| disease | Congenital Scoliosis |

**Figure 3** A. Unilateral unsegmented bone bar B. Combined with hemivertebra C. Hemivertebra with segmentation failure
There are many factors that influence the treatment of congenital scoliosis, such as the patient's age, gender, location of deformity, degree of scoliosis, segment length, type of deformity, flexibility, and progression, all of which are significant. Doctors should choose different treatment methods based on varying circumstances.
I. Non-surgical Treatment
Extensive experience has proven that congenital scoliosis differs from idiopathic scoliosis in that it does not respond to gymnastics therapy, physical therapy, exercise therapy, or electrical stimulation therapy. Risser Gypsum orthopedic treatment, due to the heaviness of the gypsum and frequent complications such as pressure sores, thoracic deformation, and reduced lung function, has largely been abandoned or rarely used nowadays. Therefore, brace therapy is the primary non-surgical treatment for congenital scoliosis. Below is a brief overview of the indications and efficacy of brace therapy.
Although brace therapy is the main or only non-surgical treatment for congenital scoliosis, not all cases are suitable for it. The indications are limited. Braces are suitable for patients who are not yet mature, whose deformities are progressively worsening, and who have long and flexible scoliotic segments. Braces are unnecessary for non-progressive cases and unsuitable for cases where the deformity has shown spontaneous improvement. For short and rigid segments, brace therapy is almost ineffective. Flexibility plays a crucial role in treatment selection. Therefore, before treatment, the degree of flexibility should be thoroughly assessed through examinations in standing, supine, traction, or lateral bending positions. Winter suggests that if the scoliosis is less than 50° and flexibility exceeds 50%, brace therapy generally yields good results. If the scoliosis is between 50° and 75° and flexibility is between 25% and 50%, brace therapy may be beneficial. However, for scoliosis exceeding 75° and flexibility below 25%, brace therapy is almost ineffective.
Two types of braces are commonly used:1. Milwaukee Brace Also known as the cervico-thoraco-lumbo-sacral orthosis (CTLSO) (Figure 1). It is suitable for treating cervicothoracic and thoracic scoliosis. For cervicothoracic scoliosis, a shoulder ring can be used, along with a lateral head support pad, applying a downward and inward pressure on the convex side of the shoulder and upper thoracic region, while applying a lateral counterforce on the opposite side at a higher level. For upper thoracic scoliosis, the lateral head support pad may be omitted, using only the shoulder ring or a trapezius pad. For mid-thoracic scoliosis, a standard thoracic pad is applied on the convex side. If the patient also has another primary or secondary lumbar scoliosis, a lumbar pad should be added.
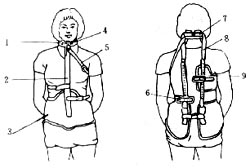
Figure 1 Milwaukee Brace (1. Neck ring 2. Support rod 3. Waistband 4. Neck ring clip 5. Belt 6. Lumbar support 7. Neck support 8. Support rod 9. Back support)
2. Thoraco-Lumbo-Sacral Orthosis (TLSO) (Figure 2) The TLSO is suitable for thoracolumbar scoliosis and scoliosis at lower levels. For congenital scoliosis with an apical vertebra at T10 or higher, the Milwaukee brace is used. For thoracolumbar scoliosis, a corrective force is applied on the convex side of the thoracolumbar region, while a counterforce is applied on the opposite side at a higher thoracic level. For lumbar scoliosis, the counterforce is not applied at the axilla but at the lower thorax.
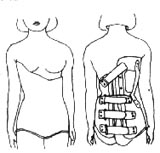
Figure 2 Thoraco-Lumbo-Sacral Orthosis (TLSO)
Brace treatment is a long-term and challenging therapeutic method that requires cooperation from both parents and patients. Patients are required to wear the brace full-time, with only one hour allowed each day for removal. Intermittent wear, partial-time wear, or seasonal wear is not permitted. The brace must be worn until skeletal maturity is reached and vertical growth ceases. Typically, the brace can be discontinued two years after reaching Risser sign grade 4. In the first year, the transition involves shifting from full-time wear to daytime wear and gradually switching to nighttime wear. The second year involves wearing the brace only at night. Premature or abrupt discontinuation of the brace may lead to worsening of the scoliosis.
II. Surgical TreatmentA single surgical method cannot address congenital scoliosis of different ages, types, and conditions. It is essential to analyze the specific situation and select the appropriate treatment method.
1. Simple Spinal Fusion
The primary goal of this surgery is not to correct the scoliosis but to stabilize the spine and prevent further progression of the curvature. It is particularly indicated for rigid cases where bracing fails to correct the deformity and the scoliosis continues to worsen. A simple posterior fusion should be performed. For unilateral unsegmented scoliosis, avoid excessive fusion of the mobile segments above and below the unsegmented area. Ensure sufficient bone grafting, preferably using autologous bone. If the patient is too young for iliac bone harvesting, allogeneic bone may be used as an alternative.
2. Posterior Fusion with Gypsum Correction
This method is suitable for younger patients (under 9 years old) who are not candidates for instrumentation correction, especially those with highly flexible and progressive scoliosis.
3. Traction Correction Followed by Instrumentation Fusion
For congenital scoliosis, preoperative slow, long-term traction can avoid sudden intraoperative correction and stretching, which is crucial for preventing spinal cord and nerve complications and improving the surgical correction rate. Gradually increase the traction preoperatively to monitor for numbness, pain, muscle tone, strength, and reflex changes. Once satisfactory correction is achieved, proceed with instrumentation and fusion. Preoperative myelography is necessary to rule out coexisting intraspinal anomalies. Intraoperative electrophysiological monitoring and wake-up tests are also required. Common corrective devices include Harrington and Luque instrumentation. However, due to the lack of interlaminar space in congenital scoliosis, passing sublaminar wires for Luque instrumentation can be challenging. Additionally, Luque devices lack the distraction capability of Harrington instrumentation, so they are often used in combination with Harrington devices rather than alone.
4. Epiphysiodesis
The principle is to destroy and fuse the convex-side epiphysis to halt overgrowth while preserving the concave-side epiphysis to allow continued growth. This typically involves anterior and posterior hemivertebral epiphyseal and facet joint fusion. This procedure is suitable for young children but not for near-mature patients or those with kyphosis.
5. Hemivertebra Resection or Wedge Osteotomy
These techniques are indicated for patients with rigid angular deformities. Better outcomes are achieved when performed before secondary curves develop into structural scoliosis.







