| disease | Osteoporosis (Surgery) |
Osteoporosis refers to a decrease in the amount of bone tissue per unit. The growth and development of bones begin during the embryonic period and continue for more than 20 years after birth. The quantity of bone in adults no longer changes, but bone metabolism continues uninterrupted, meaning the processes of bone formation and bone resorption are in balance. After the age of 40, bone formation remains unchanged, but bone resorption increases. Decades later, the amount of bone tissue is only half of what it was at age 30. Once bone density decreases to the point where it can no longer withstand the stresses of daily life, pathological fractures occur.
bubble_chart Etiology
(1) Postmenopausal and senile osteoporosis
(2) Hereditary osteoporosis
1. Osteogenesis imperfecta
2. Homocystinuria
(3) Osteoporosis caused by endocrine disorders
1. Hypogonadism
2. Hyperthyroidism
3. Hyperparathyroidism
4. Hyperadrenocorticism
(4) Diet-related osteoporosis
1. Calcium deficiency
2. Vitamin D deficiency
3. Vitamin C deficiency
4. Chronic alcoholism
(5) Drug-induced osteoporosis
1. Long-term heparin use
2. Long-term methotrexate use
(6) Disuse osteoporosis
(7) Osteoporosis caused by other diseases
1. Various chronic sexually transmitted diseases
2. Various intramedullary tumors (multiple myeloma, lymphoma, and leukemia)
(8) Idiopathic osteoporosis
1. Idiopathic juvenile osteoporosis
2. Idiopathic adult osteoporosis
bubble_chart Pathological Changes
There are many factors that can affect the amount of bone tissue.
(1) Systemic diseases Malabsorption, liver and kidney diseases, alcoholism, corticosteroid drugs, and insufficient sunlight exposure can all disrupt bone metabolism.
(2) Race and heredity White women, especially those from Northwestern Europe, have a high incidence of fracture osteoporosis, while the incidence is low in Black women.(3) Nutritional status This is related to the intake of calcium and vitamin D3. The daily calcium intake for children should be 400–700 mg, 1,300 mg for adolescents in the growth period, 700 mg for menopausal women, 1,500 mg for pregnant women, 2,000 mg for lactating women, and postmenopausal women need a daily calcium intake of 1,500 mg to prevent bone loss. Dairy products and leafy green vegetables are the main dietary sources of calcium; while high-protein diets and emaciation due to improper food can increase calcium loss in urine—doubling protein intake increases urinary calcium loss by 50%.
Half of the body's vitamin D3 comes from food, and the other half from sunlight exposure. Insufficient sunlight exposure in the elderly can lead to vitamin D3 deficiency. Young adults require 400 IU of vitamin D daily, while the elderly need 800 IU.
(4) Age and gender After the epiphyses close, the morphology of bones changes, and the areas of the bone membrane and endosteal membrane increase. After the age of 40, the endosteal membrane area increases rapidly, cortical bone quantity gradually decreases, and trabecular bone also diminishes, with this being more pronounced in women than in men. On average, bone loss is 0.5% per year. In the process of bone tissue reduction, the difference between genders is significant. The annual decline rate is 0.5–0.75% in men and 1.5–2% in women, with some cases even reaching 3%.
(5) Endocrine factors Postmenopausal osteoporosis is related to low estrogen levels. It has been confirmed that estrogen plays a key role in bone metabolism. Osteoporosis is also related to parathyroid hormone. In the elderly, the kidney's production of 1-25-(OH)2
D3 is weakened after parathyroid hormone administration, while osteoclasts remain highly responsive to endogenous parathyroid hormone, which is related to insufficient estrogen.(6) Activity and weight-bearing Mechanical weight-bearing stress is the primary external factor affecting bone development and remodeling. Inactive individuals are more prone to osteoporosis than active ones. During spaceflight, bone tissue loss can occur due to weightlessness. After 84 days in a weightless environment, the osteoporosis condition closely resembles disuse osteoporosis. It is now also believed that the loss of muscle contraction is a major cause of osteoporosis. For example, after a fracture, immobilization with a cast, nerve and spinal cord injuries, and prolonged bed rest can lead to osteoporosis.
bubble_chart Clinical Manifestations
Osteoporosis patients lose 30% of their bone mass from the spine, which is why they often seek medical attention due to spine fractures or proximal femur fractures. Spine fractures can be classified into three types: ① Thoracolumbar vertebral compression fractures. Minor trauma can lead to acute compression of the thoracolumbar vertebral body, and spontaneous vertebral compression may even occur without significant trauma. ② Lumbar compression fractures. ③ Diffuse spinal pain, which may indicate multiple microfractures. Proximal femur fractures include intracapsular femoral neck fractures and intertrochanteric fractures. The former is more common in individuals aged 65–75, while the latter occurs more frequently in older individuals, typically aged 75–85.
