| disease | Infection of the Pterygomandibular Space |
Infection of the pterygomandibular space refers to acute suppurative infection in this area, with the main clinical manifestations being limited mouth opening and pain during chewing and swallowing.
bubble_chart Etiology
The pterygomandibular space is located between the medial bony wall of the mandibular ramus and the lateral surface of the medial pterygoid muscle. Its anterior boundary is formed by the temporalis muscle and buccinator muscle; the posterior boundary is the parotid gland sheath; the superior boundary is the lower margin of the lateral pterygoid muscle; and the inferior boundary is the attachment site of the medial pterygoid muscle to the mandibular ramus. This space is triangular in shape, with its base superior and apex inferior. Within this space, branches of the mandibular nerve exiting the skull through the foramen ovale at the cranial base, along with the inferior alveolar artery and vein, pass through. It communicates via loose connective tissue with adjacent spaces such as the infratemporal, temporal, buccal, submandibular, sublingual, parapharyngeal, and masseteric spaces. Through the cranial base vessels and nerves, it can also connect intracranially (Figure 3).
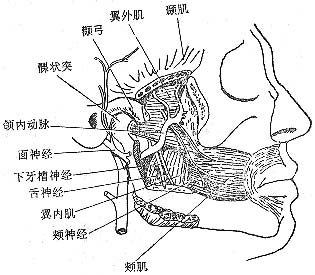
Figure 3 Anatomical location of the pterygomandibular space
Common causes include the spread of infection from pericoronitis of the mandibular wisdom tooth or periapical inflammation of the mandibular molars. Infection in the pterygomandibular space can also result from inadequate sterilization during inferior alveolar nerve block anesthesia. Additionally, infections from adjacent spaces, such as the infratemporal or parapharyngeal spaces, may spread to this area.
bubble_chart Clinical Manifestations
There is often a history of toothache first, followed by restricted mouth opening, pain when chewing food, and swallowing pain. Oral examination may reveal mucosal edema in the pterygomandibular fold, with grade I swelling and deep tenderness slightly medial to the posterior border of the mandibular ramus. Due to the deep location of the pterygomandibular space, even if an abscess has formed, it is difficult to clinically detect fluctuation directly. Puncture is often required for confirmation, which can lead to delayed diagnosis. As a result, the inflammation may spread to adjacent spaces, potentially forming infections in multiple spaces such as the infratemporal, parapharyngeal, submandibular, and retromandibular regions, complicating the condition.
bubble_chart Diagnosis1. Medical History: A history of acute pericoronitis of the mandibular wisdom tooth or a history of inferior alveolar nerve block anesthesia injection.
2. Clinical Manifestations: Significant redness, swelling, and tenderness in the pterygomandibular ligament area; obvious swelling and tenderness on the medial side of the mandibular angle and the medial side of the mandibular ramus; swelling below the zygomatic arch. The patient presents with fever and elevated white blood cell count.
Diagnosis can be confirmed by puncturing the lateral side of the pterygomandibular ligament and advancing along the medial side of the mandibular ramus into the space, or by aspirating pus from the posterior mandibular region into the space.
bubble_chart Treatment Measures
Incision and drainage of a pterygomandibular space abscess can be performed either intraorally or extraorally. The intraoral approach is less commonly adopted due to limitations in mouth opening, while the extraoral route offers advantages such as easier exposure of the space and postural drainage.
The intraoral incision is made slightly medial to the anterior border of the mandibular ramus, just lateral to the pterygomandibular fold, with a longitudinal incision of 2–3 cm. After blunt dissection of the buccinator muscle with a hemostat, the pterygomandibular space can be accessed along the medial side of the mandibular ramus (Figure 1).
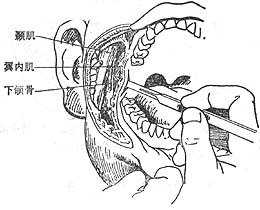
Figure 1 Intraoral incision and drainage route for pterygomandibular space abscess
The extraoral incision is similar to that for the masseteric space. When exposing the lower border of the mandibular angle, the medial attachment of the medial pterygoid muscle and the periosteum are partially incised. After separating the medial pterygoid muscle with a periosteal elevator, the space is entered to drain the pus. The abscess cavity is irrigated with saline or 1–3% hydrogen peroxide and packed with saline gauze. The dressing is changed the next day, and a rubber tube or strip is used for drainage (Figure 2).
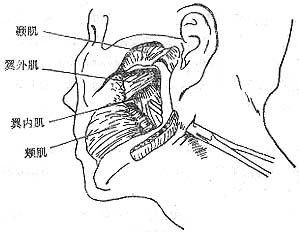
Figure 2 Extraoral incision and drainage route for pterygomandibular space abscess






