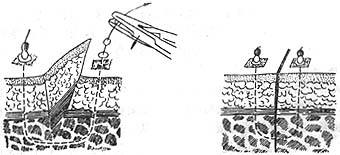
Figure 2: Wire-and-Bead Directional Suture Method
II. Special Considerations in Managing Soft Tissue Injuries of the Oral and Maxillofacial Region
(1) Lingual Injury
1. When there is tissue loss in the tongue, suturing should aim to preserve the tongue’s length, ensuring the sutured wound follows a longitudinal direction. Avoid folding the tip of the tongue backward during suturing to prevent shortening, which could impair tongue function. (Figure 3)
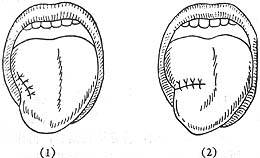
Figure 3 Suture of tongue injury (1) Correct suture (2) Incorrect suture
2. If there are wounds on the lateral side of the tongue adjacent to the gums or on the ventral side of the tongue adhering to the floor of the mouth, the wounds in each area should be sutured separately. If it is not possible to close all wounds, the tongue wound should be sutured first to prevent future adhesions that may affect tongue movement.
3. Tongue tissue is relatively fragile and highly mobile, making the sutured area prone to tearing. Therefore, thicker silk threads (such as No. 1 or No. 4) should be used for suturing. The needle should be inserted slightly farther from the wound edge and sutured deeper to include more tissue. A triple knot should be tied to prevent wound dehiscence or suture loosening. It is best to add a mattress suture.
(II) Penetrating buccal injury
The treatment principle for penetrating buccal injuries is to close the wound and eliminate the wound surface as much as possible.
1. For cases with no tissue defect or minimal defect, the oral mucosa, muscle, and skin can be sutured in layers.
2. For cases with minimal or no oral mucosal defect but significant skin defect, the oral mucosa should be tightly sutured to close the penetrating wound. Skin defects on the cheek should be immediately addressed with flap transfer, free skin grafting, or directional approximation sutures. If defects remain, reconstructive treatment can be performed later.
3. For larger full-thickness perforating defects of the cheek, the oral mucosa and skin edges can be directly sutured together to eliminate the wound surface. The remaining perforating defect can be treated with reconstructive surgery in the late stage [third stage] (Figure 4). If the injury and conditions permit, double-layer repair can be performed during debridement using pedicled flaps, free flaps, and skin grafting.

Figure 4 Suture method for full-thickness tissue defects of the cheek
(III) Palatal injury
For soft tissue lacerations of the hard palate, mucoperiosteal suturing is sufficient. For penetrating injuries of the soft palate, the nasal mucosa, muscle, and oral mucosa should be sutured separately. If there is tissue defect in the hard palate or communication with the nasal cavity or maxillary sinus, a nearby mucoperiosteal flap can be transferred to close the fistula and defect. Alternatively, relaxing incisions can be made on both sides of the hard palate, and the mucoperiosteal flap can be separated from the bone surface to approximate and suture the perforation (Figure 5). Exposed bone surfaces on the hard palate can heal on their own. If the palatal defect is too large for immediate repair, a palatal splint can be temporarily placed to separate the oral and nasal cavities, with surgical repair performed later.
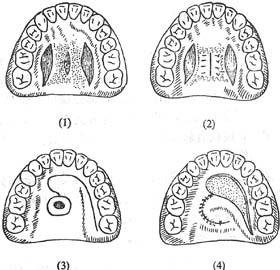
Figure 5 Suture method for penetrating palatal injury (1) Designing bilateral relaxing incisions and advancing the tissue toward the center after separation (2) Post-suture (3) Designing a rotating mucoperiosteal flap for the wound (4) Mucoperiosteal flap transfer for repair
(IV) Rupture of lips, tongue, ears, nose, and eyelids
For ruptures of the lips, tongue, ears, nose, and eyelids, if the detached tissue is still intact and the injury time does not exceed 6 hours, efforts should be made to suture it back to its original position. Before suturing, the detached tissue should be thoroughly cleaned and soaked in an antibiotic solution. The injured area should undergo debridement and be trimmed into a fresh wound surface, followed by meticulous suturing with fine needles and threads. Postoperative local warmth should be maintained, and systemic antibiotics should be administered.