Radiographic findings include decreased bone density, with at least 30–50% of bone tissue already lost before the density decline becomes apparent; vertebral bodies exhibit biconcavity; tubular bone cortices become thinner, and the medullary cavity enlarges. Singh classified osteoporotic fractures into six grades based on changes in the trabeculae of the proximal femur. Grade 6 is normal, grades below 5 indicate osteoporotic fractures, and grades below 3 signify grade III osteoporotic fractures (Figure 1).
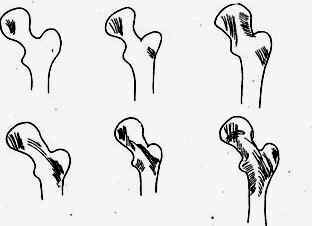
Figure 1 Singh's six-grade osteoporosis classification
After a vertebral compression fracture occurs, the following four manifestations may appear: ① Biconcave central compression fracture; ② Anterior wedge-shaped compression fracture; ③ Symmetrical transverse compression fracture; ④ Mixed-type fracture.
bubble_chart Auxiliary Examination
Laboratory tests generally show normal serum calcium and phosphorus levels, with a slight increase in serum alkaline phosphatase when fractures are present.
【Several Methods for Measuring Osteoporosis】
(1) Singh Index As previously mentioned.
(2) Hand Radiography to Measure Cortical Thickness of the Midshaft of the Second Metacarpal Under normal circumstances, the cortical bone thickness should account for at least half of the diameter at that site.
(3) Nosland-Cameson Single-Photon Absorptiometry Using 125I as the monoenergetic photon source, this method measures bone tissue content in limbs based on the difference in photon absorption between bone and soft tissues. Taking the radius as an example, under normal conditions, the proximal metaphysis of the radius consists of 95% cortical bone and 5% trabecular bone, while the distal metaphysis consists of 75% cortical bone and 25% trabecular bone. Recently, dual-photon absorptiometry has also been adopted, which can distinguish between fat and soft tissue components within the bone.
(4) Dual-Energy Quantitative CT Scanning Quantitative CT scanning can differentiate between fat, soft tissue, and bone tissue, while dual-energy quantitative CT scanning can further distinguish the soft tissue component (bone marrow) within the bone tissue.
(5) In Vivo Neutron Activation Analysis This method uses high-energy neutrons to activate calcium in the body from Ca48 to Ca49, and a gamma-ray counter measures the decay of Ca48. Since 99% of the body's calcium is stored in the bones, this method is highly accurate for determining whether there is a reduction in total bone tissue.
(6) Iliac Bone Biopsy This procedure involves three steps: ① First, administer 750 mg of tetracycline orally per day for 3 days to label the bone tissue. ② Perform an iliac bone biopsy 3 days later. ③ Process the bone sample without decalcification, prepare ultrathin sections (5–10μ), and perform morphological measurements. This method is not suitable as a routine examination.
bubble_chart Treatment Measures
(1) Acute Phase Treatment Once a vertebral fracture occurs, the patient should rest on a hard bed with a pillow placed under the knees to reduce mild purgation and stress on the lumbar region. Pay attention to bedsore care. Painkillers may be used. Exercise should begin once the pain subsides, with activity levels gradually increasing daily. Patients with severe pain may wear a brace.
(2) Methods to Increase Bone Tissue
1. Oral Calcium Supplements Calcium carbonate, calcium phosphate, calcium lactate, and calcium gluconate can all be used. Patients should be encouraged to drink plenty of water after taking oral calcium supplements to prevent urinary stones.
2. Vitamin D Supplementation It must be noted that high-dose vitamin D supplementation can cause hypercalcemia. For women around menopause, the daily dose is 400 units.
3. Estrogen Supplementation Suitable for women around menopause. The dose is 0.6mg daily. Long-term use may carry a risk of cancer and should not be used as a routine treatment method.
4. Exercise At least 30 minutes of walking daily is recommended, which allows for weight-bearing exercise and exposure to sunlight.
5. Sodium Fluoride Method Take sodium fluoride orally at 1mg/kg daily, divided into 36 doses. Calcium supplements must be taken simultaneously. Overdosing may lead to fluorosis. After 18 months of use, 90% of cases no longer experience fractures.
6. Other Medications These include bisphosphonates, calcitonin, and anabolic steroids such as stanozolol.




